Cefoxitin microbiology
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Abdurahman Khalil, M.D. [2]
Microbiology
Mechanism of Action
Cefoxitin is a bactericidal agent that acts by inhibition of bacterial cell wall synthesis. Cefoxitin has activity in the presence of some beta-lactamases, both penicillinases and cephalosporinases, of Gram-negative and Gram-positive bacteria.
Mechanism of Resistance
Resistance to Cefoxitin is primarily through hydrolysis by beta-lactamase, alteration of penicillin-binding proteins (PBPs), and decreased permeability.
Cefoxitin has been shown to be active against most isolates of the following bacteria, both in vitro and in clinical infections as described in theINDICATIONS AND USAGE section:
Gram-positive bacteria
Staphylococcus aureus Staphylococcus epidermidis Streptococcus agalactiae Streptococcus pneumoniae Streptococcus pyogenes
Gram-negative microorganisms
Escherichia coli Haemophilus influenzae Klebsiella spp. Morganella morganii Neisseria gonorrhoeae Proteus mirabilis Proteus vulgaris Providencia spp.
Anaerobic bacteria
Clostridium spp. Peptococcus niger Peptostreptococcus spp. Bacteroides distasonis Bacteroides fragilis Bacteroides ovatus Bacteroides thetaiotaomicron Bacteroides spp.
The following in vitro data are available, but their clinical significance is unknown. At least 90 percent of the following microorganisms exhibit an in vitrominimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoint for cefoxitin. However, the efficacy of cefoxitin in treating clinical infections due to these microorganisms has not been established in adequate and well-controlled clinical trials.
Gram-negative bacteria
Eikenella corrodens [non-β-lactamase producers]
Anaerobic bacteria
Clostridium perfringens Prevotella bivia
Susceptibility Test Methods
When available, the clinical microbiology laboratory should provide the results of in vitro susceptibility test results for antimicrobial drug products used in resident hospitals to the physician as periodic reports that describe the susceptibility profile of nosocomial and community-acquired pathogens. These reports should aid the physician in selecting an antibacterial drug product for treatment.
Dilution techniques
Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized test method 1,3. The MIC values should be interpreted according to criteria provided in Table 1.
Diffusion techniques
Quantitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. The zone size provides an estimate of the susceptibility of bacteria to antimicrobial compounds. The zone size should be determined using a standardized test method 2,3. This procedure uses paper disks impregnated with 30 mcg Cefoxitin to test the susceptibility of microorganisms to Cefoxitin. The disk diffusion interpretive criteria are provided in Table 1.
Table 1. Susceptibility Test Interpretive Criteria for Cefoxitin 2
A report of Susceptible indicates that the antimicrobial is likely to inhibit growth of the pathogen if the antimicrobial compound reaches the concentration at the infection site necessary to inhibit growth of the pathogen. A report of Intermediate indicates that the result should be considered equivocal, and if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where a high dosage of drug can be used. This category also provides a buffer zone that prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of Resistant indicates that the antimicrobial is not likely to inhibit growth of the pathogen if the antimicrobial compound reaches the concentrations usually achievable at the infection site; other therapy should be selected.
Quality Control
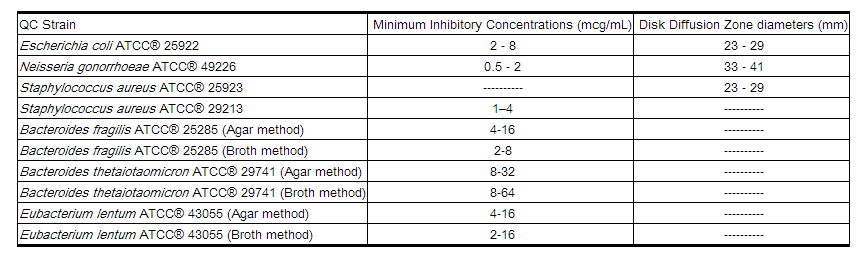
Standardized susceptibility test procedures require the use of laboratory controls to monitor and ensure the accuracy and precision of supplies and reagents used in the assay, and the techniques of the individual performing the test 1,2,3,4. Standard Cefoxitin powder should provide the following range of MIC values noted in Table 2. For the diffusion technique using the 30 mcg disk, the criteria in Table 2 should be achieved.
Table 2. Acceptable Quality Control Ranges for Cefoxitin
References
http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/065214s013lbl.pdf