Filgrastim
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]; Sree Teja Yelamanchili, MBBS [3]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Filgrastim is a human granulocyte colony-stimulating factor that is FDA approved for the treatment of cancer patients receiving myelosuppressive chemotherapy, patients with acute myeloid leukemiareceiving induction or consolidation chemotherapy, cancer patients receiving bone marrow transplant, patients undergoing peripheral blood progenitor cell collection and therapy, patients with severe chronic neutropenia. Common adverse reactions include bone pain.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Cancer Patients Receiving Myelosuppressive Chemotherapy
- Dosing information
- Recommended starting dosage: 5 mcg/kg/day‚ administered as a single daily injection by SC bolus injection‚ by short IV infusion (15 to 30 minutes)‚ or by continuous SC or continuous IV infusion.
- A CBC and platelet count should be obtained before instituting Filgrastim therapy and monitored twice weekly during therapy.
- Doses may be increased in increments of 5 mcg/kg for each chemotherapy cycle‚ according to the duration and severity of the ANC nadir.
- Filgrastim should be administered no earlier than 24 hours after the administration of cytotoxic chemotherapy.
- Filgrastim should not be administered in the period 24 hours before the administration of chemotherapy.
- Filgrastim should be administered daily for up to 2 weeks‚ until the ANC has reached 10‚000/mm3 following the expected chemotherapy-induced neutrophil nadir.
- The duration of Filgrastim therapy needed to attenuate chemotherapy-induced neutropenia may be dependent on the myelosuppressive potential of the chemotherapy regimen employed.
- Filgrastim therapy should be discontinued if the ANC surpasses 10‚000/mm3 after the expected chemotherapy-induced neutrophil nadir.
Cancer Patients Receiving Bone Marrow Transplant
- Dosing information
- Recommended dosage following BMT: 10 mcg/kg/day given as an IV infusion of 4 or 24 hours‚ or as a continuous 24-hour SC infusion. For patients receiving BMT‚ the first dose of Filgrastim should be administered at least 24 hours after cytotoxic chemotherapy and at least 24 hours after bone marrow infusion.
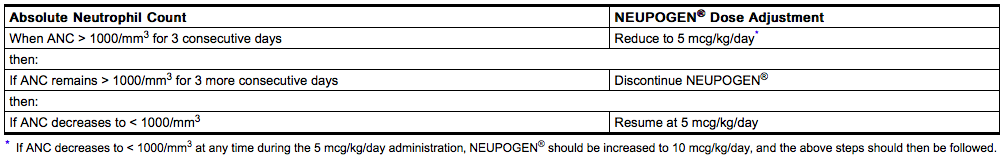
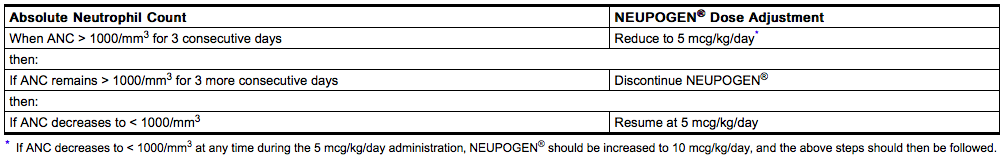
During the period of neutrophil recovery‚ the daily dose of Filgrastim should be titrated against the neutrophil response as follows:
Peripheral Blood Progenitor Cell Collection and Therapy in Cancer Patients
- Dosing information
- Recommended dosage for the mobilization of PBPC: 10 mcg/kg/day SC‚ either as a bolus or a continuous infusion. It is recommended that Filgrastim be given for at least 4 days before the first leukapheresis procedure and continued until the last leukapheresis. Although the optimal duration of Filgrastim administration and leukapheresis schedule have not been established‚ administration of Filgrastim for 6 to 7 days with leukapheresis on days 5‚ 6‚ and 7 was found to be safe and effective. Neutrophil counts should be monitored after 4 days of Filgrastim, and Filgrastim dose modification should be considered for those patients who develop a WBC count > 100‚000/mm3.
In all clinical trials of Filgrastim for the mobilization of PBPC‚ Filgrastim was also administered after reinfusion of the collected cells.
Patients With Severe Chronic Neutropenia
- Dosing information
- Filgrastim should be administered to those patients in whom a diagnosis of congenital‚ cyclic‚ or idiopathic neutropenia has been definitively confirmed. Other diseases associated with neutropenia should be ruled out.
- Starting Dose:
- Congenital neutropenia: The recommended daily starting dose is 6 mcg/kg BID SC .
- Idiopathic or Cyclic Neutropenia: The recommended daily starting dose is 5 mcg/kg injection SC qd.
- Dose Adjustments:
- Chronic daily administration is required to maintain clinical benefit. Absolute neutrophil count should not be used as the sole indication of efficacy. The dose should be individually adjusted based on the patient's clinical course as well as ANC. In the SCN postmarketing surveillance study, the reported median daily doses of Filgrastim were: 6.0 mcg/kg (congenital neutropenia), 2.1 mcg/kg (cyclic neutropenia), and 1.2 mcg/kg (idiopathic neutropenia). In rare instances, patients with congenital neutropenia have required doses of Filgrastim ≥ 100 mcg/kg/day.
Dilution
If required‚ Filgrastim may be diluted in 5% dextrose. Filgrastim diluted to concentrations between 5 and 15 mcg/mL should be protected from adsorption to plastic materials by the addition of Albumin (Human) to a final concentration of 2 mg/mL. When diluted in 5% dextrose or 5% dextrose plus Albumin (Human)‚ Filgrastim is compatible with glass bottles‚ PVC and polyolefin IV bags‚ and polypropylene syringes. Dilution of Filgrastim to a final concentration of less than 5 mcg/mL is not recommended at any time. Do not dilute with saline at any time; product may precipitate.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Myelodysplastic syndrome
- Developed by: American Society of Clinical Oncology (ASCO)
- Class of Recommendation: Not applicable
- Level of Evidence: Not applicable
- Dosing Information
- Intermittent CSF use may be considered in patients with severe neutropenia and recurrent infections.
Cancer Patients Receiving Myelosuppressive Chemotherapy
- Dosing information
- Recommended starting dosage: 5 mcg/kg/day‚ administered as a single daily injection by SC bolus injection‚ by short IV infusion (15 to 30 minutes)‚ or by continuous SC or continuous IV infusion.
- A CBC and platelet count should be obtained before instituting Filgrastim therapy and monitored twice weekly during therapy.
- Doses may be increased in increments of 5 mcg/kg for each chemotherapy cycle‚ according to the duration and severity of the ANC nadir.
- Filgrastim should be administered no earlier than 24 hours after the administration of cytotoxic chemotherapy.
- Filgrastim should not be administered in the period 24 hours before the administration of chemotherapy.
- Filgrastim should be administered daily for up to 2 weeks‚ until the ANC has reached 10‚000/mm3 following the expected chemotherapy-induced neutrophil nadir.
- The duration of Filgrastim therapy needed to attenuate chemotherapy-induced neutropenia may be dependent on the myelosuppressive potential of the chemotherapy regimen employed.
- Filgrastim therapy should be discontinued if the ANC surpasses 10‚000/mm3 after the expected chemotherapy-induced neutrophil nadir.
Non–Guideline-Supported Use
Agranulocytosis
- Dosing information
- Dosing information
- 20 milligrams/kilogram/day (mg/kg/day)
Disorder related to renal transplantation - Neutropenic disorder
- Dosing information
- 6 micrograms/kilogram/day subcutaneously [4]
- Dosing information
- 100mcg/m(2) to 400 mcg/m(2) [5]
Infectious disease
- Dosing information
- 300 micrograms/day (mcg/day) subcutaneously to 480 mcg/day[6]
- Dosing information
- 5 micrograms/kilogram/day[7]
Mucositis following chemotherapy
- Dosing information
- 120 mcg (0.4 mL)[8]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Cancer Patients Receiving Myelosuppressive Chemotherapy
- Dosing information
- Recommended starting dosage: 5 mcg/kg/day‚ administered as a single daily injection by SC bolus injection‚ by short IV infusion (15 to 30 minutes)‚ or by continuous SC or continuous IV infusion.
- A CBC and platelet count should be obtained before instituting Filgrastim therapy and monitored twice weekly during therapy.
- Doses may be increased in increments of 5 mcg/kg for each chemotherapy cycle‚ according to the duration and severity of the ANC nadir.
- Filgrastim should be administered no earlier than 24 hours after the administration of cytotoxic chemotherapy.
- Filgrastim should not be administered in the period 24 hours before the administration of chemotherapy.
- Filgrastim should be administered daily for up to 2 weeks‚ until the ANC has reached 10‚000/mm3 following the expected chemotherapy-induced neutrophil nadir.
- The duration of Filgrastim therapy needed to attenuate chemotherapy-induced neutropenia may be dependent on the myelosuppressive potential of the chemotherapy regimen employed.
- Filgrastim therapy should be discontinued if the ANC surpasses 10‚000/mm3 after the expected chemotherapy-induced neutrophil nadir.
Cancer Patients Receiving Bone Marrow Transplant
- Dosing information
- Recommended dosage following BMT: 10 mcg/kg/day given as an IV infusion of 4 or 24 hours‚ or as a continuous 24-hour SC infusion. For patients receiving BMT‚ the first dose of Filgrastim should be administered at least 24 hours after cytotoxic chemotherapy and at least 24 hours after bone marrow infusion.
During the period of neutrophil recovery‚ the daily dose of Filgrastim should be titrated against the neutrophil response as follows:
Peripheral Blood Progenitor Cell Collection and Therapy in Cancer Patients
- Dosing information
- Recommended dosage for the mobilization of PBPC: 10 mcg/kg/day SC‚ either as a bolus or a continuous infusion. It is recommended that Filgrastim be given for at least 4 days before the first leukapheresis procedure and continued until the last leukapheresis. Although the optimal duration of Filgrastim administration and leukapheresis schedule have not been established‚ administration of Filgrastim for 6 to 7 days with leukapheresis on days 5‚ 6‚ and 7 was found to be safe and effective. Neutrophil counts should be monitored after 4 days of Filgrastim, and Filgrastim dose modification should be considered for those patients who develop a WBC count > 100‚000/mm3.
In all clinical trials of Filgrastim for the mobilization of PBPC‚ Filgrastim was also administered after reinfusion of the collected cells.
Patients With Severe Chronic Neutropenia
- Dosing information
- Filgrastim should be administered to those patients in whom a diagnosis of congenital‚ cyclic neutropenia‚ or idiopathic neutropenia has been definitively confirmed. Other diseases associated with neutropenia should be ruled out.
- Starting Dose:
- congenital neutropenia: The recommended daily starting dose is 6 mcg/kg BID SC every day.
- Idiopathic or Cyclic Neutropenia: The recommended daily starting dose is 5 mcg/kg injection SC qd.
- Dose Adjustments:
- Chronic daily administration is required to maintain clinical benefit. Absolute neutrophil count should not be used as the sole indication of efficacy. The dose should be individually adjusted based on the patient's clinical course as well as ANC. In the SCN postmarketing surveillance study, the reported median daily doses of Filgrastim were: 6.0 mcg/kg (congenital neutropenia), 2.1 mcg/kg (cyclic neutropenia), and 1.2 mcg/kg (idiopathic neutropenia). In rare instances, patients with congenital neutropenia have required doses of Filgrastim ≥ 100 mcg/kg/day.
Dilution
If required‚ Filgrastim may be diluted in 5% dextrose. Filgrastim diluted to concentrations between 5 and 15 mcg/mL should be protected from adsorption to plastic materials by the addition of Albumin (Human) to a final concentration of 2 mg/mL. When diluted in 5% dextrose or 5% dextrose plus Albumin (Human)‚ Filgrastim is compatible with glass bottles‚ PVC and polyolefin IV bags‚ and polypropylene syringes. Dilution of Filgrastim to a final concentration of less than 5 mcg/mL is not recommended at any time. Do not dilute with saline at any time; product may precipitate.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Filgrastim in pediatric patients.
Non–Guideline-Supported Use
Aplastic anemia
- Dosing information
- Not applicable [9]
Neutropenia - Pre-eclampsia
- Dosing information
- 5 or 10 micrograms/kilogram (mcg/kg)/day[10]
Septicemia of newborn
- Dosing information
- Not applicable [11]
Shwachman syndrome
- Dosing information
- Not applicable [12]
Contraindications
Filgrastim is contraindicated in patients with known hypersensitivity to E coli-derived proteins‚ filgrastim‚ or any component of the product.
Warnings
Allergic Reactions
Allergic-type reactions occurring on initial or subsequent treatment have been reported in < 1 in 4000 patients treated with Filgrastim. These have generally been characterized by systemic symptoms involving at least two body systems‚ most often skin (rash‚ urticaria‚ facial edema)‚ respiratory (wheezing‚ dyspnea)‚ and cardiovascular (hypotension‚ tachycardia). Some reactions occurred on initial exposure. Reactions tended to occur within the first 30 minutes after administration and appeared to occur more frequently in patients receiving Filgrastim IV. Rapid resolution of symptoms occurred in most cases after administration of antihistamines‚ steroids‚ bronchodilators‚ and/or epinephrine. Symptoms recurred in more than half the patients who were rechallenged.
Splenic Rupture
Splenic Rupture, including fatal cases, has been reported following the admistration of Filgrastim. Individuals taking Filgrastim who report left upper abdominal pain and/or shoulder tip pain should be evaluated for an enlarged spleen or splenic rupture.
Acute Respiratory Distress Syndrome (ARDS)
Acute respiratory distress syndrome (ARDS) has been reported in patients receiving Filgrastim, and is postulated to be secondary to an influx of neutrophils to sites of inflammation in the lungs. Patients receiving Filgrastim who develop fever, lung infiltrates, or respiratory distress should be evaluated for the possibility of ARDS. In the event that ARDS occurs, Filgrastim should be withheld until resolution of ARDS or discontinued. Patients should receive appropriate medical management for this condition.
Alveolar Hemorrhage and hemoptysis
Alveolar hemorrhage manifesting as pulmonary infiltrates and hemoptysis requiring hospitalization has been reported in healthy donors undergoing PBPC mobilization. Hemoptysis resolved with discontinuation of Filgrastim. The use of Filgrastim for PBPC mobilization in healthy donors is not an approved indication.
Sickle cell disorders
Severe sickle cell crises, in some cases resulting in death, have been associated with the use of Filgrastim in patients with sickle cell disorders. Only physicians qualified by specialized training or experience in the treatment of patients with sickle cell disorders should prescribe Filgrastim for such patients, and only after careful consideration of the potential risks and benefits.
Patients With Severe Chronic Neutropenia
The safety and efficacy of Filgrastim in the treatment of neutropenia due to other hematopoietic disorders (eg‚ myelodysplastic syndrome [MDS]) have not been established. Care should be taken to confirm the diagnosis of SCN before initiating Filgrastim therapy. MDS and AML have been reported to occur in the natural history of congenital neutropenia without cytokine therapy. 17 cytogenetic abnormalities, transformation to MDS, and AML have also been observed in patients treated with Filgrastim for SCN. Based on available data including a postmarketing surveillance study, the risk of developing MDS and AML appears to be confined to the subset of patients with congenital neutropenia. Abnormal cytogenetics and MDS have been associated with the eventual development of myeloid leukemia. The effect of Filgrastim on the development of abnormal cytogenetics and the effect of continued Filgrastim administration in patients with abnormal cytogenetics or MDS are unknown. If a patient with SCN develops abnormal cytogenetics or myelodysplasia‚ the risks and benefits of continuing Filgrastim should be carefully considered.
PRECAUTIONS
General
Simultaneous Use With Chemotherapy and Radiation Therapy
The safety and efficacy of Filgrastim given simultaneously with cytotoxic chemotherapy have not been established. Because of the potential sensitivity of rapidly dividing myeloid cells to cytotoxic chemotherapy‚ do not use Filgrastim in the period 24 hours before through 24 hours after the administration of cytotoxic chemotherapy. The efficacy of Filgrastim has not been evaluated in patients receiving chemotherapy associated with delayed myelosuppression, with mitomycin C, or with myelosuppressive doses of antimetabolites such as 5-fluorouracil. The safety and efficacy of Filgrastim have not been evaluated in patients receiving concurrent radiation therapy. Simultaneous use of Filgrastim with chemotherapy and radiation therapy should be avoided.
Potential Effect on Malignant Cells
Filgrastim is a growth factor that primarily stimulates neutrophils. However‚ the possibility that Filgrastim can act as a growth factor for any tumor type cannot be excluded. In a randomized study evaluating the effects of Filgrastim versus placebo in patients undergoing remission induction for AML, there was no significant difference in remission rate, disease-free, or overall survival. The safety of Filgrastim in chronic myeloid leukemia (CML) and myelodysplasia has not been established. When Filgrastim is used to mobilize PBPC‚ tumor cells may be released from the marrow and subsequently collected in the leukapheresis product. The effect of reinfusion of tumor cells has not been well studied‚ and the limited data available are inconclusive.
Leukocytosis
Cancer Patients Receiving Myelosuppressive Chemotherapy
White blood cell counts of 100‚000/mm3 or greater were observed in approximately 2% of patients receiving Filgrastim at doses above 5 mcg/kg/day. There were no reports of adverse events associated with this degree of leukocytosis. In order to avoid the potential complications of excessive leukocytosis‚ a CBC is recommended twice per week during Filgrastim therapy.
Premature Discontinuation of Filgrastim Therapy
Cancer Patients Receiving Myelosuppressive Chemotherapy
A transient increase in neutrophil counts is typically seen 1 to 2 days after initiation of Filgrastim therapy. However‚ for a sustained therapeutic response‚ Filgrastim therapy should be continued following chemotherapy until the post-nadir ANC reaches 10‚000/mm3. Therefore‚ the premature discontinuation of Filgrastim therapy‚ prior to the time of recovery from the expected neutrophil nadir‚ is generally not recommended.
Immunogenicity
- As with all therapeutic proteins, there is a potential for immunogenicity. *The incidence of antibody development in patients receiving Filgrastim has not been adequately determined.
- While available data suggest that a small proportion of patients developed binding antibodies to filgrastim, the nature and specificity of these antibodies has not been adequately studied.
- In clinical studies comparing Filgrastim and Neulasta®, the incidence of antibodies binding to Filgrastim was 3% (11/333).
- In these 11 patients, no evidence of a neutralizing response was observed using a cell-based bioassay.
- The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay, and the observed incidence of antibody positivity in an assay may be influenced by several factors including timing of sampling, sample handling, concomitant medications, and underlying disease.
- Therefore, comparison of the incidence of antibodies to Filgrastim with the incidence of antibodies to other products may be misleading.
- Cytopenias resulting from an antibody response to exogenous growth factors have been reported on rare occasions in patients treated with other recombinant growth factors.
- There is a theoretical possibility that an antibody directed against filgrastim may cross-react with endogenous G-CSF, resulting in immune-mediated neutropenia; however, this has not been reported in clinical studies or in post-marketing experience.
- Patients who develop hypersensitivity to Filgrastim may have allergic or hypersensitivity reactions to other E coli-derived proteins.
Cutaneous Vasculitis
Cutaneous vasculitis has been reported in patients treated with Filgrastim. In most cases‚ the severity of cutaneous vasculitis was moderate or severe. Most of the reports involved patients with SCN receiving long-term Filgrastim therapy. Symptoms of vasculitis generally developed simultaneously with an increase in the ANC and abated when the ANC decreased. Many patients were able to continue Filgrastim at a reduced dose.
Thrombocytopenia
Thrombocytopenia has been reported in patients receiving Filgrastim. Platelet counts should be monitored closely.
Information for Patients and Caregivers
Patients should be referred to the “Information for Patients and Caregivers” labeling included with the package insert in each dispensing pack of Filgrastim vials or Filgrastim prefilled syringes. The “Information for Patients and Caregivers” labeling provides information about neutrophils and neutropenia and the safety and efficacy of Filgrastim. It is not intended to be a disclosure of all known or possible effects.
Laboratory Monitoring
Cancer Patients Receiving Myelosuppressive Chemotherapy
A CBC and platelet count should be obtained prior to chemotherapy‚ and at regular intervals (twice per week) during Filgrastim therapy. Following cytotoxic chemotherapy‚ the neutrophil nadir occurred earlier during cycles when Filgrastim was administered‚ and WBC differentials demonstrated a left shift‚ including the appearance of promyelocytes and myeloblasts. In addition‚ the duration of severe neutropenia was reduced and was followed by an accelerated recovery in the neutrophil counts.
Cancer Patients Receiving Bone Marrow Transplant
Frequent CBCs and platelet counts are recommended (at least 3 times per week) following marrow transplantation.
Patients With Severe Chronic Neutropenia
During the initial 4 weeks of Filgrastim therapy and during the 2 weeks following any dose adjustment‚ a CBC with differential and platelet count should be performed twice weekly. Once a patient is clinically stable‚ a CBC with differential and platelet count should be performed monthly during the first year of treatment. Thereafter, if clinically stable, routine monitoring with regular CBCs (i.e., as clinically indicated but at least quarterly) is recommended. Additionally, for those patients with congenital neutropenia, annual bone marrow and cytogenetic evaluations should be performed throughout the duration of treatment. In clinical trials‚ the following laboratory results were observed:
- Cyclic fluctuations in the neutrophil counts were frequently observed in patients with congenital or idiopathic neutropenia after initiation of Filgrastim therapy.
- Platelet counts were generally at the upper limits of normal prior to Filgrastim therapy. With Filgrastim therapy‚ platelet counts decreased but usually remained within normal limits.
- Early myeloid forms were noted in peripheral blood in most patients‚ including the appearance of metamyelocytes and myelocytes.
- Promyelocytes and myeloblasts were noted in some patients.
- Relative increases were occasionally noted in the number of circulating eosinophils and basophils. No consistent increases were observed with Filgrastim therapy.
- As in other trials‚ increases were observed in serum uric acid‚ lactic dehydrogenase‚ and serum alkaline phosphatase.
Adverse Reactions
Clinical Trials Experience
Clinical Trial Experience
Cancer Patients Receiving Myelosuppressive Chemotherapy
- In clinical trials involving over 350 patients receiving Filgrastim following nonmyeloablative cytotoxic chemotherapy‚ most adverse experiences were the sequelae of the underlying malignancy or cytotoxic chemotherapy.
- In all phase 2 and 3 trials‚ medullary bone pain‚ reported in 24% of patients‚ was the only consistently observed adverse reaction attributed to Filgrastim therapy.
- This bone pain was generally reported to be of mild-to-moderate severity‚ and could be controlled in most patients with non-narcotic analgesics; infrequently‚ bone pain was severe enough to require narcotic analgesics. *Bone pain was reported more frequently in patients treated with higher doses (20 to 100 mcg/kg/day) administered IV‚ and less frequently in patients treated with lower SC doses of Filgrastim (3 to 10 mcg/kg/day).
- In the randomized‚ double-blind‚ placebo-controlled trial of Filgrastim therapy following combination chemotherapy in patients (n = 207) with small cell lung cancer‚ the following adverse events were reported during blinded cycles of study medication (placebo or Filgrastim at 4 to 8 mcg/kg/day). *Events are reported as exposure-adjusted since patients remained on double-blind Filgrastim a median of 3 cycles versus 1 cycle for placebo.

- In this study‚ there were no serious‚ life-threatening‚ or fatal adverse reactions attributed to Filgrastim therapy.
- Specifically‚ there were no reports of flu-like symptoms‚ pleuritis‚ pericarditis‚ or other major systemic reactions to Filgrastim.
- Spontaneously reversible elevations in uric acid‚ lactate dehydrogenase‚ and alkaline phosphatase occurred in 27% to 58% of 98 patients receiving blinded Filgrastim therapy following cytotoxic chemotherapy; increases were generally mild-to-moderate.
- Transient decreases in blood pressure (< 90/60 mmHg)‚ which did not require clinical treatment‚ were reported in 7 of 176 patients in phase 3 clinical studies following administration of Filgrastim.
- Cardiac events (myocardial infarctions‚ arrhythmias) have been reported in 11 of 375 cancer patients receiving Filgrastim in clinical studies; the relationship to Filgrastim therapy is unknown.
- No evidence of interaction of Filgrastim with other drugs was observed in the course of clinical trials.
- There has been no evidence for the development of antibodies or of a blunted or diminished response to Filgrastim in treated patients‚ including those receiving Filgrastim daily for almost 2 years.
Patients With Acute myeloid leukemia
In a randomized phase 3 clinical trial, 259 patients received Filgrastim and 262 patients received placebo postchemotherapy. Overall, the frequency of all reported adverse events was similar in both the Filgrastim and placebo groups (83% vs 82% in Induction 1; 61% vs 64% in Consolidation 1). Adverse events reported more frequently in the Filgrastim-treated group included: petechiae (17% vs 14%), epistaxis (9% vs 5%), and transfusion reactions (10% vs 5%). There were no significant differences in the frequency of these events. There were a similar number of deaths in each treatment group during induction (25 Filgrastim vs 27 placebo). The primary causes of death included infection (9 vs 18), persistent leukemia (7 vs 5), and hemorrhage (6 vs 3). Of the hemorrhagic deaths, 5 cerebral hemorrhages were reported in the Filgrastim group and 1 in the placebo group. Other serious nonfatal hemorrhagic events were reported in the respiratory tract (4 vs 1), skin (4 vs 4), gastrointestinal tract (2 vs 2), urinary tract (1 vs 1), ocular (1 vs 0), and other nonspecific sites (2 vs 1). While 19 (7%) patients in the Filgrastim group and 5 (2%) patients in the placebo group experienced severe or fatal hemorrhagic events, overall, hemorrhagic adverse events were reported at a similar frequency in both groups (40% vs 38%). The time to transfusion-independent platelet recovery and the number of days of platelet transfusions were similar in both groups.
Cancer Patients Receiving Bone Marrow Transplant
In clinical trials‚ the reported adverse effects were those typically seen in patients receiving intensive chemotherapy followed by BMT. The most common events reported in both control and treatment groups included stomatitis, nausea, and vomiting‚ generally of mild-to-moderate severity and were considered unrelated to Filgrastim. In the randomized studies of BMT involving 167 patients who received study drug‚ the following events occurred more frequently in patients treated with filgrastim than in controls: nausea (10% vs 4%)‚ vomiting (7% vs 3%)‚ hypertension (4% vs 0%)‚ rash (12% vs 10%)‚ and peritonitis (2% vs 0%). None of these events were reported by the investigator to be related to Filgrastim. One event of erythema nodosum was reported moderate in severity and possibly related to Filgrastim. Generally‚ adverse events observed in nonrandomized studies were similar to those seen in randomized studies‚ occurred in a minority of patients and were of mild-to-moderate severity. In one study (n = 45)‚ 3 serious adverse events reported by the investigator were considered possibly related to Filgrastim. These included 2 events of renal insufficiency and 1 event of capillary leak syndrome. The relationship of these events to Filgrastim remains unclear since they occurred in patients with culture-proven infection with clinical sepsis who were receiving potentially nephrotoxic antibacterial and antifungal therapy.
Cancer Patients Undergoing Peripheral Blood Progenitor Cell Collection and Therapy
In clinical trials‚ 126 patients received Filgrastim for PBPC mobilization. In this setting‚ Filgrastim was generally well tolerated. Adverse events related to Filgrastim consisted primarily of mild-to-moderate musculoskeletal symptoms‚ reported in 44% of patients. These symptoms were predominantly events of medullary bone pain (33%). Headache was reported related to Filgrastim in 7% of patients. Transient increases in alkaline phosphatase related to Filgrastim were reported in 21% of the patients who had serum chemistries measured; most were mild-to-moderate. All patients had increases in neutrophil counts during mobilization‚ consistent with the biological effects of Filgrastim. Two patients had a WBC count > 100‚000/mm3. No sequelae were associated with any grade of leukocytosis. Sixty-five percent of patients had mild-to-moderate anemia and 97% of patients had decreases in platelet counts; 5 patients (out of 126) had decreased platelet counts to < 50‚000/mm3. Anemia and thrombocytopenia have been reported to be related to leukapheresis; however‚ the possibility that Filgrastim mobilization may contribute to anemia or thrombocytopenia has not been ruled out.
Patients With Severe Chronic Neutropenia
Mild-to-moderate bone pain was reported in approximately 33% of patients in clinical trials. This symptom was readily controlled with non-narcotic analgesics. Generalized musculoskeletal pain was also noted in higher frequency in patients treated with Filgrastim. Palpable splenomegaly was observed in approximately 30% of patients. Abdominal or flank pain was seen infrequently, and thrombocytopenia (< 50‚000/mm3) was noted in 12% of patients with palpable spleens. Fewer than 3% of all patients underwent splenectomy‚ and most of these had a prestudy history of splenomegaly. Fewer than 6% of patients had thrombocytopenia (< 50‚000/mm3) during Filgrastim therapy‚ most of whom had a pre-existing history of thrombocytopenia. In most cases‚ thrombocytopenia was managed by Filgrastim dose reduction or interruption. An additional 5% of patients had platelet counts between 50‚000 and 100‚000/mm3. There were no associated serious hemorrhagic sequelae in these patients. Epistaxis was noted in 15% of patients treated with Filgrastim, but was associated with thrombocytopenia in 2% of patients. Anemia was reported in approximately 10% of patients‚ but in most cases appeared to be related to frequent diagnostic phlebotomy‚ chronic illness, or concomitant medications. Other adverse events infrequently observed and possibly related to Filgrastim therapy were: injection site reaction‚ rash‚ hepatomegaly‚ arthralgia‚ osteoporosis‚ cutaneous vasculitis‚ hematuria/proteinuria‚ alopecia‚ and exacerbation of some pre-existing skin disorders (e.g.‚ psoriasis). Cytogenetic abnormalities, transformation to MDS, and AML have been observed in patients treated with Filgrastim for SCN. As of 31 December 1997, data were available from a postmarketing surveillance study of 531 SCN patients with an average follow-up of 4.0 years. Based on analysis of these data, the risk of developing MDS and AML appears to be confined to the subset of patients with congenital neutropenia. A life-table analysis of these data revealed that the cumulative risk of developing leukemia or MDS by the end of the 8th year of Filgrastim treatment in a patient with congenital neutropenia was 16.5% (95% C.I. = 9.8%, 23.3%); this represents an annual rate of approximately 2%. Cytogenetic abnormalities, most commonly involving chromosome 7, have been reported in patients treated with Filgrastim who had previously documented normal cytogenetics. It is unknown whether the development of cytogenetic abnormalities, MDS, or AML is related to chronic daily Filgrastim administration or to the natural history of congenital neutropenia. It is also unknown if the rate of conversion in patients who have not received Filgrastim is different from that of patients who have received Filgrastim. Routine monitoring through regular CBCs is recommended for all SCN patients. Additionally, annual bone marrow and cytogenetic evaluations are recommended in all patients with congenital neutropenia.
Postmarketing Experience
The following adverse reactions have been identified during postapproval of Filgrastim. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- splenic rupture and splenomegaly (enlarged spleen)
- acute respiratory distress syndrome (ARDS)
- alveolar hemorrhage and hemoptysis
- sickle cell crisis
- cutaneous vasculitis
- Sweet’s syndrome
- decreased bone density and osteoporosis in pediatric SCN patients receiving chronic treatment with Filgrastim
Drug Interactions
Drug interactions between Filgrastim and other drugs have not been fully evaluated. Drugs which may potentiate the release of neutrophils‚ such as lithium‚ should be used with caution. Increased hematopoietic activity of the bone marrow in response to growth factor therapy has been associated with transient positive bone-imaging changes. This should be considered when interpreting bone-imaging results.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): C
Filgrastim has been shown to have adverse effects in pregnant rabbits when given in doses 2 to 10 times the human dose. Since there are no adequate and well-controlled studies in pregnant women, the effect, if any, of Filgrastim on the developing fetus or the reproductive capacity of the mother is unknown. However, the scientific literature describes transplacental passage of Filgrastim when administered to pregnant rats during the latter part of gestation18 and apparent transplacental passage of Filgrastim when administered to pregnant humans by ≤ 30 hours prior to preterm delivery (≤ 30 weeks gestation).19 Filgrastim should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
In rabbits‚ increased abortion and embryolethality were observed in animals treated with Filgrastim at 80 mcg/kg/day. Filgrastim administered to pregnant rabbits at doses of 80 mcg/kg/day during the period of organogenesis was associated with increased fetal resorption‚ genitourinary bleeding‚ developmental abnormalities‚ decreased body weight‚ live births‚ and food consumption. External abnormalities were not observed in the fetuses of dams treated at 80 mcg/kg/day. Reproductive studies in pregnant rats have shown that Filgrastim was not associated with lethal‚ teratogenic‚ or behavioral effects on fetuses when administered by daily IV injection during the period of organogenesis at dose levels up to 575 mcg/kg/day.
In Segment III studies in rats‚ offspring of dams treated at > 20 mcg/kg/day exhibited a delay in external differentiation (detachment of auricles and descent of testes) and slight growth retardation‚ possibly due to lower body weight of females during rearing and nursing. Offspring of dams treated at 100 mcg/kg/day exhibited decreased body weights at birth‚ and a slightly reduced 4-day survival rate.
Encourage women who become pregnant during Filgrastim treatment to enroll in Amgen’s Pregnancy Surveillance Program. Patients or their physicians should call 1-800-77-AMGEN (1-800-772-6436) to enroll.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Filgrastim in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Filgrastim during labor and delivery.
Nursing Mothers
It is not known whether Filgrastim is excreted in human milk. Because many drugs are excreted in human milk‚ caution should be exercised if Filgrastim is administered to a nursing woman. Encourage women who are nursing during Filgrastim treatment to enroll in Amgen’s Lactation Surveillance Program. Patients or their physicians should call 1‑800‑77‑AMGEN (1-800-772-6436) to enroll.
Pediatric Use
In a phase 3 study to assess the safety and efficacy of Filgrastim in the treatment of SCN, 120 patients with a median age of 12 years were studied. Of the 120 patients, 12 were infants (1 month to 2 years of age), 47 were children (2 to 12 years of age), and 9 were adolescents (12 to 16 years of age). Additional information is available from a SCN postmarketing surveillance study, which includes long-term follow-up of patients in the clinical studies and information from additional patients who entered directly into the postmarketing surveillance study. Of the 531 patients in the surveillance study as of 31 December 1997, 32 were infants, 200 were children, and 68 were adolescents (see CLINICAL EXPERIENCE, INDICATIONS AND USAGE, LABORATORY MONITORING, and DOSAGE AND ADMINISTRATION). Pediatric patients with congenital types of neutropenia (Kostmann’s syndrome, congenital agranulocytosis, or Schwachman-Diamond syndrome) have developed cytogenetic abnormalities and have undergone transformation to MDS and AML while receiving chronic Filgrastim treatment. The relationship of these events to Filgrastim administration is unknown (see WARNINGS and ADVERSE REACTIONS). Long-term follow-up data from the postmarketing surveillance study suggest that height and weight are not adversely affected in patients who received up to 5 years of Filgrastim treatment. Limited data from patients who were followed in the phase 3 study for 1.5 years did not suggest alterations in sexual maturation or endocrine function. The safety and efficacy in neonates and patients with autoimmune neutropenia of infancy have not been established. In the cancer setting‚ 12 pediatric patients with neuroblastoma have received up to 6 cycles of cyclophosphamide‚ cisplatin‚ doxorubicin‚ and etoposide chemotherapy concurrently with Filgrastim; in this population‚ Filgrastim was well tolerated. There was one report of palpable splenomegaly associated with Filgrastim therapy; however‚ the only consistently reported adverse event was musculoskeletal pain‚ which is no different from the experience in the adult population.
Geriatic Use
Among 855 subjects enrolled in 3 randomized, placebo-controlled trials of Filgrastim use following myelosuppressive chemotherapy, there were 232 subjects age 65 or older, and 22 subjects age 75 or older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other clinical experience has not identified differences in the responses between elderly and younger patients. Clinical studies of Filgrastim in other approved indications (ie, bone marrow transplant (BMT) recipients, PBPC mobilization, and SCN) did not include sufficient numbers of subjects aged 65 and older to determine whether elderly subjects respond differently from younger subjects.
Gender
There is no FDA guidance on the use of Filgrastim with respect to specific gender populations.
Race
There is no FDA guidance on the use of Filgrastim with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Filgrastim in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Filgrastim in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Filgrastim in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Filgrastim in patients who are immunocompromised.
Administration and Monitoring
Administration
Filgrastim is supplied in either vials or in prefilled syringes with UltraSafe® Needle GuARDS. Following administration of Filgrastim from the prefilled syringe, the UltraSafe® Needle Guard should be activated to prevent accidental needle sticks. To activate the UltraSafe® Needle Guard, place your hands behind the needle, grasp the guard with one hand, and slide the guard forward until the needle is completely covered and the guard clicks into place. NOTE: If an audible click is not heard, the needle guard may not be completely activated. The prefilled syringe should be disposed of by placing the entire prefilled syringe with guard activated into an approved puncture-proof container.
Monitoring
There is limited information regarding Filgrastim Monitoring in the drug label.
IV Compatibility
There is limited information about the IV Compatibility.
Overdosage
In cancer patients receiving Filgrastim as an adjunct to myelosuppressive chemotherapy‚ it is recommended to avoid the potential risks of excessive Leukocytosis‚ that Filgrastim therapy be discontinued if the ANC surpasses 10‚000/mm3 after the chemotherapy-induced ANC nadir has occurred. Doses of Filgrastim that increase the ANC beyond 10‚000/mm3 may not result in any additional clinical benefit. The maximum tolerated dose of Filgrastim has not been determined. Efficacy was demonstrated at doses of 4 to 8 mcg/kg/day in the phase 3 study of nonmyeloablative chemotherapy. Patients in the BMT studies received up to 138 mcg/kg/day without toxic effects‚ although there was a flattening of the dose response curve above daily doses of greater than 10 mcg/kg/day. In Filgrastim clinical trials of cancer patients receiving myelosuppressive chemotherapy‚ WBC counts > 100‚000/mm3 have been reported in less than 5% of patients‚ but were not associated with any reported adverse clinical effects. In cancer patients receiving myelosuppressive chemotherapy‚ discontinuation of Filgrastim therapy usually results in a 50% decrease in circulating neutrophils within 1 to 2 days‚ with a return to pretreatment levels in 1 to 7 days.
Pharmacology
| Template:Px | |
Filgrastim
| |
| Systematic (IUPAC) name | |
| Human granulocyte colony stimulating factor | |
| Identifiers | |
| CAS number | |
| ATC code | L03 |
| PubChem | ? |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 18802.8 g/mol |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | ? |
Mechanism of Action
Colony-Stimulating Factors
Colony-stimulating factors are glycoproteins which act on hematopoietic cells by binding to specific cell surface receptors and stimulating proliferation‚ differentiation commitment‚ and some end-cell functional activation. Endogenous G-CSF is a lineage specific colony-stimulating factor which is produced by monocytes‚ fibroblasts, and endothelial cells. G-CSF regulates the production of neutrophils within the bone marrow and affects neutrophil progenitor proliferation‚2‚3 differentiation,2‚4 and selected end-cell functional activation (including enhanced phagocytic ability‚5 priming of the cellular metabolism associated with respiratory burst‚6 antibody dependent killing,7 and the increased expression of some functions associated with cell surface antigens8). G-CSF is not species-specific and has been shown to have minimal direct in vivo or in vitro effects on the production of hematopoietic cell types other than the neutrophil lineage.
Structure
Filgrastim is a human granulocyte colony-stimulating factor (G-CSF)‚ produced by recombinant DNA technology. Filgrastim is the Amgen Inc. trademark for filgrastim‚ which has been selected as the name for recombinant methionyl human granulocyte colony-stimulating factor (r-metHuG-CSF). Filgrastim is a 175 amino acid protein manufactured by recombinant DNA technology.1 Filgrastim is produced by Escherichia coli (E coli) bacteria into which has been inserted the human granulocyte colony-stimulating factor gene. Filgrastim has a molecular weight of 18‚800 daltons. The protein has an amino acid sequence that is identical to the natural sequence predicted from human DNA sequence analysis‚ except for the addition of an N-terminal methionine necessary for expression in E coli. Because Filgrastim is produced in E coli‚ the product is nonglycosylated and thus differs from G-CSF isolated from a human cell. Filgrastim is a sterile‚ clear‚ colorless‚ preservative-free liquid for parenteral administration containing filgrastim at a specific activity of 1.0 ± 0.6 x 108 U/mg (as measured by a cell mitogenesis assay). The product is available in single use vials and prefilled syringes. The single-use vials contain either 300 mcg or 480 mcg filgrastim at a fill volume of 1.0 mL or 1.6 mL, respectively. The single-use prefilled syringes contain either 300 mcg or 480 mcg filgrastim at a fill volume of 0.5 mL or 0.8 mL, respectively. See table below for product composition of each single-use vial or prefilled syringe.

Pharmacodynamics
In phase 1 studies involving 96 patients with various nonmyeloid malignancies‚ Filgrastim administration resulted in a dose-dependent increase in circulating neutrophil counts over the dose range of 1 to 70 mcg/kg/day.9-11 This increase in neutrophil counts was observed whether Filgrastim was administered IV (1 to 70 mcg/kg twice daily)‚9 SC (1 to 3 mcg/kg once daily)‚11 or by continuous SC infusion (3 to 11 mcg/kg/day).10 With discontinuation of Filgrastim therapy‚ neutrophil counts returned to baseline in most cases within 4 days. Isolated neutrophils displayed normal phagocytic (measured by zymosan-stimulated chemoluminescence) and chemotactic (measured by migration under agarose using N-formyl-methionyl-leucyl-phenylalanine [fMLP] as the chemotaxin) activity in vitro. The absolute monocyte count was reported to increase in a dose-dependent manner in most patients receiving Filgrastim; however‚ the percentage of monocytes in the differential count remained within the normal range. In all studies to date‚ absolute counts of both eosinophils and basophils did not change and were within the normal range following administration of Filgrastim. Increases in lymphocyte counts following Filgrastim administration have been reported in some normal subjects and cancer patients. White blood cell (WBC) differentials obtained during clinical trials have demonstrated a shift towARDS earlier granulocyte progenitor cells (left shift)‚ including the appearance of promyelocytes and myeloblasts‚ usually during neutrophil recovery following the chemotherapy-induced nadir. In addition‚ Dohle bodies‚ increased granulocyte granulation‚ and hypersegmented neutrophils have been observed. Such changes were transient and were not associated with clinical sequelae, nor were they necessarily associated with infection.
Pharmacokinetics
Absorption and clearance of Filgrastim follows first-order pharmacokinetic modeling without apparent concentration dependence. A positive linear correlation occurred between the parenteral dose and both the serum concentration and area-under-the-concentration-time curves. Continuous IV infusion of 20 mcg/kg of Filgrastim over 24 hours resulted in mean and median serum concentrations of approximately 48 and 56 ng/mL‚ respectively. Subcutaneous administration of 3.45 mcg/kg and 11.5 mcg/kg resulted in maximum serum concentrations of 4 and 49 ng/mL‚ respectively‚ within 2 to 8 hours. The volume of distribution averaged 150 mL/kg in both normal subjects and cancer patients. The elimination half-life‚ in both normal subjects and cancer patients‚ was approximately 3.5 hours. Clearance rates of Filgrastim were approximately 0.5 to 0.7 mL/minute/kg. Single parenteral doses or daily IV doses‚ over a 14-day period‚ resulted in comparable half-lives. The half-lives were similar for IV administration (231 minutes‚ following doses of 34.5 mcg/kg) and for SC administration (210 minutes‚ following Filgrastim doses of 3.45 mcg/kg). Continuous 24-hour IV infusions of 20 mcg/kg over an 11- to 20-day period produced steady-state serum concentrations of Filgrastim with no evidence of drug accumulation over the time period investigated. Pharmacokinetic data in geriatric patients (≥ 65 years) are not available.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
The carcinogenic potential of Filgrastim has not been studied. Filgrastim failed to induce bacterial gene mutations in either the presence or absence of a drug metabolizing enzyme system. Filgrastim had no observed effect on the fertility of male or female rats‚ or on gestation at doses up to 500 mcg/kg.
Clinical Studies
FDA Package Insert for Filgrastim contains no information regarding Clinical Studies.
How Supplied
Use only one dose per vial; do not re-enter the vial. Discard unused portions. Do not save unused drug for later administration. Use only one dose per prefilled syringe. Discard unused portions. Do not save unused drug for later administration.
Vials
Single-dose‚ preservative-free vials containing 300 mcg (1 mL) of filgrastim (300 mcg/mL). Dispensing packs of 10 (NDC 55513-530-10). Single-dose‚ preservative-free vials containing 480 mcg (1.6 mL) of filgrastim (300 mcg/mL). Dispensing packs of 10 (NDC 55513-546-10).
Prefilled Syringes (SingleJect®)
Single-dose‚ preservative-free, prefilled syringe with 27 gauge, ½ inch needle with an UltraSafe® Needle Guard, containing 300 mcg (0.5 mL) of filgrastim (600 mcg/mL). Dispensing packs of 1 (NDC 55513-924-91). Single-dose‚ preservative-free, prefilled syringes with 27 gauge, ½ inch needles with an UltraSafe® Needle Guard, containing 300 mcg (0.5 mL) of filgrastim (600 mcg/mL). Dispensing packs of 10 (NDC 55513-924-10). Single-dose‚ preservative-free, prefilled syringe with 27 gauge, ½ inch needle with an UltraSafe® Needle Guard, containing 480 mcg (0.8 mL) of filgrastim (600 mcg/mL). Dispensing packs of 1 (NDC 55513-209-91). Single-dose‚ preservative-free, prefilled syringes with 27 gauge, ½ inch needles with an UltraSafe® Needle Guard, containing 480 mcg (0.8 mL) of filgrastim (600 mcg/mL). Dispensing packs of 10 (NDC 55513-209-10). The needle cover of the prefilled syringe contains dry natural rubber (a derivative of latex).
Storage
Filgrastim should be stored at 2° to 8°C (36° to 46°F). Avoid shaking.
Images
Drug Images
{{#ask: Page Name::Filgrastim |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Filgrastim |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Information for Patients and Caregivers
This patient package insert provides information and instructions for people who will be receiving Filgrastim and their caregivers. This patient package insert does not tell you everything about Filgrastim. You should discuss any questions you have about treatment with Filgrastim with your doctor.
What is Filgrastim?
Filgrastim is a man-made form of granulocyte colony-stimulating factor (G-CSF), which is made using the bacteria Escherichia coli. G-CSF is a substance naturally produced by the body. It stimulates the growth of neutrophils (nu-tro-fils), a type of white blood cell important in the body’s fight against infection. What is Filgrastim used for?
Filgrastim is used to treat neutropenia (nu-tro-peen-ee-ah), a condition where the body makes too few neutrophils. Neutropenia may be a long-standing condition where your body does not make enough neutrophils or it may be caused by drugs used to treat cancer. In some cases, your body may make enough neutrophils but as part of your treatment for cancer your doctor may want to increase the number of certain blood cells (CD34 cells) and collect them. The cells are collected using a process called apheresis (ay-fer-ree-sis). These collected cells are given back to you after you receive very high doses of treatment for cancer to make your blood counts get back to normal more quickly.
How does Filgrastim work?
Filgrastim works by helping your body make more neutrophils. To make sure Filgrastim is working, your doctor will ask that you have regular blood tests to count the number of neutrophils you have. It is important that you follow your doctor’s instructions about getting these tests.
Who should not take Filgrastim?
Do not take Filgrastim if you are: Allergic to Filgrastim (filgrastim) or any of its ingredients. See the end of this leaflet for a list of ingredients in Filgrastim. Allergic to other medicines made using the bacteria E coli. Ask your doctor if you are not sure.
What important information do I need to know about taking Filgrastim?
Filgrastim may reduce your chance of getting an infection, but does not prevent all infections. An infection can still happen during the short time when your/your child's neutrophil levels are low. You must be alert and look for some of the common signs or symptoms of infection, such as fever, chills, rash, sore throat, diarrhea, redness, swelling, or pain around a cut or sore. If you/your child has any of these signs or symptoms during treatment with Filgrastim, tell your doctor or nurse immediately. There is a possibility that you/your child could have a reaction at an injection site. If there is a lump, swelling, or bruising at an injection site that does not go away, call your doctor. If you have a sickle cell disorder, make sure that you tell your doctor before you start taking Filgrastim. If you have a sickle cell crisis after getting Filgrastim, tell your doctor right away. Talk to your doctor if you experience unusual bleeding or bruising while taking Filgrastim, as this could mean a decrease of platelets which reduces the ability of blood to clot. Make sure your doctor knows about all medicines, and herbal or vitamin supplements you are taking before starting Filgrastim. If you are taking lithium you may need more frequent blood tests. If you/your child are receiving Filgrastim because you are also receiving chemotherapy, the last dose of Filgrastim should be injected at least 24 hours before your next dose of chemotherapy. There is more information about Filgrastim in the Physician Package Insert. If you have any questions, you should talk to your doctor.
What are possible serious side effects of Filgrastim?
- Spleen Rupture. Your spleen may become enlarged and can rupture while taking Filgrastim. A ruptured spleen can cause death. The spleen is located in the upper left section of your stomach area. Call your doctor right away if you/your child has pain in the left upper stomach area or left shoulder tip area. This pain could mean your/your child’s spleen is enlarged or ruptured.
- Serious Allergic Reactions. Filgrastim can cause serious allergic reactions. These reactions can cause a rash over the whole body, shortness of breath, wheezing, dizziness, swelling around the mouth or eyes, fast pulse, and sweating. If you or your child starts to have any of these symptoms, stop using Filgrastim and call your doctor or seek emergency care right away. If you/your child has an allergic reaction during the injection of Filgrastim, stop the injection right away.
- A serious lung problem called acute respiratory distress syndrome (ARDS). Call your doctor or seek emergency care right away if you/your child has shortness of breath, trouble breathing or a fast rate of breathing.
What are the most common side effects of Filgrastim?
The most common side effect you/your child may experience is aching in the bones and muscles. This aching can usually be relieved by taking a non-aspirin pain reliever such as acetaminophen. Some people experience redness, swelling, or itching at the site of injection. This may be an allergy to the ingredients in Filgrastim or it may be a local reaction. If you are giving an injection to a child, look for signs of redness, swelling, or itching at the site of injection because they may not be able to tell you they are experiencing a reaction. If you notice any signs of a local reaction, call your doctor.
What about pregnancy or breastfeeding?
Filgrastim has not been studied in pregnant women, and its effects on unborn babies are not known. If you take Filgrastim while you are pregnant, it is possible that small amounts of it may get into your baby’s blood. It is not known if Filgrastim can get into human breast milk. If you are pregnant, plan to become pregnant, think you may be pregnant, or are breast feeding, you should tell your doctor before using Filgrastim. If you become pregnant during Filgrastim treatment, you are encouraged to enroll in Amgen's Pregnancy Surveillance Program. You should call 1-800-77-AMGEN (1-800-772-6436) to enroll. If you breastfeed during Filgrastim treatment, you are encouraged to enroll in Amgen’s Lactation Surveillance Program. You should call 1-800-77-AMGEN (1-800-772-6436) to enroll.
How to prepare and give a Filgrastim injection?
Filgrastim should be injected at the same time each day. If you miss a dose contact your doctor or nurse. You must always use the correct dose of Filgrastim. Too little Filgrastim may not protect you against infections, and too much Filgrastim may cause too many neutrophils to be in your blood. Your doctor will determine your/your child’s correct dose based on your/your child's body weight. If you are giving someone else Filgrastim injections, it is important that you know how to inject Filgrastim, how much to inject, and how often to inject Filgrastim. Filgrastim is available as a liquid in vials or in prefilled syringes. When you receive your Filgrastim, always check to see that:
- The name Filgrastim appears on the package and vial or prefilled syringe label.
- The expiration date on the vial or prefilled syringe label has not passed. You should not use a vial or prefilled syringe after the date on the label.
- The strength of the Filgrastim (number of micrograms in the colored dot on the package containing the vial or prefilled syringe) is the same as your doctor prescribed.
- The Filgrastim liquid in the vial or in the prefilled syringe is clear and colorless. Do not use Filgrastim® if the contents of the vial or prefilled syringe appear discolored or cloudy, or if the vial or prefilled syringe appears to contain lumps, flakes, or particles.
If you are using vials of Filgrastim only use the syringe that your doctor prescribes.
Your doctor or nurse will give you instructions on how to measure the correct dose of Filgrastim. This dose will be measured in milliliters. You should only use a syringe that is marked in tenths of milliliters, or mL (for example, 0.2 mL). The doctor or nurse may refer to an mL as a cc (1 mL = 1 cc). If you do not use the correct syringe, you/your child could receive too much or too little Filgrastim.
Only use disposable syringes and needles. Use the syringes only once and dispose of them as instructed by your doctor or nurse.
IMPORTANT: TO HELP AVOID POSSIBLE INFECTION, YOU SHOULD FOLLOW THESE INSTRUCTIONS.
Setting up for an injection
1. Find a clean flat working surface, such as a table. 2. Remove the vial or prefilled syringe of Filgrastim from the refrigerator. Allow Filgrastim to reach room temperature (this takes about 30 minutes). Vials or prefilled syringes should be used only once. DO NOT SHAKE 3. THE VIAL OR PREFILLED SYRINGE. Shaking may damage the Filgrastim. If the vial or prefilled syringe has been shaken vigorously, the solution may appear foamy and it should not be used.
- Assemble the supplies you will need for an injection:

Precautions with Alcohol
Alcohol-Filgrastim interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
NEUPOGEN
Look-Alike Drug Names
Filgrastim - Neumega
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Kendra JR, Rugman FP, Flaherty TA, Myers A, Horsfield N, Barton A; et al. (1993). "First use of G-CSF in chlorpromazine-induced agranulocytosis: a report of two cases". Postgrad Med J. 69 (817): 885–7. PMC 2399942. PMID 7507240.
- ↑ Herrmann J (1994). "[Granulocyte colony-stimulating factor (G-CSF) in the early stage of thyrostatic-induced agranulocytosis]". Dtsch Med Wochenschr. 119 (13): 463–6. doi:10.1055/s-2008-1058716. PMID 7512460.
- ↑ Gruner U, tho Pesch S, Spittler S, Schaefer HE, Peters U (1994). "[Treatment of clozapine-induced agranulocytosis using granulocyte colony-stimulating factor]". Dtsch Med Wochenschr. 119 (43): 1467–70. doi:10.1055/s-2008-1058861. PMID 7525175.
- ↑ Derici U, Ayerdem F, Arinsoy T, Reis KA, Dalgic A, Sindel S (2002). "The use of granulocyte colony-stimulating factor in a neutropenic renal transplant recipient". Haematologia (Budap). 32 (4): 557–60. PMID 12803133.
- ↑ Yoshida M, Karasawa M, Naruse T, Fukuda M, Hirashima K, Oh H; et al. (1999). "Effect of granulocyte-colony stimulating factor on empiric therapy with flomoxef sodium and tobramycin in febrile neutropenic patients with hematological malignancies. Kan-etsu Hematological Disease and Infection Study Group". Int J Hematol. 69 (2): 81–8. PMID 10071455.
- ↑ Schäfer H, Hübel K, Bohlen H, Mansmann G, Hegener K, Richarz B; et al. (2000). "Perioperative treatment with filgrastim stimulates granulocyte function and reduces infectious complications after esophagectomy". Ann Hematol. 79 (3): 143–51. PMID 10803937.
- ↑ Carella AM, Cascavilla N, Greco MM, Melillo L, Sajeva MR, Ladogana S; et al. (2001). "Treatment of "poor risk" acute [[myeloid leukemia]] with fludarabine, cytarabine and G-CSF (flag regimen): a single center study". Leuk Lymphoma. 40 (3–4): 295–303. doi:10.3109/10428190109057928. PMID 11426551. URL–wikilink conflict (help)
- ↑ Karthaus M, Rosenthal C, Huebner G, Paul H, Elser C, Hertenstein B; et al. (1998). "Effect of topical oral G-CSF on oral mucositis: a randomised placebo-controlled trial". Bone Marrow Transplant. 22 (8): 781–5. doi:10.1038/sj.bmt.1701434. PMID 9827976.
- ↑ Kojima S, Hibi S, Kosaka Y, Yamamoto M, Tsuchida M, Mugishima H; et al. (2000). "Immunosuppressive therapy using antithymocyte globulin, cyclosporine, and danazol with or without human granulocyte colony-stimulating factor in children with acquired aplastic anemia". Blood. 96 (6): 2049–54. PMID 10979946.
- ↑ Kocherlakota P, La Gamma EF (1998). "Preliminary report: rhG-CSF may reduce the incidence of neonatal sepsis in prolonged preeclampsia-associated neutropenia". Pediatrics. 102 (5): 1107–11. PMID 9794941.
- ↑ Bernstein HM, Pollock BH, Calhoun DA, Christensen RD (2001). "Administration of recombinant granulocyte colony-stimulating factor to neonates with septicemia: A meta-analysis". J Pediatr. 138 (6): 917–20. doi:10.1067/mpd.2001.114014. PMID 11391341.
- ↑ Adachi N, Tsuchiya H, Nunoi H, Higuchi S, Akaboshi I, Chikazawa S (1990). "rhG-CSF for Shwachman's syndrome". Lancet. 336 (8723): 1136. PMID 1700246.
{{#subobject:
|Label Page=Filgrastim |Label Name=Filgrastim_label_01.jpg
}}
{{#subobject:
|Label Page=Filgrastim |Label Name=Filgrastim_label_02.jpg
}}
{{#subobject:
|Label Page=Filgrastim |Label Name=Filgrastim_label_03.jpg
}}
{{#subobject:
|Label Page=Filgrastim |Label Name=Filgrastim_label_04.jpg
}}
{{#subobject:
|Label Page=Filgrastim |Label Name=Filgrastim_label_05.jpg
}}
{{#subobject:
|Label Page=Filgrastim |Label Name=Filgrastim_label_06.jpg
}}
{{#subobject:
|Label Page=Filgrastim |Label Name=Filgrastim_panel_01.png
}}
{{#subobject:
|Label Page=Filgrastim |Label Name=Filgrastim_panel_02.png
}}
{{#subobject:
|Label Page=Filgrastim |Label Name=Filgrastim_panel_03.png
}}
{{#subobject:
|Label Page=Filgrastim |Label Name=Filgrastim_panel_04.png
}}