B cell
|
WikiDoc Resources for B cell |
|
Articles |
|---|
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on B cell at Clinical Trials.gov Clinical Trials on B cell at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on B cell
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating B cell Risk calculators and risk factors for B cell
|
|
Healthcare Provider Resources |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
B cells are lymphocytes that play a large role in the humoral immune response as opposed to the cell-mediated immune response that is governed by T cells. B cells are produced in the bone marrow of most mammals and are therefore called B cells. The principal function of B cells is to make antibodies against soluble antigens. B cells are an essential component of the adaptive immune system.
Development of B cells
B cells are produced in the bone marrow of most mammals. Rabbits are an exception; their B cells develop in the appendix-sacculus rotundus. B cell development occurs through several stages, each stage representing a change in the genome content at the antibody loci. An antibody is composed of two light (L) and two heavy (H) chains, and the genes specifying them are found in the 'H' chain locus and the 'L' chain locus. In the H chain loci there are three regions, V, D and J, which recombine randomly, in a process called VDJ recombination, to produce a unique variable domain in the immunoglobulin of each individual B cell. Similar rearrangements occur for L chain locus except there are only two regions, namely V and J. The list below describes the process of immunoglobulin formation at the different stages of B cell development.
- Progenitor B cells - Contains Germline H genes, Germline L genes
- Early Pro-B cells - undergoes D-J rearrangement on the H chains
- Late Pro-B cells - undergoes V-DJ rearrangement on the H chains
- Large Pre-B cells - the H chain is VDJ rearranged, Germline L genes
- Small Pre-B cells - undergoes V-J rearrangement on the L chains
- Immature B cells - VJ rearranged on L chains, VDJ rearranged on H chains. There is start of expression of IgM receptors.
- Mature B cells - There is start of expression of IgD
When the B cell fails in any step of the maturation process, it will die by a mechanism called apoptosis. If it recognizes self-antigen during the maturation process, the B cell will become suppressed (known as anergy) or undergo apoptosis (a process called negative selection). B cells are continuously produced in the bone marrow, but only a small portion of newly made B cells survive to participate in the long-lived peripheral B cell pool.
B cell membrane receptors on which drugs may be active evolve during the B cell life span [2]. CD20 is present on preB cells, but disappears in mature B cells. TACI, BCMA and BAFF-R are present on immature B cells and mature B cells. The agonist of these 3 receptors is inhibited by Belimumab
Functions
The human body makes millions of different types of B cells each day that circulate in the blood and lymph performing the role of immune surveillence. They do not produce antibodies until they become fully activated. Each B cell has a unique receptor protein (referred to as the B cell receptor (BCR)) on its surface that will bind to one particular antigen. The BCR is a membrane-bound immunoglobulin, and it is this molecule that allows the distinction of B cells from other types of lymphocyte, as well as being the main protein involved in B cell activation. Once a B cell encounters its cognate antigen and receives an additional signal from a T helper cell, it can further differentiate into one of the two types of B cells listed below. The B cell may either become one of these cell types directly or it may undergo an intermediate differentiation step, the germinal center reaction, where the B cell will hypermutate the variable region of its immunoglobulin gene ("somatic hypermutation") and possibly undergo class switching.
B cell types
- Plasma B cells (also known as plasma cells) are large B cells that have been exposed to antigen and are producing and secreting large amounts of antibodies, which assist in the destruction of microbes by binding to them and making them easier targets for phagocytes and activation of the complement system. They are sometimes referred to as antibody factories. An electron micrograph of these cells reveals large amounts of rough endoplasmic reticulum, responsible for synthesizing the antibody, in the cell's cytoplasm.
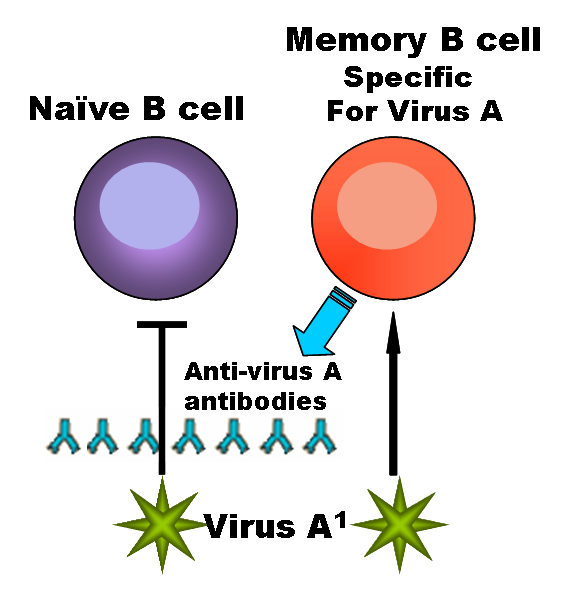
- Memory B cells are formed from activated B cells that are specific to the antigen encountered during the primary immune response. These cells are able to live for a long time, and can respond quickly following a second exposure to the same antigen.
- B-1 cells express IgM in greater quantities than IgG and its receptors show polyspecificity, meaning that they have low affinities for many different antigens, but have a preference for other immunoglobulins, self antigens and common bacterial polysaccharides. B-1 cells are present in low numbers in the lymph nodes and spleen and are instead found predominantly in the peritoneal and pleural cavities.
- B-2 cells are the conventional B cells most texts refer to.
Recognition of antigen by B cells
A critical difference between B cells and T cells is how each lymphocyte "sees" its antigen. B cells recognize their cognate antigen in its native form. They recognize free (soluble) antigen in the blood or lymph using their BCR or membrane bound-immunoglobulin. In contrast, T cells recognize their cognate antigen in a processed form, as a peptide fragment presented by an antigen presenting cell's MHC molecule to the T cell receptor.
Activation of B cells
B cell recognition of antigen is not the only element necessary for B cell activation (a combination of clonal proliferation and terminal differentiation into plasma cells). B cells that have not been exposed to antigen, also known as Naive B cells, can be activated in a T-cell dependent or independent manner.
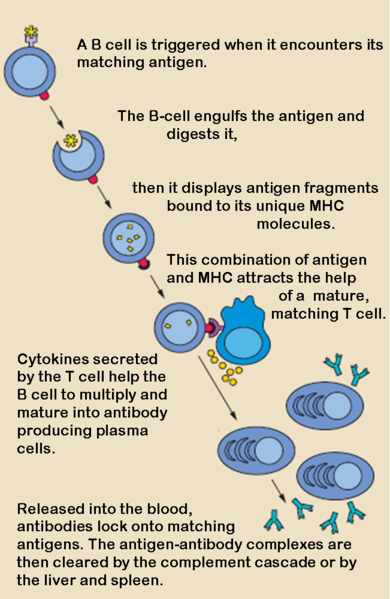
T-cell dependent activation
When a B cell ingests a pathogen, it attaches parts of the pathogen's proteins to a class II MHC protein. This complex is moved to the outside of the cell membrane, where it can be recognized by a T lymphocyte, which is compatible with similar structures on the cell membrane of a B lymphocyte. If the B cell and T cell structures match, the T lymphocyte activates the B lymphocyte, which produces antibodies against the bits of pathogen, called antigen, it has presented on its surface.
Most antigens are T-dependent, meaning T cell help is required for maximal antibody production. With a T-dependent antigen, the first signal comes from antigen cross linking the B cell receptor (BCR) and the second signal comes from co-stimulation provided by a T cell. T dependent antigens contain proteins that are presented on B cell Class II MHC to a special subtype of T cell called a Th2 cell. When a B cell processes and presents the same antigen to the primed Th cell, the T cell secretes cytokines that activate the B cell. These cytokines trigger B cell proliferation and differentiation into plasma cells. Isotype switching to IgG, IgA, and IgE and memory cell generation occur in response to T-dependent antigens. This isotype switching is known as Class Switch Recombination (CSR). Once this switch has occurred, that particular B-cell can no longer make the earlier isotypes, IgM or IgD.
T-cell independent activation
Many antigens are T-independent, meaning they can deliver both of the signals to the B cell. Mice without a thymus (nude or athymic mice that do not produce any T cells) can respond to T-independent antigens. Many bacteria have repeating carbohydrate epitopes that stimulate B cells, through so called pattern recognition receptors, to respond with IgM synthesis in the absence of T cell help. There are two types of T-cell independent activation; Type 1 T cell-independent (polyclonal) activation, and type 2 T cell-independent activation (in which macrophages present several of the same antigen in a way that causes cross-linking of antibodies on the surface of B cells).
The ancestral roots of B cells
In an October 2006 issue of Nature Immunology, it was reported that certain B-cells of primitive vertebrates (like fish and amphibians) are capable of phagocytosis, a function usually associated with cells of the innate immune system. The authors of this article postulate that these phagocytic B-cells represent the ancestral history shared between macrophages and lymphocytes; B-cells may have evolved from macrophage-like cells during the formation of the adaptive immune system[1].
B cells in humans (and other vertebrates) are nevertheless able to endocytose antibody-fixed pathogens, and it is through this route that MHC Class II presentation by B cells is possible, allowing Th2 help and stimulation of B cell proliferation. This is purely for the benefit of MHC Class II presentation, not as a significant method of reducing the pathogen load.
Origin of the word B-cell
The abbreviation "B" in B cell originally came from Bursa of Fabricius, an organ in birds in which avian B cells mature. When it was discovered that in most mammals B cells are formed in bone marrow, the word B cell continued to be appropriate. The fact that bone and bursa both start with the letter 'B' is a coincidence.
References
See also
External links
Acknowledgements
The content on this page was first contributed by: C. Michael Gibson, M.S., M.D.
List of contributors:
Suggested Reading and Key General References
Suggested Links and Web Resources
For Patients
da:B-celle de:B-Lymphozyt ko:B세포 he:לימפוציט B lt:B limfocitai nl:B-cel fi:B-solu sv:B-cell th:บีเซลล์