Burn physical examination
|
Burn Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Burn physical examination On the Web |
|
American Roentgen Ray Society Images of Burn physical examination |
|
Risk calculators and risk factors for Burn physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Eman Alademi, M.D.[2]
Overview
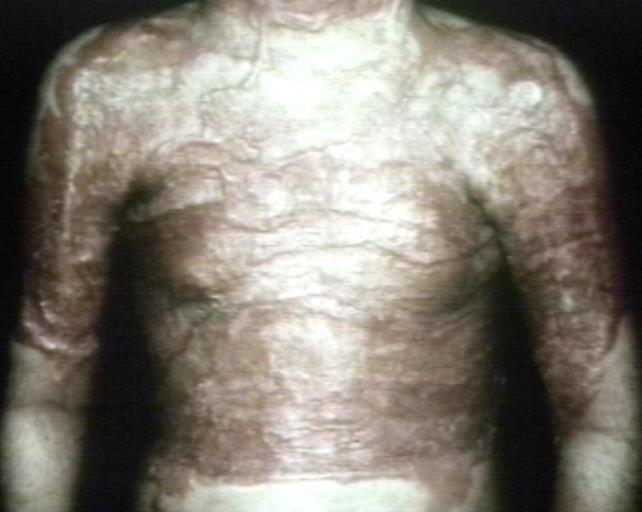
Patients with burn injury usually appear as burned(injury) skin . When a doctor or physician has been admitted burned patient, the diagnosis is usually known by physical examination of the patient. Physical examination of burn injury consists of a thorough of thickness and total body surface area of the patient body. Patient may be have burn on his head, neck, arm, leg, Anterior trunk,Posterior trunk, and genatilia.
Physical Examination
Key factors in the history include the type of burn, possible:
Inhalation injury: If possible, ask pre hospital emergency services providers if the patient had prolonged smoke exposure (consider carbon monoxide poisoning, cyanide poisoning, lung injury)
associated traumatic injuries: might have other injuries from explosions, falls or jumping to safety. Examination of the burn can be done in the patient's secondary survey.
The patient's clothing should be removed, and the patient should be examined from head to toe in a warm room.
Burn calcification:
Burns can divided in to: minor burns (most burns are small), or severe burns(major trauma patient) and serious burn injury.
- Partial-thickness burns greater than 10% of TBSA [1]Burns that involve the face, hands, feet, genitalia, perineum, or major joints
- Third-degree burns in any age group
- Electrical burns, including lightning injury
- Inhalation injury
- Burn injury in patients with preexisting medical disorders that could complicate management, prolong recovery, or affect mortality
- Any patient with burns and concomitant trauma (such as fractures) in which the burn injury poses the greatest risk for morbidity or mortality. In such cases, if the trauma poses the greater immediate risk, the patient may be stabilized initially in a trauma center before being transferred to a burn unit. Physician judgment will be necessary in such situations and should be in concert with the regional medical control plan and triage protocols.
- Burned children in hospitals without qualified personnel or equipment for the care of children[2][3]
- Burn injury in patients who will require special social, emotional, or rehabilitative intervention.
Burn evaluation:
The major factors to consider when evaluating the burned skin during a burn evaluation are :
1.An estimated percentage of total body surface area (TBSA) that has been burned(The extent of the burns (usually calculated by the percentage of total body surface area (% TBSA) burned).
2.An estimated depth of the burns (superficial, partial thickness or full thickness).[4][5][6][7][8]
Rule of nines estimates are not used for children. Their bodies have different proportions than adults. If your child has a burn that covers a medium to large area, your provider may use a chart, called a Lund-Browder chart, to make an estimate. This gives more accurate estimates based on a child's age and body size.
If you or your child has a burn that covers a small area, your provider may use an estimate based on the size of the palm, which is about 1% of TBSA.
In serious burn injury, you may also need an emergency evaluation known as an ABCDE assessment. ABCDE assessments are used to check key body systems and functions. They often take place in ambulances, emergency rooms, and hospitals. They are used for different types of traumatic emergencies, including severe burns.
"ABCDE" stands for the following checks:
- Airway: check for any blockages in your airway.
- Breathing: check for signs of trouble breathing, including coughing, rasping, or wheezing. The provider may use a stethoscope to monitor your breath sounds.
- Circulation. A provider will use devices to check your heart and blood pressure. Health provider insert a catheter into your vein. Burns can often cause serious fluid loss.
- Disability: A provider will check for signs of brain damage. This for checking to see how you respond to different verbal and physical stimulation.
- Exposure: A provider will remove any chemicals or burn-causing substances from the skin by flushing the injured area with water. the health provider may bandage the area with a sterile dressing. The provider will also check your temperature, and warm you with a blanket and warm fluids if necessary.[9]
Skin
Extent of the Burn
Burn evaluations are used to examine moderate to severe burn injuries
Several methods are available to estimate the percentage of total body surface area burned such as: the "rule of nines" to get this estimate, or Lund and Browder Chart.
The rule of nines :
Divides the body into sections of 9% or 18% (2 times 9). The sections are divided as follows:
- Head and neck: 9% of TBSA
- Each arm: 9% TBSA
- Each leg: 18% TBSA
- Anterior trunk (front of the body=the anterior chest and abdomen) 18% TBSA
- Posterior trunk (back of the body=chest and back) 18% TBSA
- the perineum is 1%
- Palmar Surface - For small burns, (excluding the fingers) represents approximately 0.5%, and (including the palm and fingers) represents about 1%.
Lund and Browder Chart:
This is a more accurate method, especially in children, where each arm is 10%, anterior trunk and posterior trunk are each 13% and the percentage calculated for the head and legs varies based on the patient’s age.
 |
 |
 |
 |
 |
Head

References
- ↑ Mertens DM, Jenkins ME, Warden GD (1997). "Outpatient burn management". Nurs Clin North Am. 32 (2): 343–64. PMID 9115481.
- ↑ Baxter CR (1993). "Management of burn wounds". Dermatol Clin. 11 (4): 709–14. PMID 8222354.
- ↑ Orgill DP (2009). "Excision and skin grafting of thermal burns". N Engl J Med. 360 (9): 893–901. doi:10.1056/NEJMct0804451. PMID 19246361.
- ↑ Grammatikopoulou MG, Theodoridis X, Gkiouras K, Stamouli EM, Mavrantoni ME, Dardavessis T, Bogdanos DP, Schmoldt A, Benthe HF, Haberland G, Holder AA, Wootton JC, Baron AJ, Chambers GK, Fincham JR, Longo DL, Herbert V (May 2019). "AGREEing on Guidelines for Nutrition Management of Adult Severe Burn Patients". JPEN J Parenter Enteral Nutr. 43 (4): 490–496. doi:10.1002/jpen.1452. PMID 30320409.
- ↑ Watson C, Troynikov O, Lingard H (June 2019). "Design considerations for low-level risk personal protective clothing: a review". Ind Health. 57 (3): 306–325. doi:10.2486/indhealth.2018-0040. PMC 6546585 Check
|pmc=value (help). PMID 30089764. - ↑ Johnson SP, Chung KC (May 2017). "Outcomes Assessment After Hand Burns": 389–397. doi:10.1016/j.hcl.2016.12.011. PMC 5380152.
- ↑ Beltran SL, Vilela RAG, de Almeida IM (2018) Challenging the immediate causes: A work accident investigation in an oil refinery using organizational analysis. Work 59 (4):617-636. DOI:10.3233/WOR-182702 PMID: 29733046 PMID: 29733046
- ↑ Devinck, F.; Deveaux, C.; Bennis, Y.; Deken-Delannoy, V.; Jeanne, M.; Martinot-Duquennoy, V.; Guerreschi, P.; Pasquesoone, L. (2018). "Les brûlures profondes par agents basiques : évaluation d'une stratégie chirurgicale en deux temps". Annales de Chirurgie Plastique Esthétique. 63 (3): 191–196. doi:10.1016/j.anplas.2018.03.008. ISSN 0294-1260.
- ↑ "Burn Evaluation: MedlinePlus Medical Test".