Crohn's disease causes
|
Crohn's disease |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Crohn's disease causes On the Web |
|
American Roentgen Ray Society Images of Crohn's disease causes |
|
Risk calculators and risk factors for Crohn's disease causes |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Several theories exist about what causes Crohn’s disease, but none have been proven. The human immune system is made from cells and different proteins that protect people from infection. The most popular theory is that the body’s immune system reacts abnormally in people with Crohn’s disease, mistaking bacteria, foods, and other substances for being foreign. The immune system’s response is to attack these “invaders.” During this process, white blood cells accumulate in the lining of the intestines, producing chronic inflammation, which leads to ulcerations and bowel injury.[1] and with susceptibility to certain phenotypes of disease location and activity.[2]
Causes
The exact cause of Crohn's disease is unknown. However, genetic and environmental factors have been invoked in the pathogenesis of the disease. Research has indicated that Crohn's disease has a strong genetic link. [3] The disease runs in families and those with a sibling with the disease are 30 times more likely to develop it than the normal population.
Scientists do not know if the abnormality in the functioning of the immune system in people with Crohn’s disease is a cause, or a result, of the disease. Research shows that the inflammation seen in the GI tract of people with Crohn’s disease involves several factors: the genes the patient has inherited, the immune system itself, and the environment. Foreign substances, also referred to as antigens, are found in the environment. One possible cause for inflammation may be the body’s reaction to these antigens, or that the antigens themselves are the cause for the inflammation.
- Scientists have found that high levels of a protein produced by the immune system, called tumor necrosis factor (TNF), are present in people with Crohn’s disease.
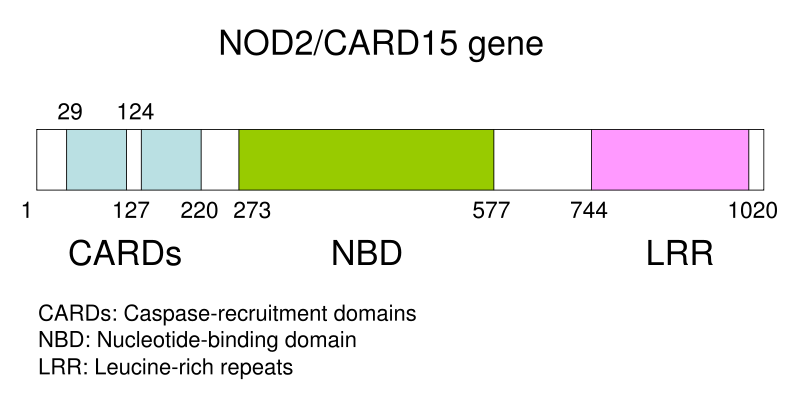
- Mutations in the CARD15 gene (also known as the NOD2 gene) are associated with Crohn's disease. In earlier studies, only two genes were linked to Crohn's, but scientists now believe there are over eight genes that show genetics play a crucial role in the disease. [4] and with susceptibility to certain phenotypes of disease location and activity.[5]
- Abnormalities in the immune system have often been invoked as being causes of Crohn's disease. It has been hypothesized that Crohn's disease involves augmentation of the Th1 of cytokine response in inflammation.[6] The most recent gene to be implicated in Crohn's disease is ATG16L1, which may reduce the effectiveness of autophagy, and hinder the body's ability to attack invasive bacteria.[7]
- A variety of pathogenic bacteria were initially suspected of being causative agents of Crohn's disease. However, the current consensus is that a variety of microorganisms are simply taking advantage of their host's weakened mucosal layer and inability to clear bacteria from the intestinal walls, both symptoms of the disease. [8] Some studies have linked Mycobacterium avium subsp. paratuberculosis to Crohn's disease, in part because it causes a very similar disease, Johne's disease, in cattle. [9]
- The mannose bearing antigens, mannins, from yeast may also elicit pathogenic anti saccharomyces cerevisiae antibodies.[10] Newer studies have linked specific strains of enteroadherent E. coli to the disease but failed to find evidence of contributions by other species. [11]
A handful of cases of Crohn's Disease cases were reported at the turn of the 20th century, but since then, the disease has continued to increase in prevalence dramatically. Some argue that this increase has been the result of a genetic shift in the population caused by conditions favoring individuals carrying the genes linked with the disease. These conditions could be a lower infant mortality rate or better health care in the nations that have the highest incidence of disease (industrialized nations).
References
- ↑ Ogura Y, Bonen DK, Inohara N, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. Nature. 2001 May 31;411(6837):603-6.
- ↑ Cuthbert A, Fisher S, Mirza M; et al. (2002). "The contribution of NOD2 gene mutations to the risk and site of disease in inflammatory bowel disease". Gastroenterology. 122 (4): 867–74. PMID 11910337.
- ↑ link Crohn's disease has strong genetic link: study
- ↑ Ogura Y, Bonen DK, Inohara N, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. Nature. 2001 May 31;411(6837):603-6.
- ↑ Cuthbert A, Fisher S, Mirza M; et al. (2002). "The contribution of NOD2 gene mutations to the risk and site of disease in inflammatory bowel disease". Gastroenterology. 122 (4): 867–74. PMID 11910337.
- ↑ Cobrin GM, Abreu MT. Defects in mucosal immunity leading to Crohn's disease. Immunol Rev. 2005 Aug;206:277-95. PMID 16048555
- ↑ Prescott NJ, Fisher SA, Franke A, Hampe J, Onnie CM, Soars D, Bagnall R, Mirza MM, Sanderson J, Forbes A, Mansfield JC, Lewis CM, Schreiber S, Mathew CG. A nonsynonymous SNP in ATG16L1 predisposes to ileal Crohn's disease and is independent of CARD15 and IBD5. Gastroenterology. 2007 May;132(5):1665-71. PMID: 17484864.
- ↑ Sartor, R. (2006). "Mechanisms of Disease: pathogenesis of Crohn's disease and ulcerative colitis". Nature Clinical Practice Gastroenterology & Hepatology (3): 390–407. doi:10.1038 Check
|doi=value (help). - ↑ Naser SA, Collins MT. Debate on the lack of evidence of Mycobacterium avium subsp. paratuberculosis in Crohn's disease. Inflamm Bowel Dis. 2005 Dec;11(12):1123. PMID 16306778
- ↑ Giaffer MH, Clark A, Holdsworth CD (1992). "Antibodies to Saccharomyces cerevisiae in patients with Crohn's disease and their possible pathogenic importance". Gut. 33 (8): 1071–5. PMID 1398231.
- ↑ Baumgart, M.; et al. (2007). "Culture independent analysis of ileal mucosa reveals a selective increase in invasive Escherichia coli of novel phylogeny relative to depletion of Clostridiales in Crohn's disease involving the ileum (advance online publication)". The ISME Journal. doi:10.1038 Check
|doi=value (help).