Epidural

|
WikiDoc Resources for Epidural |
|
Articles |
|---|
|
Most recent articles on Epidural |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Epidural at Clinical Trials.gov Clinical Trials on Epidural at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Epidural
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating Epidural Risk calculators and risk factors for Epidural
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Epidural |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Nima Nasiri, M.D.[2]
Overview
The term epidural is often short for epidural anesthesia, a form of regional anesthesia involving injection of drugs through a catheter placed into the epidural space. The epidural space (or extradural space or peridural space) is the space inside the spinal canal but outside the membrane called the dura mater (sometimes called the "dura"). In contact with the inner surface of the dura is another membrane called the arachnoid mater ("arachnoid"). The arachnoid encompasses the cerebrospinal fluid that surrounds the spinal cord. Epidural analgesia (pain relief) is a type of Regional Anesthesia which is commonly used to ease the pain of labor and childbirth but can also be used to provide anesthesia for other types of surgeries. A Spanish surgeon named Fidel Pagés Miravé reported the first single-shot thoracolumbar epidural anesthesia in 1921. After a decade, the Italian surgeon Achille M. Dogliotti described a reproducible loss-of-resistance technique to identify the epidural space. Epidural is a technique for perioperative pain management with different applications in anesthesiology and it can be a single shot or a continuous infusion for long term pain relief. Epidural is excellent analgesic, it decreases the side effect of other anesthetics and analgesics and reducing their side effects. Low blood pressure, fever, nausea, difficulty urinating are complications of epidural anesthesia. An epidural is a way of anesthetic which is used for pain relief during labor, it stops pain signals traveling from the spine to the brain. During labor, anesthesiologists injecting a small amount of anesthetic into the epidural space of the spine. The epidural space is filled with fluid and surrounds the spinal cord. Nerves that carry pain signals from the body to the brain (spinal nerves) connect to the spinal cord in certain places. The anesthetic numbs the spinal nerves, blocking the pain signals. Spinal anesthesia is a technique whereby a local anesthetic drug is injected into the cerebrospinal fluid. This technique has some similarity to epidural anesthesia, and the two techniques may be easily confused with each other.
History of epidural anesthesia
- In 1921, a Spanish surgeon named Fidel Pages developed the epidural anesthesia technique, he was the pioneer of lumbar epidural anesthesia.[1]
- In 1931, Eugene Aburel, a Romanian obstetrician, performed the lumbar obstetric Epidural analgesia.[2]
- In 1933, an Italian surgen, named Achille M. Dogliotti described a loss-of-resistance technique to identify the epidural space.[3]
- In 1949, Manuel Martinez Curbelo, a Cuban physician reported the first successful continuous lumbar Epidural anaesthesia.[2]
Epidural anaesthesia and analgesia indication
Indications for epidural anaesthesia and analgesia have expanded over the past decades, a summary of major indications for epidural include:[4][5][6][7]
- For analgesia alone, where surgery is not contemplated. An epidural for pain relief (e.g. in childbirth) is unlikely to cause loss of muscle power but is not usually sufficient for surgery.
- As an adjunct to general anaesthesia. The anesthetist may use epidural analgesia in addition to general anesthesia. This may reduce the patient's requirement for opioid analgesics. This is suitable for a wide variety of surgery, for example gynaecological surgery (e.g. hysterectomy), orthopaedic surgery (e.g. hip replacement), general surgery (e.g. laparotomy) and vascular surgery (e.g. open aortic aneurysm repair). See also caudal epidural, below.
- As a sole technique for surgical anesthesia . Some operations, most frequently Caesarean section, may be performed using an epidural anesthetic as the sole technique. Typically the patient would remain awake during the operation. The dose required for anesthesia is much higher than that required for analgesia.
- For post-operative analgesia, in either of the two situations above. Analgesics are given into the epidural space for a few days after surgery, provided a catheter has been inserted. Through the use of a patient-controlled analgesia (PCA) infusion pump, a patient may be given the ability to control post-surgical pain medications administered through the epidural.
- For the treatment of back pain. Injection of analgesics and steroids into the epidural space may improve some forms of back pain. See below.
- For the treatment of chronic pain or palliation of symptoms in terminal care, usually in the short or medium term.
Because of the nature of epidurals, they are most suitable for analgesia for the abdomen, pelvis or legs. They are much less suitable for analgesia for the chest, neck, or arms and are not possible for the head.
Cautions
There are circumstances where the risks of an epidural are higher than normal. These circumstances include:
- Anatomical abnormalities, such as spina bifida, meningomyelocele or scoliosis
- Previous spinal surgery (which may cause an acquired tethered spinal cord)
- Certain problems of the central nervous system, including multiple sclerosis or syringomyelia
- Certain heart-valve problems (such as aortic stenosis)
Contraindications
These are circumstances in which epidurals should not be used:
A relative contraindication to neuraxial anesthesia include:[8]
- Low platelets but no bleeding diathesis
- Infection remote from the site of lumbar puncture
- Progressive neurologic diseases
- Raised intracranial pressure
- Hypovolemia
- Fixed cardiac output (eg, severe aortic stenosis)
Absolute contraindication:[8]
- Patient refusal
- Lack of adequate staff
- Bleeding disorder (coagulopathy) or anticoagulant medication (e.g. warfarin)
- Infection near the point of insertion
- Infection in the bloodstream which may "seed" onto the catheter i.e septicemia which antibiotics must be given prior to anesthesia.
Anatomy
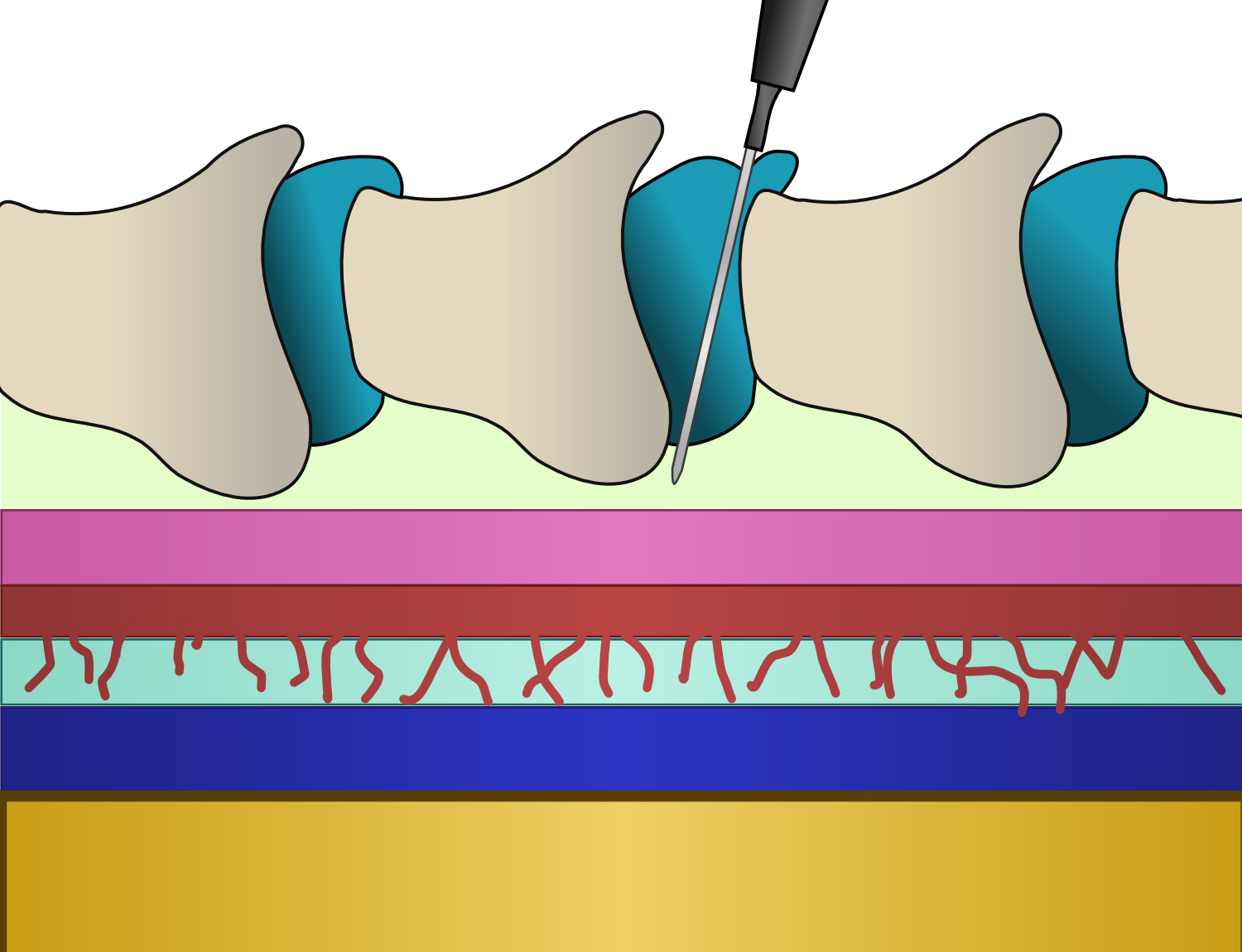
The diagram at right depicts the various structures of the spinal column. The spinal cord (yellow core) is in intimate contact with the pia mater (blue). The arachnoid (red) exists superficial to the pia mater, and is attached to it by many, many trabeculae, giving it a spider-like appearance. This space (light blue) is filled with cerebrospinal fluid (CSF) and is called the subarachnoid space. Superficial to the arachnoid is the dura mater (pink) and although they are unattached, they are kept firmly pressed against one another because of pressure exerted by the CSF. Superficial to the dura mater is a space (pale green), known as the epidural space, that exists between it and the internal surfaces of the vertebral bones and their supporting ligamentous structures. The vertebral bones (taupe) are attached to one another by the interspinous ligaments (teal), and it is through this ligament that the needle used to place the epidural catheter is put.
Technique of insertion
Epidural anesthesia should always be performed by a trained anesthetist, using a strict aseptic technique to reduce the risk of infection. American Society of Anesthesiologists Task Force recommends the following steps on infection control during epidural anesthesia:[9]
- Removal of jewelry from hands
- Handwashing
- Wearing of caps and sterile gloves
- Wearing masks that cover both mouth and nose; masks should be changed between cases
- Individually packaged skin preparation
- Chlorhexidine with alcohol for skin preparation; this must be allowed to dry before needle insertion; povidone-iodine with alcohol is also acceptable
- Sterile draping
- Sterile occlusive dressing
Position of the patient
The insertion of epidural catheters for analgesia in labor may be carried out with the patient in the sitting or lateral position.[10][8]
- Epidural block can be performed in the lateral or sitting position, and the decision is usually based on anesthesiologist and patient preferences.[11]
- When the spinous processes are not easily palpable, the sitting position is preferred. In patients with easily identifiable landmarks, neither the lateral nor the sitting position is superior with regard to patient comfort, but heavier patients preferred the sitting position.
- In some patients, the sitting position may be associated with orthostatic hypotension and syncope. For this reason, it is important for an assistant to provide continuous support to the patient during the procedure. Maternal cardiac output can be reduced in the left lateral position if held too tightly in position. [12]
- The sitting patient is asked to slouch and bend forward slightly from the waist to increase the curvature of the spine. The lying patient is asked to draw the knees up to the chin for the same reason. In the sitting position, the midline can be found by drawing a straight line between the vertebra of C7 (palpable in most patients) and the coccygeal cleft.
- Ultrasound identification of the midline may be useful to locate the midline, determine the approximate depth to the epidural space, and to determine the level of puncture.[13]
Insertion site
The anesthetist palpates the patient's back and identifies a suitable anatomical gap between the bony spinous processes prior to the procedure. Anesthesiologists use ultrasound imaging to detect the anatomic structure of the lumbar spine in order to insert the needle in epidural space.[14][15]
- The level of the spine at which the catheter is best placed depends mainly on the size and type of an intended operation or the anatomical origin of pain.
- Suboptimal epidural catheter insertion may occur during the block and complications such as paresthesia and venous and subarachnoid cannulation may occur.
- Administration of local anesthetic through the epidural needle before catheter insertion improves the quality of anesthesia, a single-injection dose of local anesthetic (20 mL of 2% lidocaine) through the epidural needle into the epidural space before catheter insertion is used to ease the induction.
- Most commonly, the anesthetist conducting an epidural place the catheter in the mid-lumbar, or lower back region of the spine, although occasionally a catheter is placed in the thoracic (chest) or cervical (neck) region. In adults, the spinal cord terminates at the first lumbar vertebra, below which lies a bundle of nerves known as the cauda equina ("horse's tail"). Hence, lumbar epidurals carry a very low risk of injuring the spinal cord.
Locating the epidural space
- The skin is infiltrated with a local anesthetic such as lidocaine over the identified space. The insertion point is usually in the midline, although other approaches, such as the paramedian approach, may occasionally be employed. [16][17]
- A particular type of needle known as a Tuohy needle 16 or 18 gauge is almost invariably used. This needle was specially designed for locating the epidural space safely and has several specific features for this purpose.
- The Tuohy needle is inserted to the interspinous ligament and a loss of resistance to injection technique is used to identify the epidural space. This technique works because the interspinous ligament is extremely dense, and injection into it is almost impossible. The anesthetist attaches a syringe to the Tuohy needle and advances it slowly.
- The syringe may contain air or saline. The principles are the same, but the specifics of the technique are different due to the greater compressibility of air with respect to saline.
- When the tip of the needle enters a space of negative or neutral pressure (such as the epidural space), there will be a "loss of resistance" and it will be possible to inject through the syringe. There is now a high likelihood that the tip of the needle has entered the epidural space. A sensation of "pop" or "click" may be felt as the needle breaches the ligamentum flavum just before entering the epidural space.
- Traditionally anesthetists have used either air or saline for identifying the epidural space, depending on their personal preference. however, the evidence is accumulating that saline may result in a more rapid and satisfactory quality of analgesia.[18]
- In addition to the loss of resistance technique, realtime observation of the progress of the needle is becoming more common. This may be done using a portable ultrasound scanner, or with fluoroscopy (moving X-ray pictures).
- The position of an epidural catheter and the distribution of local anesthetic drugs in the epidural space are two of the most important determining factors for successful epidural analgesia.
Feeding the catheter
- After placement of the tip of the Tuohy needle into the epidural space the catheter is threaded through the needle. The needle is then withdrawn over the catheter. Generally, the catheter is then withdrawn slightly so that 4-6 cm remains in the epidural space. The catheter has depth markings on it (see photo) so that the length of the catheter in the epidural space can be estimated.
- The catheter is a fine plastic tube, down which anesthetics may be given into the epidural space. Early catheters had a hole at the end ("end-hole catheters"), but were prone to blockage. More modern catheters ("side-hole catheters") have a blind end but three or more side-holes along the shaft near the tip. This not only disperses the anesthetic more widely around the catheter but lessens the likelihood of blockage.
- The catheter is typically secured to the skin with adhesive tape or dressings to prevent it from becoming dislodged.
- In some unusual instances, it may not be required to insert a catheter into the epidural space, e.g. for steroid injections; see below. The anesthesiologist may inject medication into the epidural space through the needle, then remove the needle.
- complications including abscess, spinal hematoma, radiculopathy, breakage, migration may occur during insertion of the catheter. [19]
Anaesthetic drugs
- A patient receiving an epidural for pain relief typically receives a combination of local anesthetics and opioids. This combination works better than either type of drug used alone. This combination helps to reduce the dose of the local anesthetic agent.
- Local anesthetic agents are combined with morphine, fentanyl or clonidine to prolong the epidural effect or to stabilize the blood pressure. Common local anesthetics include lidocaine, bupivacaine, ropivacaine, and chloroprocaine. Common opioids include morphine, fentanyl, sufentanil, and pethidine (known as meperidine in the U.S.). These are injected in relatively small doses.
Bolus or infusion?
- For a short procedure, the anesthetist may introduce a single dose of medication (the "bolus" technique). This will eventually wear off. Thereafter, the anesthetist may repeat the bolus provided the catheter remains undisturbed.
- For a prolonged effect, a continuous infusion of drugs may be employed. A common solution for epidural infusion in childbirth or for post-operative analgesia is 0.2% ropivacaine or 0.125% bupivacaine, with 2 μg/mL of fentanyl added. This solution is infused at a rate between 4 and 14 mL/hour, following a loading dose to initiate the nerve block.
- There is some evidence that an intermittent bolus technique provides better analgesia than a continuous infusion technique when the total doses are identical.
Removing the catheter
- The catheter should be withdrawn when it is no longer used. An epidural catheter is likely to be safe if left in for up to 72 hours.[20]
- The risk of problems such as infection rises sharply after this time. Subcutaneously tunneled epidural catheters may be left in place for longer periods, without as much risk of infection.
- If prolonged analgesics are needed, tunneled epidural catheters can be used. This might reduce the risk of infection including epidural abscess formation.
Other types of epidural
Combined spinal-epidurals
Combined spinal and epidural anaesthesia (CSE) is a regional anaesthetic technique, which combines the rapid spinal block with the flexibility of continuous epidural to extend the duration of analgesia. This is an effective way to reduce the total drug dosage required for anaesthesia or analgesia.[21]
- For some procedures, the anaesthetist may choose to combine the rapid onset and reliable, dense block of a spinal anaesthetic with the post-operative analgesic effects of an epidural. This is called combined spinal and epidural anaesthesia (CSE).
- The anaesthetist may insert the spinal anaesthetic at one level, and the epidural at an adjacent level. Alternatively, after locating the epidural space with the Tuohy needle, a spinal needle may be inserted through the Tuohy needle into the subarachnoid space. The spinal dose is then given, the spinal needle withdrawn, and the epidural catheter inserted as normal. This method, known as the "needle-through-needle" technique, may be associated with a slightly higher risk of placing the catheter into the subarachnoid space.
- Many studies have confirmed that low-dose CSE with local anaesthetic and opioid, or low-dose epidural block alone, will provide effective analgesia with minimal motor and proprioceptive block.
Caudal epidurals
- It is performed by inserting a standard 21G needle through the sacral hiatus to gain entrance into the sacral epidural space. Injecting a volume of local anesthetic here provides good analgesia of the perineum and genital areas. This is typically a single-injection technique and a catheter is not normally placed. This is known as a caudal epidural or "caudal".[22]
- It is performed by inserting a needle through the sacral hiatus to gain entrance into the sacral epidural space.
- The caudal epidural is an effective and safe analgesic technique in children undergoing pelvic or perineal surgery. It is usually combined with general anesthesia.
- A well-documented epidural complication, a “wet tap,” results in a headache and possible total spinal anesthesia/block, requiring immediate maintenance of the patient’s airway and blood pressure.
Techniques of Caudal Epidural Block
There are different techniques to perform caudal epidural block during anesthesia, by advances in diagnostic imaging tools, anesthesiologists can use ultrasound-guided block rather than the blind technique. [23]
Blind Caudal Epidural Block:
- In blind caudal block, the patient can be placed in prone or lateral decubitus position, a line is drawn to connect the bilateral posterior superior iliac crests and used as one side of an equilateral triangle; then the location of the sacral hiatus should be approximated.
- By palpating the sacral cornua as 2 bony prominences, the sacral hiatus could be identified as a dimple in between. A needle is inserted at 45 degrees to the sacrum and redirected if the posterior surface of the sacral bone is contacted.
Fluoroscopy-Guided Caudal Epidural Block:
- In this technique, the patient is usually placed in a prone position for the fluoroscopy-guided caudal epidural block. In lateral view of fluoroscopy, the sacral hiatus could be identified as an abrupt drop off at the end of S4 lamina.
- The block needle trajectory can be visualized and navigated accordingly into the sacral canal.
- By injecting contrast medium under fluoroscopy, the placement of needle tip within the sacral epidural space can be verified, and intravascular or intrathecal needle tip placement can be detected.
Ultrasound-Guided Caudal Epidural Block:
- In 2003, Klocke and colleagues first described the ultrasound-guided caudal block, thereafter use of ultrasound-guided epidural gained popularity.[24]
- The ultrasound transducer is placed at the midline to have the transverse view of sacral hiatus.
- The two sacral cornua appear as two hyperechoic structures on ultrasound. Between the sacral cornua are two band-like hyperechoic structures; the superficial one is the SCL, and the deep one is the dorsal surface of sacral bone.
- At this level, the ultrasound transducer is rotated 90 degrees to obtain the longitudinal view of sacral hiatus (Figure 5). Under longitudinal view, the block needle is inserted using the “in-plane” technique. The block needle can be visualized in real-time, piercing the SCL, entering the sacral hiatus, but cannot be visualized beyond the apex of sacral hiatus.
Epidural steroid injections
- An epidural injection, or epidural steroid injection, may be used to help reduce the pain caused by a herniated disc, degenerative disc disease, or spinal stenosis. These spinal disorders often affect the cervical (neck) and lumbar (lower back) areas of the spine.
- The medicine used in the injection is usually a combination of a local anesthetic (e.g. bupivacaine) and a steroid (e.g. triamcinolone).
- The technique and risks of the procedure are similar to those for standard epidural analgesia. The effects of an epidural steroid injection vary, but the permanent benefit is unlikely
- Some patients who have some residual pain after the first injection may receive a second or third epidural steroid injection. Patients who do not receive any relief from the first injection are unlikely to benefit from a second injection.
Benefits of epidural analgesia after surgery
Epidural analgesia has been demonstrated to have several benefits after surgery. These include:
- Effective analgesia without the need for systemic opioids [25].
- The incidence of postoperative respiratory problems and chest infections is reduced [26].
- The incidence of postoperative myocardial infarction ("heart attack") is reduced [27].
- The stress response to surgery is reduced [28].
- Motility of the intestines is improved by blockade of the sympathetic nervous system [29].
- Use of epidural analgesia during surgery reduces blood transfusion requirements [30].
Despite these benefits, no survival benefit has been proven for high-risk patients [31].
Potential problems
Side effects
In addition to blocking the nerves which carry pain, local anesthetic drugs in the epidural space will block other types of nerves as well, in a dose-dependent manner. Depending on the drug and dose used, the effects may last only a few minutes or up to several hours. This results in three main effects:[8]
- Loss of other modalities of sensation (including touch, and proprioception)
- Loss of muscle power
- Loss of function of the sympathetic nervous system, which controls blood pressure
- The leak of spinal fluid can cause headache in less than 1% of patients and it is corrected by using blood patch( injecting blood into epidural space).
- Very large doses of epidural anesthetic can cause paralysis of the intercostal muscles and diaphragm (which are responsible for breathing), and loss of sympathetic function to the heart itself, causing a profound drop in heart rate and blood pressure. This requires emergency treatment, and in severe cases may require airway support. This happens because the epidural is blocking the heart's sympathetic nerves, as well as the phrenic nerves, which supply the diaphragm.
Complications of epidural use
These include:
- Block failure (about 1 in 20). Partial failure may still give satisfactory pain relief. However, if pain relief is inadequate, another epidural may have to be performed.
- Bloody tap (about 1 in 30-50). It is easy to injure an epidural vein with the needle. In patients who have normal blood clotting, it is extremely rare (e.g. 1 in 100,000) for problems to develop. However, in a patient who has a coagulopathy, the patient may be at risk of epidural hematoma. If blood comes back down the needle, the anesthesiologist will normally site the epidural at another level.
- Accidental dural puncture with headache (common, about 1-3 in 100 insertions[32][33][34]) The epidural space in the adult lumbar spine is only 3-5mm deep, which means it is comparatively easy to cross it and accidentally puncture the dura (and arachnoid) with the needle. This may cause cerebrospinal fluid (CSF) to leak out into the epidural space, which may, in turn, cause the post dural puncture headache (PDPH). This can be severe and last several days and in some cases weeks or months. It is caused by a reduction in CSF pressure and is characterized by postural exacerbation when the patient raises their head above the lying position. If severe it may be successfully treated with a epidural blood patch (a small amount of the patient's own blood given into the epidural space via another epidural needle). Most cases resolve spontaneously with time.
- Catheter misplaced into a vein (uncommon, less than 1 in 300). Occasionally the catheter may be misplaced into an epidural vein, which results in all the anaesthetic being injected intravenously, where it can be toxic in large doses (about 1 in 10,000 insertions[35]). This also results in block failure.
- High block, as described above (uncommon, less than 1 in 500).
- Catheter misplaced into the subarachnoid space (rare, less than 1 in 1000). If the catheter is accidentally misplaced into the subarachnoid space (e.g. after an unrecognized accidental dural puncture), normally cerebrospinal fluid can be freely aspirated from the catheter (which would usually prompt the anesthetist to withdraw the catheter and resite it elsewhere). If, however, this is not recognized, large doses of anesthetic may be delivered directly into the cerebrospinal fluid. This may result in a high block, or, more rarely, a total spinal, where the anesthetic is delivered directly to the brainstem, causing unconsciousness and sometimes seizures.
- Neurological injury lasting less than 1 year (rare, about 1 in 6,700).[3]
- Epidural abscess formation (very rare, about 1 in 145,000).[4] The risk increases greatly with catheters which are left in place longer than 72 hours.
- Epidural haematoma formation (very rare, about 1 in 168,000).[5]
- Neurological injury lasting longer than 1 year (extremely rare, about 1 in 240,000).[6]
- Paraplegia (extremely rare, less than 1 in 100,000)[36].
- Arachnoiditis (extremely rare, fewer than 1000 cases in the past 50 years)[37]
- Death (extremely rare, less than 1 in 100,000)[38]) .
The figures above relate to epidurals in healthy individuals.
There is no evidence to support the concern that epidural analgesia increases the risk of anastomotic breakdown following bowel surgery[39].
Epidural analgesia in childbirth
Safety and efficacy
Epidural analgesia is a relatively safe method of relieving pain in labor. It provides rapid pain relief in most cases. It is more effective than nitrous oxide, opioids, TENS, and other common modalities of analgesia in childbirth.[7]
Prolonged labour and risk of instrumental delivery
- Epidural analgesia is associated with a longer labor, some researchers claim that it is correlated with an increased chance of operational intervention. The clinical research data on this topic are conflicting. For example, a study in Australia (Roberts, Tracy, Peat, 2000) concluded that having an epidural reduced the woman's chances of having a vaginal birth, without further interventions (such as episiotomy, forceps, ventouse or caesarean section) from 71.4% to 37.8%. Conversely, a 2001 study by researchers at the National Institute of Child Health and Human Development and a 2002 study by researchers at Cornell University and the University of Ontario demonstrated that epidurals do not increase the likelihood of a cesarean section. In 2005, a meta-analysis of 21 studies also showed that epidurals do not increase the likelihood of cesarean section, but they do increase the chance of a forceps or ventouse delivery by 40% (Anim-Somuah, Cochrane Review, 2005). The COMET Study, published in The Lancet in 2001 (vol358, No9275 p19-23) showed that a combined spinal-epidural in labor may speed up the labor process by a few minutes, although those women receiving an epidural had a cesarean rate of 28% and only 35% had a normal birth without instrument-assisted delivery.
These differing outcomes may be explained by data that demonstrates that the likelihood of increased intervention is directly related to the quality of the institution or practitioner providing the care: epidurals administered at top-rated institutions do not generally result in a clinically significant increase in cesarean rates, whereas the risk of cesarean delivery at poorly ranked facilities seems to increase with the use of epidural[40]
An alternative explanation is that women having difficult labors are more likely to request epidurals, and are also less likely to have an unassisted vaginal birth.
Effects on the baby
- Some mothers worry that epidural analgesia may harm their newborn. However, although epidural labor analgesia may be associated with slower progression of labor, it has no adverse effect on perinatal outcome and perinatal complications.[41]
- One study concluded that women whose epidurals contain the drug fentanyl were less likely to fully breastfeed their infant in the few days after birth and more likely to stop breastfeeding in the first 24 weeks.[42] However, this study has been criticized for several reasons, one of which is that the original patient records were not examined in this study, and so many of the epidurals were assumed to contain fentanyl when almost certainly they would not have.[43]
- In addition, all patients who used epidurals in labor had also used systemic pethidine, which would be much more likely to be the cause of any effect on breastfeeding due to the higher amounts of medication used via that route. If that were the case, then early epidurals which avoided the need for pethidine may actually improve breastfeeding outcomes, not worsen them.
Historical notes
- Prior to 1943, there were few methods of relieving pain in childbirth without risk of harm to the baby. Caesarean sections under general anesthesia was used only as an emergency measure. Dr. Robert A. Hingson, Dr. Waldo B. Edwards, and Dr. James L. Southworth working at the United States Marine Hospital at Stapleton, on Staten Island, New York, developed the technique of continuous caudal anesthesia.[44]
- In 1912, German physicians had found that the injection of an anesthetic, at the base of the spinal cord, would prevent pain impulses from reaching the brain. Doctors in the United States developed the technique further. For expectant mothers, the injection "only reduced the pangs of childbirth; it did not eliminate them," wrote Dr. Morris Fishbein in the March 1943 issue of Hygeia, and a single nerve-blocking injection was used only toward the end of labor.[44]
- Drs. Hingson and Southworth combined the concepts of caudal analgesia and the spinal injection in an operation to strip the varicose veins of a Scottish merchant seaman. The surgeons experimented with a continuous infusion of the local anesthetic, rather than removing the needle after the injection, to originate "continuous caudal analgesia". Dr. Hingson then collaborated with Dr. Edwards, the chief obstetrician at the Marine Hospital, to study the use of this technique in childbirth. The two studied the caudal region to determine where a needle could be safely placed to deliver anesthesia to the spinal nerves without placing the drugs into the spinal fluid.
- Testing on a human being did not occur until January 6, 1942, when the wife of a Coast Guardsman was brought into the Marine Hospital for delivery. Because the woman suffered from rheumatic heart disease, general anesthesia could not be safely used for an emergency Caesarean section, and it was believed that she would not survive the stress of labor. With the use of continuous local anesthesia, the woman and her baby survived. According to Dr. Fishbein's article in Hygeia, a total of 589 women in more than twenty participating hospitals gave birth relatively painlessly in 1942.[45]
- The results were published in the January 23, 1943, issue of the Journal of the American Medical Association.[46]
References
- ↑ de Lange JJ, Cuesta MA, Cuesta de Pedro A (May 1994). "Fidel Pagés Miravé (1886-1923). The pioneer of lumbar epidural anaesthesia". Anaesthesia. 49 (5): 429–31. doi:10.1111/j.1365-2044.1994.tb03480.x. PMID 8209988.
- ↑ 2.0 2.1 Waurick K, Waurick R (July 2015). "[History and Technique of Epidural Anaesthesia]". Anasthesiol Intensivmed Notfallmed Schmerzther (in German). 50 (7–8): 476–82, quiz 483. doi:10.1055/s-0041-100845. PMID 26230893.
- ↑ Dhansura T, Shaikh T, Maadoo M, Chittalwala F (October 2015). "Identification of the epidural space-loss of resistance to saline: An inexpensive modification". Indian J Anaesth. 59 (10): 677–9. doi:10.4103/0019-5049.167483. PMC 4645360. PMID 26644619.
- ↑ Kim YJ, Cho HM, Yoon CS, Lee CK, Lee TY, Seok JP (April 2011). "Thoracic Epidural Anesthesia and Analgesia (TEA) in Patients with Rib Fractures". Korean J Thorac Cardiovasc Surg. 44 (2): 178–82. doi:10.5090/kjtcs.2011.44.2.178. PMC 3249296. PMID 22263147.
- ↑ Jensen CD, Stark JT, Jacobson LE, Powers JM, Leslie KL, Kinsella-Shaw JM, Joseph MF, Denegar CR (January 2018). "Implications of Thoracic Epidural Analgesia on Hospital Charges in Rib Fracture Patients". Pain Med. 19 (1): 160–168. doi:10.1093/pm/pnw353. PMID 28340013.
- ↑ Gimeno AM, Errando CL (February 2018). "Neuraxial Regional Anaesthesia in Patients with Active Infection and Sepsis: A Clinical Narrative Review". Turk J Anaesthesiol Reanim. 46 (1): 8–14. doi:10.5152/TJAR.2018.12979. PMC 5858898. PMID 30140495.
- ↑ Jeon YS, Lee JA, Choi JW, Kang EG, Jung HS, Kim HK, Shim BY, Park JH, Joo JD (May 2012). "Efficacy of epidural analgesia in patients with cancer pain: a retrospective observational study". Yonsei Med. J. 53 (3): 649–53. doi:10.3349/ymj.2012.53.3.649. PMC 3343439. PMID 22477012.
- ↑ 8.0 8.1 8.2 8.3 Silva M, Halpern SH (2010). "Epidural analgesia for labor: Current techniques". Local Reg Anesth. 3: 143–53. doi:10.2147/LRA.S10237. PMC 3417963. PMID 23144567.
- ↑ "Practice advisory for the prevention, diagnosis, and management of infectious complications associated with neuraxial techniques: a report by the American Society of Anesthesiologists Task Force on infectious complications associated with neuraxial techniques". Anesthesiology. 112 (3): 530–45. March 2010. doi:10.1097/ALN.0b013e3181c4c7d8. PMID 20051824.
- ↑ Shapiro A, Fredman B, Zohar E, Olsfanger D, Abu-Ras H, Jedeikin R (July 1998). "Alternating patient position following the induction of obstetric epidural analgesia does not affect local anaesthetic spread". Int J Obstet Anesth. 7 (3): 153–6. PMID 15321207.
- ↑ Vincent RD, Chestnut DH (September 1991). "Which position is more comfortable for the parturient during identification of the epidural space?". Int J Obstet Anesth. 1 (1): 9–11. PMID 15636789.
- ↑ Figueroa JJ, Basford JR, Low PA (May 2010). "Preventing and treating orthostatic hypotension: As easy as A, B, C". Cleve Clin J Med. 77 (5): 298–306. doi:10.3949/ccjm.77a.09118. PMC 2888469. PMID 20439562.
- ↑ Andrews PJ, Ackerman WE, Juneja MM (April 1993). "Aortocaval compression in the sitting and lateral decubitus positions during extradural catheter placement in the parturient". Can J Anaesth. 40 (4): 320–4. doi:10.1007/BF03009629. PMID 8485791.
- ↑ Yu S, Tan KK, Sng BL, Li S, Sia AT (September 2014). "Automatic identification of needle insertion site in epidural anesthesia with a cascading classifier". Ultrasound Med Biol. 40 (9): 1980–90. doi:10.1016/j.ultrasmedbio.2014.03.010. PMID 24972502.
- ↑ Cesur M, Alici HA, Erdem AF, Silbir F, Yuksek MS (November 2005). "Administration of local anesthetic through the epidural needle before catheter insertion improves the quality of anesthesia and reduces catheter-related complications". Anesth. Analg. 101 (5): 1501–5. doi:10.1213/01.ANE.0000181005.50958.1E. PMID 16244020.
- ↑ Schmoldt A, Benthe HF, Haberland G, Sinelnikova EM, Dvoretskova TV, Kagan ZS, Smith RC, Stricker CM, Otteni JC, Haberer JP, Share JB, Leber HW, Geissler RH, Faber M, Post D (September 1975). "Digitoxin metabolism by rat liver microsomes". Biochem. Pharmacol. 24 (17): 1639–41. doi:10.2527/jas1975.4161674x. PMID 10.
- ↑ McNeill MJ, Thorburn J (February 1988). "Cannulation of the epidural space. A comparison of 18- and 16-gauge needles". Anaesthesia. 43 (2): 154–5. PMID 3354812.
- ↑ Norman D. Epidural analgesia using loss of resistance with air versus saline: does it make a difference? Should we reevaluate our practice? AANA J 2003;71:449-53. PMID 15098532
- ↑ Hobaika AB (2008). "Breakage of epidural catheters: etiology, prevention, and management". Rev Bras Anestesiol. 58 (3): 227–33. PMID 19378518.
- ↑ Aram L, Krane EJ, Kozloski LJ, Yaster M (June 2001). "Tunneled epidural catheters for prolonged analgesia in pediatric patients". Anesth. Analg. 92 (6): 1432–8. doi:10.1097/00000539-200106000-00016. PMID 11375820.
- ↑ Rawal N, Holmström B, Crowhurst JA, Van Zundert A (June 2000). "The combined spinal-epidural technique". Anesthesiol Clin North Am. 18 (2): 267–95. PMID 10935011.
- ↑ Lee EK, Tian H, Lee J, Wie X, Neeld J, Smith KD, Kaplan AR (2018). "Investigating a Needle-Based Epidural Procedure in Obstetric Anesthesia". AMIA Annu Symp Proc. 2018: 720–729. PMC 6371386. PMID 30815114.
- ↑ Kao SC, Lin CS (2017). "Caudal Epidural Block: An Updated Review of Anatomy and Techniques". Biomed Res Int. 2017: 9217145. doi:10.1155/2017/9217145. PMC 5346404. PMID 28337460.
- ↑ Klocke R, Jenkinson T, Glew D (November 2003). "Sonographically guided caudal epidural steroid injections". J Ultrasound Med. 22 (11): 1229–32. doi:10.7863/jum.2003.22.11.1229. PMID 14620894.
- ↑ Block BM, Liu SS, Rowlingson AJ, et al. (2003). Efficacy of postoperative epidural analgesia: A meta-analysis. JAMA, 290, 2455-2463.
- ↑ Ballantyne JC, Carr DB, deFerranti S, et al. (1998). The comparative effects of postoperative analgesic therapies on pulmonary outcome: cumulative meta-analyses of randomized, controlled trials. Anesth Analg, 86, 598-612.
- ↑ Allman KG, Wilson IH (eds) (2006). The Oxford Handbook of Anaesthesia, Oxford University Press, ISBN 0 19 856609 3, p. 1038
- ↑ Allman KG, Wilson IH (eds) (2006). The Oxford Handbook of Anaesthesia, Oxford University Press, ISBN 0 19 856609 3, p. 1038
- ↑ Allman KG, Wilson IH (eds) (2006). The Oxford Handbook of Anaesthesia, Oxford University Press, ISBN 0 19 856609 3, p. 1038
- ↑ Allman KG, Wilson IH (eds) (2006). The Oxford Handbook of Anaesthesia, Oxford University Press, ISBN 0 19 856609 3, p. 1038
- ↑ Rigg JRA, Jamrozik K, Myles PS, et al. (2002). Epidural anaesthesia and analgesia and outcome of major surgery: a randomised trial. Lancet 359, 1276-1282.
- ↑ Norris MC, Leighton BL, DeSimone CA. Needle bevel direction and headache after inadvertent dural puncture. Anesthesiology 1989;70:729-31.
- ↑ Sprigge JS, Harper SJ "Accidental dural puncture and post-dural puncture headache in obstetric anesthesia" Anaesthesia. 2008 Jan;63(1):36-43.
- ↑ Allman KG, Wilson IH (eds) (2006). The Oxford Handbook of Anaesthesia, Oxford University Press, ISBN 0 19 856609 3, p. 20
- ↑ Allman KG, Wilson IH (eds) (2006). The Oxford Handbook of Anaesthesia, Oxford University Press, ISBN 0 19 856609 3, p. 20
- ↑ Allman KG, Wilson IH (eds) (2006). The Oxford Handbook of Anaesthesia, Oxford University Press, ISBN 0 19 856609 3, p. 21
- ↑ Rice I, Wee MY, Thomson K., Obstetric epidurals and chronic adhesive arachnoiditis, Br J Anaesth. 2004 Jan;92(1):109-20. PMID 14665562
- ↑ Allman KG, Wilson IH (eds) (2006). The Oxford Handbook of Anaesthesia, Oxford University Press, ISBN 0 19 856609 3, p. 21
- ↑ Allman KG, Wilson IH (eds) (2006). The Oxford Handbook of Anaesthesia, Oxford University Press, ISBN 0 19 856609 3, p. 1039
- ↑ Thorp JA, Breedlove G. Epidural analgesia in labor: an evaluation of risks and benefits. Birth. 1996 Jun;23(2):63-83. PMID 8826170.
- ↑ Sieńko J, Czajkowski K, Swiatek-Zdzienicka M, Krawczyńska-Wichrzycka R., Epidural analgesia and the course of delivery in term primiparas, Ginekol Pol. 2005 Oct;76(10):806-11. PMID 16417096
- ↑ Torvaldsen S, Roberts CL, Simpson JM, Thompson JF, Ellwood DA., Intrapartum epidural analgesia, and breastfeeding: a prospective cohort study. Int Breastfeed J. 2006 Dec 11;1:24. PMID 17134489
- ↑ Camann, W. Labour analgesia and breastfeeding: avoid parenteral narcotics and provide lactation support Int J. of Obstetric Anesthesia 2007 16;199:201. PMID 17521903
- ↑ 44.0 44.1 "Robert A. Hingson, et al." Current Biography 1943, pp300-04
- ↑ Current Biography 1943, p301
- ↑ "Childbirth Made Painless and Safe By New Methods," AP article by Willis Young, reprinted in Oakland Tribune, January 21, 1943
Other reading
- Roberts C, Tracy S, Peat B,Rates for obstetric intervention among private and public patients in Australia: population-based descriptive study, British Medical Journal (BMJ), v321:p137, 15 July 2000
- Jun Zhang, Michael K. Yancey, Mark A. Klebanoff, Jenifer Schwarz and Dina Schweitzer, Does epidural analgesia prolong labor and increase risk of cesarean delivery? A natural experiment, American Journal of Obstetrics and Gynecology, Volume 185, Issue 1, July 2001, Pages 128-134.[8]
- Barbara L. Leighton and Stephen H. Halpern, The effects of epidural analgesia on labor, maternal, and neonatal outcomes: A systematic review, American Journal of Obstetrics and Gynecology, Volume 186, Issue 5, Part 2, May 2002, Pages S69-S77. Also available online.
- Boqing Chen and Patrick M. Foye, UMDNJ: New Jersey Medical School, Epidural Steroid Injections: Non-surgical Treatment of Spine Pain, eMedicine: Physical Medicine and Rehabilitation (PM&R), August 2005. Also available online.
da:Epiduralblokade de:Periduralanästhesie it:Anestesia peridurale he:אפידורל nl:Peridurale anesthesie sl:Epiduralna anestezija