Meningitis pathophysiology
|
Meningitis Main Page |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Pathophysiology
The clinical picture of meningitis largely arises from the host response to the inciting organism in the CSF.
- It seems that the subcapsular components (the cell wall and lipopolysaccharide) of bacteria are more important in determining inflammation than the surface components (pili and polysaccharide capsule).
- The primary site of breakdown of the blood-brain barrier is the cerebral microvascular endothelium.
- Electron microscope (EM) studies have shown complete separation of the intercellular tight junctions
- It appears that there is a final common pathway, mediated by TNF-alpha, IL-1 and IL-6, that results in meningeal inflammation and loss of the blood-brain barrier.
- One of the major roles of these cytokines is to facilitate the migration of neutrophils across the vascular endothelium into the CSF.
- A key initial step in this process is obviously adhesion of the PMN to the endothelial surface.
- This is mediated by the expression of specific transmembrane glycoproteins expressed on the endothelial surface that interact with specific counterparts on the neutrophils.
- These adhesion molecules fall into three large categories: the immunoglobin superfamily (including the antigen-specific T and B cell receptors, ICAM-1 and ICAM-2), the integrin family (beta-1, beta-2, and beta-3) and the selectin family (including ELAM-1).
- The interaction of beta-2 integrin (CD18) and ICAM-1 is largely responsible for PMN diapedesis.
- Additionally, patients get cerebral edema that is mediated by an increase in capillary permeability, the inflammatory response from the neutrophils, and CSF outflow resistance.
- The above pathophysiologic processes are not only important in producing the symptoms associated with meningitis, but the understanding of the underlying disease process is necessary to guide therapy.
Mechanism
- In order to gain access to the CNS, the pathogen needs to colonize mucosal epithelium, invade and survive in the intravascular space, cross the blood-brain barrier and survive in the CSF.
- Colonization of the nasopharynx is usually asymptomatic, and during peak seasons, approximately 20% of the population are colonized with N. meningitidis.
Gross Pathology
Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
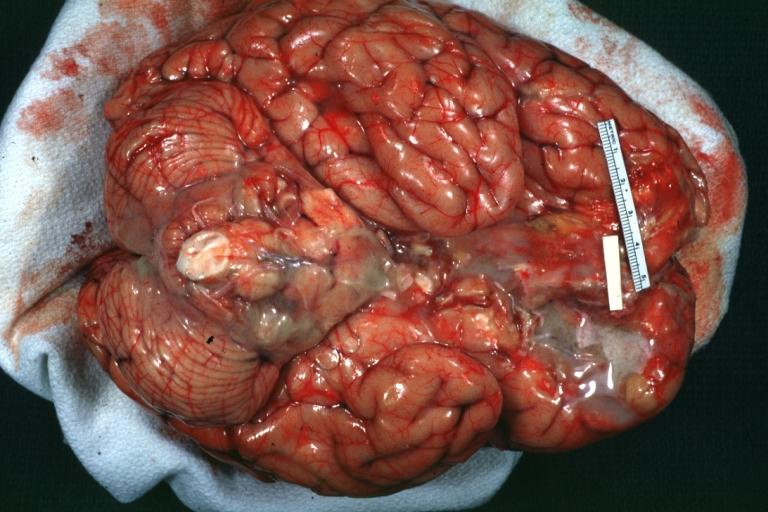
Meningitis: Gross, purulent leptomeningitis due to pneumococcus infection, an excellent example.
-
Bacterial Meningitis: Gross, basilar view
-
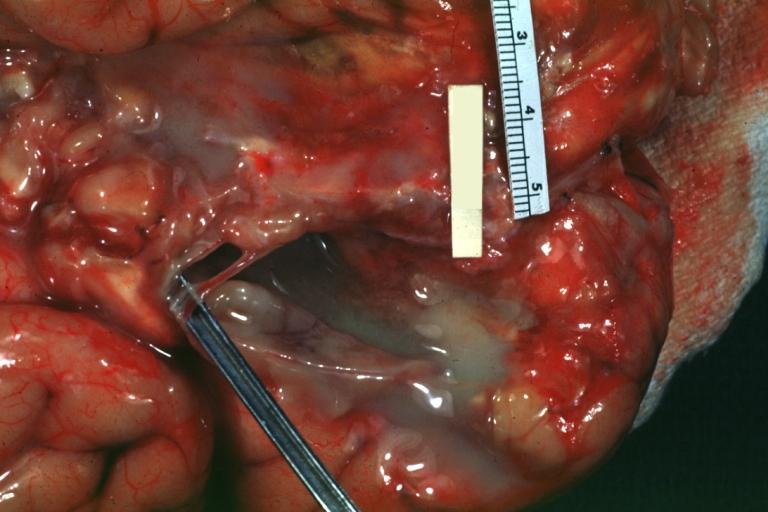
Bacterial Meningitis: Gross close-up
-
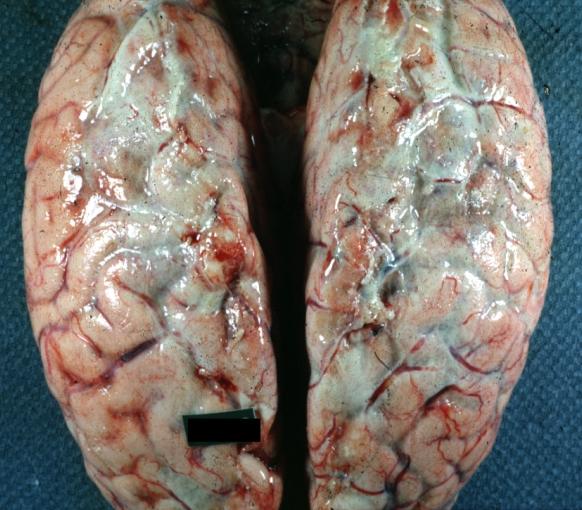
Meningitis: Gross base of frontal lobes well shown meningitis burn case with Pseudomonas sepsis
-
Meningitis: Gross natural color excellent demonstration of greenish pus in subarachnoid space
-
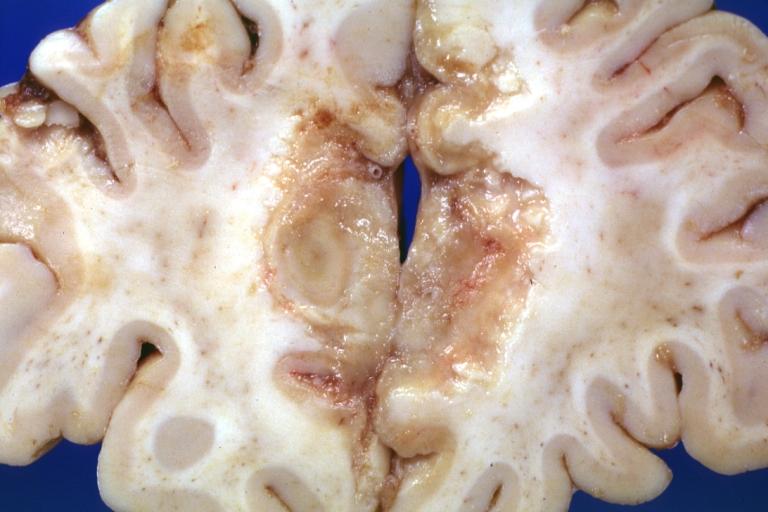
Tuberculous Meningitis: Gross fixed tissue close-up of large areas of necrosis in frontal parasagittal cortex secondary to tuberculous vasculitis. An excellent example
-
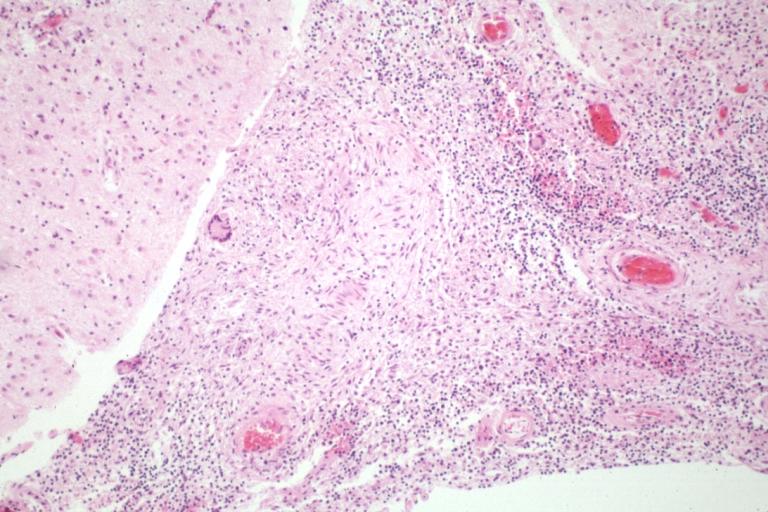
Tuberculous Meningitis: Micro low mag H&E. An excellent example with giant cells.
-
Purulent Meningitis: Gross natural color excellent photo lateral aspect of brain with easily seen purulent exudate due to Pneumococcus infection.
-
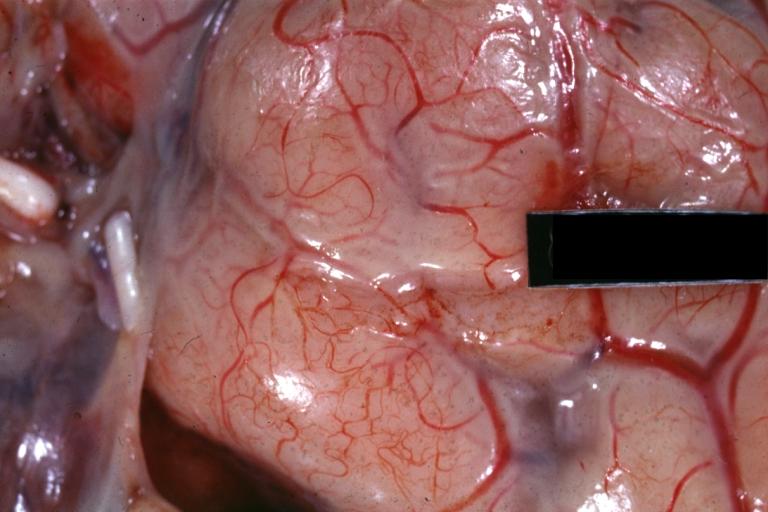
Purulent Meningitis: Gross natural color close-up view outstanding example of purulent exudate adjacent to blood vessels
-
Purulent Meningitis: Gross natural color Staphylococcal meningitis.
-
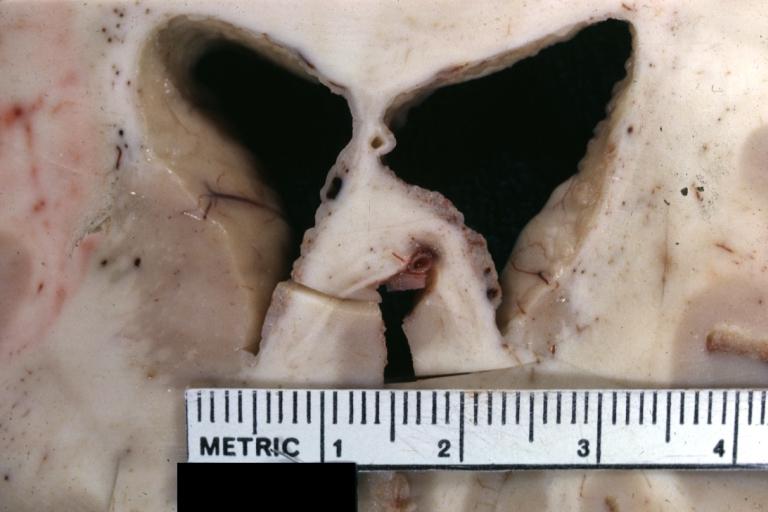
Ependymitis Granular Neoplastic: Gross fixed tissue close-up view and a spectacular one of this lesion case also has carcinomatous meningitis primary is lung oat cell.
-
Purulent Meningitis: Gross natural color brain in situ with removed calvarium very good illustration of exudate in meninges over convexities pneumococcus.
Microscopic Pathology
{{#ev:youtube|L9jpjxTSLws}}