Fever pathophysiology
|
Fever Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Fever pathophysiology On the Web |
|
American Roentgen Ray Society Images of Fever pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Pathophysiology
Temperature is regulated in the hypothalamus, in response to PGE2. PGE2 release, in turn, comes from a trigger, a pyrogen. The hypothalamus generates a response back to the rest of the body, making it increase the temperature set-point.
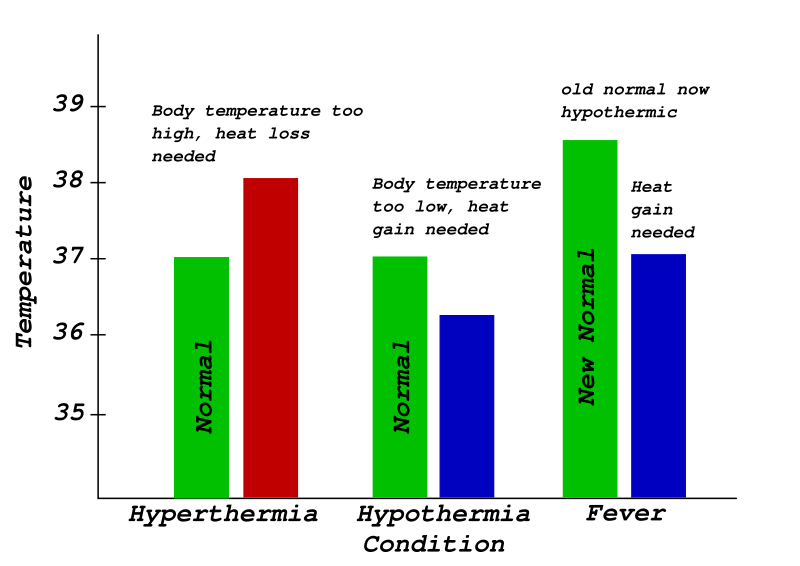
Hypothermia: Characterized in the center: Normal body temperature is shown in green, while the hypothermic temperature is shown in blue. As can be seen, hypothermia can be conceptualized as a decrease below the thermoregulatory set-point.
Fever: Characterized on the right: Normal body temperature is shown in green. It reads "New Normal" because the thermoregulatory set-point has risen. This has caused what was the normal body temperature (in blue) to be considered hypothermic.
Pyrogens
A pyrogen is a substance that induces fever. These can be either internal (endogenous) or external (exogenous). The bacterial substance lipopolysaccharide (LPS) is an example of an exogenous pyrogen.
Endogenous
The cytokines (such as interleukin 1) are a part of the innate immune system, produced by phagocytic cells, and cause the increase in the thermoregulatory set-point in the hypothalamus. Other examples of endogenous pyrogens are interleukin 6 (IL-6), and the tumor necrosis factor-alpha.
These cytokine factors are released into general circulation where they migrate to the circumventricular organs of the brain, where the blood-brain barrier is reduced. The cytokine factors bind with endothelial receptors on vessel walls, or interact with local microglial cells. When these cytokine factors bind, they activate the arachidonic acid pathway.
Exogenous
One model for the mechanism of fever caused by exogenous pyrogens includes LPS, which is a cell wall component of gram-negative bacteria. An immunological protein called lipopolysaccharide-binding protein (LBP) binds to LPS. The LBP–LPS complex then binds to the CD14 receptor of a nearby macrophage. This binding results in the synthesis and release of various endogenous cytokine factors, such as interleukin 1 (IL-1), interleukin 6 (IL-6), and the tumor necrosis factor-alpha. In other words, exogenous factors cause release of endogenous factors, which, in turn, activate the arachidonic acid pathway.
PGE2 release
PGE2 release comes from the arachidonic acid pathway. This pathway (as it relates to fever), is mediated by the enzymes phospholipase A2 (PLA2), cyclooxygenase-2 (COX-2), and prostaglandin E2 synthase. These enzymes ultimately mediate the synthesis and release of PGE2.
PGE2 is the ultimate mediator of the febrile response. The set-point temperature of the body will remain elevated until PGE2 is no longer present. PGE2 acts on neurons in the preoptic area (POA) through the EP3 subtype of PGE receptors and the EP3-expressing neurons in the POA innervate the dorsomedial hypothalamus (DMH), the rostral raphe pallidus nucleus in the medulla oblongata (rRPa) and the paraventricular nucleus of the hypothalamus (PVN). Fever signals sent to the DMH and rRPa lead to stimulation of the sympathetic output system, which evokes non-shivering thermogenesis to produce body heat and skin vasoconstriction to decrease heat loss from the body surface. It is presumed that the innervation from the POA to the PVN mediates the neuroendocrine effects of fever through the pathway involving pituitary gland and various endocrine organs.
Hypothalamus response
The brain ultimately orchestrates heat effector mechanisms. These may be;
- Increased heat production by increased muscle tone, shivering and hormones like epinephrine.
- Prevention of heat loss, such as vasoconstriction.
The autonomic nervous system may also activate brown adipose tissue to produce heat (non-exercise-associated thermogenesis, also known as non-shivering thermogenesis), but this seems mostly important for babies. Increased heart rate and vasoconstriction contribute to increased blood pressure in fever.