Chronic prostatitis/chronic pelvic pain syndrome
| Chronic Pelvic Pain Syndrome | ||
 | ||
|---|---|---|
| ICD-10 | N41.9 | |
| ICD-9 | 601.9 | |
| DiseasesDB | 10801 | |
| MedlinePlus | 000524 | |
| eMedicine | med/1922 | |
| MeSH | D011472 | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) is a pelvic pain condition in men, and should be distinguished from other forms of prostatitis such as chronic bacterial prostatitis and acute bacterial prostatitis.
Nomenclature
The name of this disorder is evolving. In 2007, the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) began using the umbrella term Urologic Chronic Pelvic Pain Syndromes (UCPPS), for research purposes, to refer to pain syndromes associated with the bladder (i.e. interstitial cystitis/painful bladder syndrome, IC/PBS) and the prostate gland (i.e. chronic prostatitis/chronic pelvic pain syndrome, CP/CPPS).[1]
Prevalence
The annual prevalence in the general population of chronic pelvic pain syndrome is 0.5%.[2] 38% of primary care providers, when presented with a vignette of a man with CPPS, indicate that they have never seen such a patient.[3] However, the overall prevalence of symptoms suggestive of CP/CPPS is 6.3%.[4] The role of the prostate was questoned in the etiology of CP/CPPS when both men and women in the general population were tested using the (1) National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) —with the female homolog of each male anatomical term use on questionnaires for female participants— (2) the International Prostate Symptom Score (IPSS), and (3) additional questions on pelvic pain. The prevalence of symptoms suggestive of CPPS in this selected population was 5.7% in women and 2.7% in men, placing in doubt the role of the prostate gland.[5]
Signs and symptoms
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is characterised by pelvic or perineal pain without evidence of urinary tract infection,[6] lasting longer than 3 months,[7] as the key symptom. Symptoms may wax and wane. Pain can range from mild discomfort to debilitating. Pain may radiate to back and rectum, making sitting difficult. Dysuria, arthralgia, myalgia, unexplained fatigue, abdominal pain, constant burning pain in the penis, and frequency may all be present. Frequent urination and increased urgency may suggest interstitial cystitis (inflammation centred in bladder rather than prostate). Ejaculation may be painful, as the prostate contracts during emission of semen, although nerve- and muscle-mediated post-ejaculatory pain is more common, and a classic sign of CP/CPPS. Some patients report low libido, sexual dysfunction and erectile difficulties. Pain after ejaculation is a very specific complaint that distinguishes CP/CPPS from men with BPH or normal men.
Theories of etiology
Nerves, stress and hormones
In 2008, a literature review for the years 1966 to 2003 was performed using the MEDLINE database of the United States National Library of Medicine, finding that the symptoms of CP/CPPS appear to result from an interplay between psychological factors and dysfunction in the immune, neurological and endocrine systems.[8]
Theories behind the disease include stress-driven hypothalamic-pituitary-adrenal axis dysfunction and adrenocortical hormone (endocrine) abnormalities,[9][10] neurogenic inflammation,[11][12][13] and myofascial pain syndrome.[14][15] In the latter two categories, dysregulation of the local nervous system due to past trauma, infection or an anxious disposition and chronic albeit unconscious pelvic tensing lead to inflammation that is mediated by substances released by nerve cells (such as substance P). The prostate (and other areas of the genitourinary tract: bladder, urethra, testicles) can become inflamed by the action of the chronically activated pelvic nerves on the mast cells at the end of the nerve pathways. Similar stress-induced genitourinary inflammation has been shown experimentally in other mammals.[16] However, there is no correlation between inflammation on histological examination of the prostate and the National Institutes of Health Chronic Prostatitis Symptom Index.[17]
The bacterial infection theory that for so long had held sway in this field was shown to be unimportant in a 2003 study from the University of Washington team led by Dr Lee and Professor Richard Berger. The study found that one third of both normal men and patients had equal counts of similar bacteria colonizing their prostates.[18] This view was endorsed by Dr Anthony Schaeffer, Professor and Chairman of the Department of Urology at Northwestern University, in a 2003 editorial of The Journal of Urology, in which he stated that "...these data suggest that bacteria do not have a significant role in the development of the chronic pelvic pain syndrome",[19] and a year later with his colleagues he published studies showing that antibiotics are essentially useless for CP/CPPS.[20][21] Since the publication of these studies, the research focus has shifted from infection to neuromuscular, behavioral, psychological, and genetic etiologies for UCPPS (CP/CPPS and IC/PBS), where the interplay between the lower urinary tract and other physiological systems is stressed.[22] UCPPS is now studied as a systemic disorder.[22] In support of this approach, a 2005 study showed that stress is correlated to Cat III prostatitis.[23]
Overlap with interstitial cystitis
Some researchers have suggested that CPPS is a form of interstitial cystitis/painful bladder syndrome (IC/PBS). A large multicenter prospective randomized controlled study showed that Elmiron was slightly better than placebo in treating the symptoms of CPPS, however the primary endpoint did not reach statistical significance.[24] Other therapies shown more effective than Elmiron in treating interstitial cystitis, such as quercetin and Elavil (amitriptyline), can help with chronic prostatitis. In 2007 the NIDDK began to group IC/PBS and CP/CPPS under the umbrella term Urologic Chronic Pelvic Pain Syndromes (UCPPS).
Infection
Additional theories and observations include:
Nanobacteria
In a preliminary 2005 open label study of 16 treatment-recalcitrant CPPS patients, controversial entities known as nanobacteria were proposed as a cause of prostatic calcification and symptoms found in CPPS.[25] Patients were treated with EDTA (to dissolve the calcifications) and 3 months of tetracycline (a calcium-leaching antibiotic with anti-inflammatory effects,[26] used here to kill the "pathogens"), and half had significant improvement in symptoms. Scientists have expressed strong doubts about whether nanobacteria are living organisms.[27][28] Research in 2008 showed that "nanobacteria" are merely tiny lumps of abiotic limestone.[29][30] Confirmation of the clinical efficacy of the treatment awaits placebo controlled studies.
Viruses
The evidence supporting a viral cause of prostatitis and chronic pelvic pain syndrome is weak. Single case reports have implicated Herpes simplex virus (HSV) and Cytomegalovirus (CMV) but a study using PCR failed to demonstrate the presence of viral DNA in patients with chronic pelvic pain syndrome undergoing radical prostatectomy for localized prostate cancer.[31] The reports implicating CMV must be interpreted with caution because in all cases the patients were immunocompromised.[32][33][34] For HSV the evidence is weaker still and there is only one reported case and the causative role of the virus was not proven,[35] and there are no reports of successful treatments using antiviral drugs such as aciclovir.
Diagnosis
There are no definitive diagnostic tests for CP/CPPS. This is a poorly understood disorder, even though it accounts for 90%-95% of prostatitis diagnoses.[36] It is found in men of any age, with the peak onset in the early 30s. CP/CPPS may be inflammatory (Category IIIa) or non-inflammatory (Category IIIb), based on levels of pus cells in expressed prostatic secretions, but these subcategories are of limited use clinically. In the inflammatory form, urine, semen, and other fluids from the prostate contain pus cells (dead white blood cells or WBCs), whereas in the non-inflammatory form no pus cells are present. Recent studies have questioned the distinction between categories IIIa and IIIb, since both categories show evidence of inflammation if pus cells are ignored and other more subtle signs of inflammation, like cytokines, are measured. In 2006, Chinese researchers found that men with categories IIIa and IIIb both had significantly and similarly raised levels of anti-inflammatory cytokine TGFβ1 and pro-inflammatory cytokine IFN-γ in their expressed prostatic secretions when compared with controls; therefore measurement of these cytokines could be used to diagnose category III prostatitis.[37]
For CP/CPPS patients, analysis of urine and expressed prostatic secretions for leukocytes is debatable, especially due to the fact that the differentiation between patients with inflammatory and non-inflammatory subgroups of CP/CPPS may not be useful.[38] Serum PSA tests, routine imaging of the prostate, and tests for Chlamydia trachomatis and Ureaplasma are not really proven to provide benefit for the patient.[38]
Extraprostatic abdominal/pelvic tenderness is present in half of the patients with chronic pelvic pain syndrome but only 7% of controls.[39]
Normal men have slightly more bacteria in their semen than men with CPPS.[40] The traditional Stamey 4-glass test is invalid for diagnosis of this disorder, and inflammation cannot be localized to any particular area of the lower GU tract.[40]
Men with CP/CPPS are more likely than the general population to suffer from Chronic Fatigue Syndrome (CFS),[41] and Irritable Bowel Syndrome (IBS). Prostate specific antigen levels may be elevated, although there is no malignancy.
Experimental tests that could be useful in the future include tests to measure semen and prostate fluid cytokine levels. Various studies have shown increases in markers for inflammation such as elevated levels of cytokines, myeloperoxidase, and chemokines.
Bladder neck hypertrophy and urethral stricture may both cause similar symptoms through urinary reflux (inter alia), and can be excluded through flexible cytoscopy and urodynamic tests.[42][43][44]
Treatment
A 2007 review article by Drs Potts and Payne in the Cleveland Clinic Journal of Medicine states:
"Indeed, chronic abacterial prostatitis (also known as chronic pelvic pain syndrome) is both the most prevalent form and also the least understood and the most challenging to evaluate and treat. This form of prostatitis may respond to non-prostate-centered treatment strategies such as physical therapy, myofascial trigger point release, and relaxation techniques."[45]
Physical and psychological therapy
For chronic nonbacterial prostatitis (Cat III), also known as CP/CPPS, which makes up the majority of men diagnosed with "prostatitis", a treatment called the "Stanford Protocol",[46], has recently been published. This is a combination of medication (using tricyclic antidepressants and benzodiazepines), psychological therapy (paradoxical relaxation, an advancement and adaptation, specifically for pelvic pain, of a type of progressive relaxation technique developed by Edmund Jacobson during the early 20th century), and physical therapy (trigger point release therapy on pelvic floor and abdominal muscles, and also yoga-type exercises with the aim of relaxing pelvic floor and abdominal muscles).[14][15] While these studies are encouraging, definitive proof of efficacy would require a randomized, sham controlled, blinded study, which is not as easy to do with physical therapy as with drug therapy.
Cat. III prostatitis may have no initial trigger other than anxiety, often with an element of Obsessive Compulsive Disorder or other anxiety-spectrum problem. This is theorized to leave the pelvic area in a sensitized condition resulting in a loop of muscle tension and heightened neurological feedback (neural wind-up). Current protocols largely focus on stretches to release overtensed muscles in the pelvic or anal area (commonly referred to as trigger points), physical therapy to the area, and progressive relaxation therapy to reduce causative stress. Biofeedback physical therapy to relearn how to control pelvic floor muscles may be useful.[47]
Aerobic exercise can help those sufferers who are not also suffering from Chronic Fatigue Syndrome (CFS) or whose symptoms are not exacerbated by exercise.[48] Acupuncture has reportedly benefited some patients.[49]
Food allergies
Anecdotal evidence suggests that food allergies and intolerances may have a role in exacerbating CP/CPPS, perhaps through mast cell mediated mechanisms. Specifically patients with gluten intolerance or celiac disease report severe symptom flares after sustained gluten ingestion. Patients may therefore find an exclusion diet helpful in lessening symptoms by identifying problem foods. Studies are lacking in this area.
Pharmacological treatment
There is a substantial list of medications used to treat this disorder.[50]
- The effectiveness of alpha blockers (tamsulosin, alfuzosin) is questionable in men with CPPS. A 2006 meta analysis found that they are moderately beneficial when the duration of therapy was at least 3 months.[51] However a 2004 trial found no benefit from alfuzosin during 6 weeks of treatment[20] and a 2008 clinical trial of alfuzosin found it was no better than placebo for treating CPPS in treatment naive recently diagnosed men.[52]
- Quercetin has shown effective in a randomized, placebo-controlled trial in chronic prostatitis using 500 mg twice a day for 4 weeks[53] Subsequent studies showed that quercetin, a mast cell inhibitor, reduces inflammation and oxidative stress in the prostate.
- Pollen extract (Cernilton) has also been shown effective in randomized placebo controlled trials.[54]
- Commonly used therapies that have not been properly evaluated in clinical trials are dietary modification, gabapentin, and amitriptyline.
- Therapies shown to be ineffective by randomized placebo/sham controlled trials: levaquin (antibiotics), alpha blockers for 6 weeks or less, transurethral needle ablation of the prostate (TUNA).
- At least one study suggests that multi-modal therapy (aimed at different pathways such as inflammation and neuromuscular dysfunction simultaneously) is better long term than monotherapy.[55]
- Antibiotics are generally not recommended.[21] Any improvement on antibiotics is likely to be evanescent, and due to the anti-inflammatory effects of the antibiotic.[56]
Surgery
Surgery (including minimally invasive) is recommended only for definitive indications and not generally for CP/CPPS.[57]
Prognosis
In recent years the prognosis for CP/CPPS has improved greatly with the advent of multimodal treatment, phytotherapy and protocols aimed at quieting the pelvic nerves through myofascial trigger point release and anxiety control.
See also
- Interstitial cystitis — a related disease.
- Myofascial Pain Syndrome
- Myofascial Release
- Neuromuscular Therapy
- Trigger Points
- Pelvic myoneuropathy
External links
- The Urologic Chronic Pelvic Pain Syndrome Society
- The Sex Destroyer — article at Men's Health gives a layman's overview of current developments
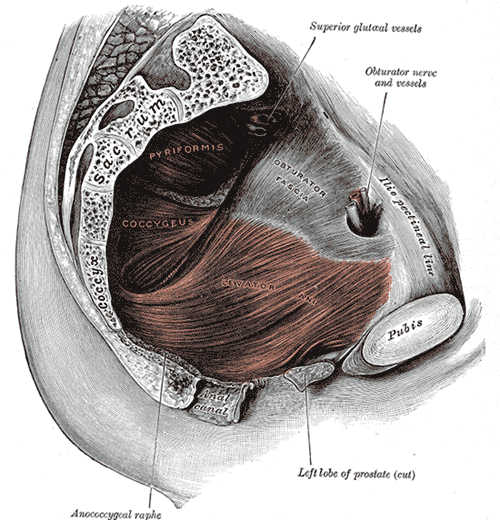
- Diagrams of the Pelvic Floor Muscles - pelvic musculature involved in causing CP/CPPS symptoms.
- Template:Dmoz
References
- ↑ "Multi-disciplinary Approach to the Study of Chronic Pelvic Pain (MAPP) Research Network". NIDDK. 2007. Retrieved 2008-01-11.
- ↑ Taylor BC, Noorbaloochi S, McNaughton-Collins M; et al. (2008). "Excessive antibiotic use in men with prostatitis". Am. J. Med. 121 (5): 444–9. doi:10.1016/j.amjmed.2008.01.043. PMC 2409146. PMID 18456041. Unknown parameter
|month=ignored (help) - ↑ Phillp Hannno. "Defining The Urologic Chronic Pelvic Pain Syndromes: A New Beginning - An International Symposium". Urotoday. Retrieved 2008-07-22.
- ↑ Daniels NA, Link CL, Barry MJ, McKinlay JB (2007). "Association between past urinary tract infections and current symptoms suggestive of chronic prostatitis/chronic pelvic pain syndrome". J Natl Med Assoc. 99 (5): 509–16. PMID 17534008. Unknown parameter
|month=ignored (help) - ↑ Marszalek M, Wehrberger C, Temml C, Ponholzer A, Berger I, Madersbacher S (2008). "Chronic Pelvic Pain and Lower Urinary Tract Symptoms in Both Sexes: Analysis of 2749 Participants of an Urban Health Screening Project". Eur. Urol. doi:10.1016/j.eururo.2008.03.073. PMID 18395963. Unknown parameter
|month=ignored (help) - ↑ Schaeffer AJ (2007). "Epidemiology and evaluation of chronic pelvic pain syndrome in men". Int J Antimicrob Agents: 108. doi:10.1016/j.ijantimicag.2007.08.027. PMID 18164597.
- ↑ Luzzi GA (2002). "Chronic prostatitis and chronic pelvic pain in men: aetiology, diagnosis and management". Journal of the European Academy of Dermatology and Venereology : JEADV. 16 (3): 253–6. PMID 12195565.
- ↑ Pontari MA, Ruggieri MR (2008). "Mechanisms in prostatitis/chronic pelvic pain syndrome". J. Urol. 179 (5 Suppl): S61–7. doi:10.1016/j.juro.2008.03.139. PMID 18405756. Unknown parameter
|month=ignored (help) - ↑ Anderson RU, Orenberg EK, Chan CA, Morey A, Flores V (2008). "Psychometric Profiles and Hypothalamic-Pituitary-Adrenal Axis Function in Men With Chronic Prostatitis/Chronic Pelvic Pain Syndrome". J Urol: 956. doi:10.1016/j.juro.2007.10.084. PMID 18207189.
- ↑ Dimitrakov J, Joffe HV, Soldin SJ, Bolus R, Buffington CA, Nickel JC (2008). "Adrenocortical Hormone Abnormalities in Men with Chronic Prostatitis/Chronic Pelvic Pain Syndrome". Urology. 71 (2): 261–266. doi:10.1016/j.urology.2007.09.025. PMID 18308097.
- ↑ Theoharides TC, Cochrane DE (2004). "Critical role of mast cells in inflammatory diseases and the effect of acute stress". J. Neuroimmunol. 146 (1–2): 1–12. doi:10.1016/j.jneuroim.2003.10.041. PMID 14698841.
- ↑ Theoharides TC, Kalogeromitros D (2006). "The critical role of mast cells in allergy and inflammation". Ann. N. Y. Acad. Sci. 1088: 78–99. doi:10.1196/annals.1366.025. PMID 17192558.
- ↑ Sant GR, Kempuraj D, Marchand JE, Theoharides TC (2007). "The mast cell in interstitial cystitis: role in pathophysiology and pathogenesis". Urology. 69 (4 Suppl): 34–40. doi:10.1016/j.urology.2006.08.1109. PMID 17462477.
- ↑ 14.0 14.1 Anderson RU, Wise D, Sawyer T, Chan C (2005). "Integration of myofascial trigger point release and paradoxical relaxation training treatment of chronic pelvic pain in men". J. Urol. 174 (1): 155–60. doi:10.1097/01.ju.0000161609.31185.d5. PMID 15947608.
- ↑ 15.0 15.1 Anderson RU, Wise D, Sawyer T, Chan CA (2006). "Sexual dysfunction in men with chronic prostatitis/chronic pelvic pain syndrome: improvement after trigger point release and paradoxical relaxation training". J. Urol. 176 (4 Pt 1): 1534–8, discussion 1538–9. doi:10.1016/j.juro.2006.06.010. PMID 16952676.
- ↑ Alexacos N, Pang X, Boucher W, Cochrane DE, Sant GR, Theoharides TC (1999). "Neurotensin mediates rat bladder mast cell degranulation triggered by acute psychological stress". Urology. 53 (5): 1035–40. doi:10.1016/S0090-4295(98)00627-X. PMID 10223502.
- ↑ Nickel JC, Roehrborn CG, O'leary MP, Bostwick DG, Somerville MC, Rittmaster RS (2007). "Examination of the relationship between symptoms of prostatitis and histological inflammation: baseline data from the REDUCE chemoprevention trial". J. Urol. 178 (3 Pt 1): 896–900, discussion 900–1. doi:10.1016/j.juro.2007.05.041. PMID 17632164.
- ↑ Lee JC, Muller CH, Rothman I; et al. (2003). "Prostate biopsy culture findings of men with chronic pelvic pain syndrome do not differ from those of healthy controls". J. Urol. 169 (2): 584–7, discussion 587–8. doi:10.1097/01.ju.0000045673.02542.7a. PMID 12544312. Unknown parameter
|month=ignored (help) - ↑ Schaeffer AJ (2003). "Editorial: Emerging concepts in the management of prostatitis/chronic pelvic pain syndrome". J Urol. 169 (2): 597-598. doi:10.1016/S0022-5347(05)63961-4. PMID 12544315. More than one of
|pages=and|page=specified (help) - ↑ 20.0 20.1 Alexander RB, Propert KJ, Schaeffer AJ; et al. (2004). "Ciprofloxacin or tamsulosin in men with chronic prostatitis/chronic pelvic pain syndrome: a randomized, double-blind trial". Ann. Intern. Med. 141 (8): 581–9. PMID 15492337.
- ↑ 21.0 21.1 Nickel JC, Downey J, Clark J; et al. (2003). "Levofloxacin for chronic prostatitis/chronic pelvic pain syndrome in men: a randomized placebo-controlled multicenter trial". Urology. 62 (4): 614–7. doi:10.1016/S0090-4295(03)00583-1. PMID 14550427.
- ↑ 22.0 22.1 "Multi-disciplinary Approach to the Study of Chronic Pelvic Pain". NIDDK - Department of Health and Human Services. 2007. Retrieved 2008-02-12.
- ↑ Ullrich PM, Turner JA, Ciol M, Berger R (2005). "Stress is associated with subsequent pain and disability among men with nonbacterial prostatitis/pelvic pain". Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 30 (2): 112–8. doi:10.1207/s15324796abm3002_3. PMID 16173907.
- ↑ Nickel JC, Forrest JB, Tomera K; et al. (2005). "Pentosan polysulfate sodium therapy for men with chronic pelvic pain syndrome: a multicenter, randomized, placebo controlled study". J. Urol. 173 (4): 1252–5. doi:10.1097/01.ju.0000159198.83103.01. PMID 15758763. Unknown parameter
|month=ignored (help) - ↑ Shoskes DA, Thomas KD, Gomez E (2005). "Anti-nanobacterial therapy for men with chronic prostatitis/chronic pelvic pain syndrome and prostatic stones: preliminary experience". J. Urol. 173 (2): 474–7. doi:10.1097/01.ju.0000150062.60633.b2. PMID 15643213.
- ↑ Rempe S, Hayden JM, Robbins RA, Hoyt JC (2007). "Tetracyclines and pulmonary inflammation". Endocr Metab Immune Disord Drug Targets. 7 (4): 232–6. PMID 18220943. Unknown parameter
|month=ignored (help) - ↑ Urbano P, Urbano F (2007). "Nanobacteria: facts or fancies?". PLoS Pathogens. 3 (5): e55. doi:10.1371/journal.ppat.0030055. PMID 17530922.
- ↑ Urbano P, Urbano F (2007). "Nanobacteria: Facts or Fancies?". PLoS Pathogens. Retrieved 2008-01-15.
- ↑ Michael Hopkin (2008). "Nanobacteria theory takes a hit". Nature. Retrieved 2008-04-29.
- ↑ Martel J, Young JD (2008). "Purported nanobacteria in human blood as calcium carbonate nanoparticles". Proc. Natl. Acad. Sci. U.S.A. 105 (14): 5549–54. doi:10.1073/pnas.0711744105. PMID 18385376. Unknown parameter
|month=ignored (help) - ↑ Leskinen MJ, Vainionp R, Syrjnen S; et al. (2003). "Herpes simplex virus, cytomegalovirus, and papillomavirus DNA are not found in patients with chronic pelvic pain syndrome undergoing radical prostatectomy for localized prostate cancer". Urology. 61 (2): 397–401. doi:10.1016/S0090-4295(02)02166-0. PMID 12597955.
- ↑ Benson PJ, Smith CS (1992). "Cytomegalovirus prostatitis". Urology. 40 (2): 165–7. doi:10.1016/0090-4295(92)90520-7. PMID 1323895.
- ↑ Mastroianni A, Coronado O, Manfredi R, Chiodo F, Scarani P (1996). "Acute cytomegalovirus prostatitis in AIDS". Genitourinary medicine. 72 (6): 447–8. PMID 9038649.
- ↑ McKay TC, Albala DM, Sendelbach K, Gattuso P (1994). "Cytomegalovirus prostatitis. Case report and review of the literature". International urology and nephrology. 26 (5): 535–40. PMID 7860201.
- ↑ Doble A, Harris JR, Taylor-Robinson D (1991). "Prostatodynia and herpes simplex virus infection". Urology. 38 (3): 247–8. doi:10.1016/S0090-4295(91)80355-B. PMID 1653479.
- ↑ Habermacher GM, Chason JT, Schaeffer AJ (2006). "Prostatitis/chronic pelvic pain syndrome". Annu. Rev. Med. 57: 195–206. doi:10.1146/annurev.med.57.011205.135654. PMID 16409145.
- ↑ Ding XG, Li SW, Zheng XM, Hu LQ (2006). "[IFN-gamma and TGF-beta1, levels in the expressed prostatic secretions of patients with chronic abacterial prostatitis]". Zhonghua Nan Ke Xue (in Chinese). 12 (11): 982–4. PMID 17146921.
- ↑ 38.0 38.1 Weidner W, Anderson RU (2007). "Evaluation of acute and chronic bacterial prostatitis and diagnostic management of chronic prostatitis/chronic pelvic pain syndrome with special reference to infection/inflammation". Int J Antimicrob Agents: 91. doi:10.1016/j.ijantimicag.2007.07.044. PMID 18162376.
- ↑ Shoskes DA, Berger R, Elmi A, Landis JR, Propert KJ, Zeitlin S (2008). "Muscle tenderness in men with chronic prostatitis/chronic pelvic pain syndrome: the chronic prostatitis cohort study". J. Urol. 179 (2): 556–60. doi:10.1016/j.juro.2007.09.088. PMID 18082223.
- ↑ 40.0 40.1 Nickel JC, Alexander RB, Schaeffer AJ, Landis JR, Knauss JS, Propert KJ (2003). "Leukocytes and bacteria in men with chronic prostatitis/chronic pelvic pain syndrome compared to asymptomatic controls". J. Urol. 170 (3): 818–22. doi:10.1097/01.ju.0000082252.49374.e9. PMID 12913707.
- ↑ Leslie A Aaron; et al. (2001). "Comorbid Clinical Conditions in Chronic Fatigue, A Co-Twin Control Study". J Gen Intern Med. 16 (1): 24-31. PMID 11251747.
- ↑ Chiari R (1983). "Urethral obstruction and prostatitis". Int Urol Nephrol. 15 (3): 245–55. doi:10.1007/BF02083011. PMID 6654631.
- ↑ Hruz P, Danuser H, Studer UE, Hochreiter WW (2003). "Non-inflammatory chronic pelvic pain syndrome can be caused by bladder neck hypertrophy". Eur. Urol. 44 (1): 106–10, discussion 110. doi:10.1016/S0302-2838(03)00203-3. PMID 12814683.
- ↑ Romero Pérez P, Mira Llinares A (1996). "[Complications of the lower urinary tract secondary to urethral stenosis]". Actas Urol Esp (in Spanish; Castilian). 20 (9): 786–93. PMID 9065088.
- ↑ Potts J, Payne RE (2007). "Prostatitis: Infection, neuromuscular disorder, or pain syndrome? Proper patient classification is key". Cleveland Clinic journal of medicine. 74 (Suppl 3): S63–71. PMID 17549825. Unknown parameter
|month=ignored (help) - ↑ "The Stanford Protocol". 2005. Retrieved 2006-12-09.
- ↑ Cornel EB, van Haarst EP, Schaarsberg RW, Geels J (2005). "The effect of biofeedback physical therapy in men with Chronic Pelvic Pain Syndrome Type III". Eur. Urol. 47 (5): 607–11. doi:10.1016/j.eururo.2004.12.014. PMID 15826751.
- ↑ Giubilei G, Mondaini N, Minervini A; et al. (2007). "Physical activity of men with chronic prostatitis/chronic pelvic pain syndrome not satisfied with conventional treatments--could it represent a valid option? The physical activity and male pelvic pain trial: a double-blind, randomized study". J. Urol. 177 (1): 159–65. doi:10.1016/j.juro.2006.08.107. PMID 17162029.
- ↑ Rosted P (2007). "Chronic prostatitis/chronic pelvic pain syndrome and acupuncture - a case report". Acupunct Med. 25 (4): 198–9. PMID 18160930.
- ↑ "Pharmacological treatment options for prostatitis/chronic pelvic pain syndrome". 2006. Retrieved 2006-12-11.
- ↑ Yang G, Wei Q, Li H, Yang Y, Zhang S, Dong Q (2006). "The effect of alpha-adrenergic antagonists in chronic prostatitis/chronic pelvic pain syndrome: a meta-analysis of randomized controlled trials". J. Androl. 27 (6): 847–52. doi:10.2164/jandrol.106.000661. PMID 16870951.
...treatment duration should be long enough (more than 3 months)
- ↑ Nickel JC, Krieger JN, McNaughton-Collins M; et al. (2008). "Alfuzosin and symptoms of chronic prostatitis-chronic pelvic pain syndrome". N. Engl. J. Med. 359 (25): 2663–73. doi:10.1056/NEJMoa0803240. PMID 19092152. Unknown parameter
|month=ignored (help) - ↑ Shoskes DA, Zeitlin SI, Shahed A, Rajfer J (1999). "Quercetin in men with category III chronic prostatitis: a preliminary prospective, double-blind, placebo-controlled trial". Urology. 54 (6): 960–3. doi:10.1016/S0090-4295(99)00358-1. PMID 10604689.
- ↑ Elist J (2006). "Effects of pollen extract preparation Prostat/Poltit on lower urinary tract symptoms in patients with chronic nonbacterial prostatitis/chronic pelvic pain syndrome: a randomized, double-blind, placebo-controlled study". Urology. 67 (1): 60–3. doi:10.1016/j.urology.2005.07.035. PMID 16413333.
- ↑ Potts JM (2005). "Therapeutic options for chronic prostatitis/chronic pelvic pain syndrome". Current urology reports. 6 (4): 313–7. doi:10.1007/s11934-005-0030-5. PMID 15978236.
- ↑ Hua VN, Williams DH, Schaeffer AJ (2005). "Role of bacteria in chronic prostatitis/chronic pelvic pain syndrome". Curr Urol Rep. 6 (4): 300–6. doi:10.1007/s11934-005-0028-z. PMID 15978234.
- ↑ Nickel JC (2007). "Treatment of chronic prostatitis/chronic pelvic pain syndrome". Int J Antimicrob Agents: 112. doi:10.1016/j.ijantimicag.2007.07.028. PMID 17954024.
Template:Diseases of the pelvis, genitals and breasts
de:Prostatitis it:Prostatite nl:Prostatitis fi:Eturauhasen tulehdus