Antihemophilic factor (recombinant)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Shivani Chaparala M.B.B.S [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Antihemophilic factor (recombinant) is a blood coagulation factor VIII (Factor VIII) that is FDA approved for the treatment of * Hemophilia A for:
- On-demand treatment and control of bleeding episodes.
- Perioperative management of bleeding.
- Routine prophylaxis to reduce the frequency of bleeding episodes.. Common adverse reactions include paresthesia, headache, injection site inflammation, injection site pain, non-neutralizing anti-Factor VIII antibody formation, back pain, vertigo, and dry mouth..
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- Antihemophilic factor (recombinant) is a recombinant antihemophilic factor [blood coagulation factor VIII (Factor VIII)] indicated in adults and children with Hemophilia A for:
- On-demand treatment and control of bleeding episodes.
- Perioperative management of bleeding.
- Routine prophylaxis to reduce the frequency of bleeding episodes.
- Antihemophilic factor (recombinant) is not indicated for the treatment of von Willebrand Disease.
DOSAGE AND ADMINISTRATION
- For intravenous use after reconstitution
- Each vial of Antihemophilic factor (recombinant) is labeled with the actual amount of Factor VIII potency in international units (IU).
- Determine dose using the following formula for adolescents and adults:
- Required IU = body weight (kg) x desired Factor VIII rise (%) (IU/dL) x 0.5 (IU/kg per IU/dL)
- Dosing for routine prophylaxis:

- Frequency and duration of therapy depends on severity of the FVIII deficiency, location and extent of bleeding, and patient’s clinical condition.
DOSAGE FORMS AND STRENGTHS
- Antihemophilic factor (recombinant) is available as a white sterile, non-pyrogenic, lyophilized powder for reconstitution in single-use vials containing nominally 250, 500, 1000 or 2000 IU Factor VIII potency.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Antihemophilic factor (recombinant) in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Antihemophilic factor (recombinant) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)

Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Antihemophilic factor (recombinant) in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Antihemophilic factor (recombinant) in pediatric patients.
Contraindications
Antihemophilic factor (recombinant) is contraindicated in patients who have manifested life-threatening hypersensitivity reactions, including anaphylaxis, to the product or its components.
Warnings
Hypersensitivity Reactions
- Hypersensitivity reactions, including anaphylaxis, are possible with Antihemophilic factor (recombinant).
- Early signs of hypersensitivity reactions that can progress to anaphylaxis may include angioedema, chest tightness, dyspnea, wheezing, urticaria, or pruritus.
- Immediately discontinue administration and initiate appropriate treatment if hypersensitivity reactions occur.
Neutralizing Antibodies
- The formation of neutralizing antibodies (inhibitors) to Factor VIII can occur following the administration of Antihemophilic factor (recombinant).
- Monitor all patients for the development of Factor VIII inhibitors by appropriate clinical observations and laboratory tests.
- If the plasma Factor VIII level fails to increase as expected, or if bleeding is not controlled after Antihemophilic factor (recombinant) administration, suspect the presence of an inhibitor (neutralizing antibody).
Monitoring and Laboratory Tests
- Monitor plasma Factor VIII activity by performing a validated test (e.g., one stage clotting assay), to confirm that adequate Factor VIII levels have been achieved and maintained.
- Monitor for the development of Factor VIII inhibitors.
- Perform a Bethesda inhibitor assay if expected Factor VIII plasma levels are not attained, or if bleeding is not controlled with the expected dose of Antihemophilic factor (recombinant).
- Use Bethesda Units (BU) to report inhibitor levels.
Adverse Reactions
Clinical Trials Experience
- The most common adverse reactions (>0.5% of subjects) reported in clinical trials were paresthesia, headache, injection site inflammation, injection site pain, non-neutralizing anti-Factor VIII antibody formation, back pain, vertigo, and dry mouth.
Clinical Trial Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to the rate in the clinical trials of another drug and may not reflect the rates observed in practice.
- The safety profile of Antihemophilic factor (recombinant) was evaluated in five prospective, open-label clinical studies in previously treated patients (PTPs - exposed to a Factor VIII containing product for ≥150 exposure days (EDs) in the case of adolescents and adults or ≥50 EDs in the case of subjects below 12 years of age) with severe Hemophilia A (Factor VIII ≤ 1%).
- Subjects who had a history of detectable Factor VIII inhibitor, severe liver or kidney disease, were not immune competent (CD4+ count <200/µL), or scheduled to receive immunomodulating drugs, were excluded.
- Across all clinical studies, 135 patients were stratified, among them, 74 were adults, 3 adolescents between 12 and 17 years old, and 58 pediatric patients between 2 and 11 years old.
- A total of 127 (94.1%) subjects were treated for at least 180 days.
- Collectively, patients received between 24,005 and 996,550 IU (555 to 8629 IU/kg) from14 to 319 infusions over 14 to 299 exposure days, over a period of 33 to 563 days.
- An exposure day was defined as any day on which at least one infusion was started.
- With a total of 16,134 infusions over 15,950 EDs, reported adverse reactions included paresthesia, headache, injection site inflammation, injection site pain, back pain, vertigo, and dry mouth.
- Each of these adverse reactions occurred once in the study population of 135, and thus each had a rate of 0.7%.
- Non-neutralizing anti-Factor VIII antibodies (without inhibitory activity as measured by the modified Bethesda assay) were reported in four patients, giving a rate of 3%.
- Three of four subjects had pre-existing non-neutralizing antibodies prior to exposure with Antihemophilic factor (recombinant).
- The binding antibodies were transient in two of these three subjects.
- In one subject who was tested negative at screening, the non-neutralizing antibody was measured once at study end.
Immunogenicity
- All clinical trial subjects (N = 135) were monitored for neutralizing antibodies (inhibitors) to Factor VIII by the modified Bethesda assay using blood samples obtained prior to the first infusion of Antihemophilic factor (recombinant), at defined intervals (at ED 10 to 15, at 3 months, and every further 3 months) during the studies and at the completion visit.
- No subject developed neutralizing antibodies to Factor VIII.
- Four subjects (3%) developed a non-neutralizing antibody without any inhibitory activity.
- The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay.
- Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease.
- For these reasons, comparison of the incidence of antibodies to Antihemophilic factor (recombinant) with the incidence of antibodies to other products may be misleading.
Postmarketing Experience
There is limited information regarding Antihemophilic factor (recombinant) Postmarketing Experience in the drug label.
Drug Interactions
There is limited information regarding Antihemophilic factor (recombinant) Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
Risk Summary
- There are no data with Antihemophilic factor (recombinant) use in pregnant women to inform a drug-associated risk.
- Animal reproduction studies have not been conducted with Antihemophilic factor (recombinant).
- It is not known whether Antihemophilic factor (recombinant) can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity.
- Antihemophilic factor (recombinant) should be given to a pregnant woman only if clearly needed.
- In the U.S. general population, the estimated background risk of major birth defect and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Antihemophilic factor (recombinant) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Antihemophilic factor (recombinant) during labor and delivery.
Nursing Mothers
- There is no information regarding the presence of Antihemophilic factor (recombinant) in human milk, the effect on the breastfed infant, or the effects on milk production.
- The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Antihemophilic factor (recombinant) and any potential adverse effects on the breastfed infant from Antihemophilic factor (recombinant) or from the underlying maternal condition.
Pediatric Use
- Safety and efficacy studies were performed in 59 previously treated pediatric patients (58 patients 2 to 11 years old) who received at least one dose of Antihemophilic factor (recombinant) for routine prophylaxis.
- Efficacy in routine prophylaxis and on-demand treatment of bleeding episodes is comparable between children and adults.
- The children received a total of 5746 infusions.
- Of these infusions, 5316 (93%) were for prophylaxis, 216 (4%) for the treatment of bleeding episodes, 41 (0.7%) for peri-operative management and 173 (3%) for pharmacokinetic (PK) and recovery assessments.
- For two adverse events (mild back pain, mild headache) in two (3%) subjects, causality was rated as possibly related to Antihemophilic factor (recombinant) administration.
- The pediatric pharmacokinetic data of Antihemophilic factor (recombinant) were obtained in 29 children between 2 and 5 years of age and 30 children between 6 and ≤12 years of age.
- Half-life (T 1/2 ) and incremental in vivo recovery (IVR) are lower in children than in adults and systemic drug clearance is substantially higher in the pediatric age group 2 to 5 yrs compared to adults.
- Higher doses and/or a more frequent dosing schedule for prophylactic treatment should be considered in pediatric patients aged 2 to 5 yrs.
Geriatic Use
Clinical studies of Antihemophilic factor (recombinant) did not include sufficient numbers of subjects age 65 and over to provide conclusive evidence as to whether or not they respond differently than younger subjects.
Gender
There is no FDA guidance on the use of Antihemophilic factor (recombinant) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Antihemophilic factor (recombinant) with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Antihemophilic factor (recombinant) in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Antihemophilic factor (recombinant) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Antihemophilic factor (recombinant) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Antihemophilic factor (recombinant) in patients who are immunocompromised.
Administration and Monitoring
Administration
Preparation and Reconstitution
- Antihemophilic factor (recombinant) package contents:
- single-use vial of Antihemophilic factor (recombinant) concentrate
- pre-filled syringe containing 2.5 mL Sterile Water for Injection
- vial adapter
- butterfly needle
- two alcohol swabs.
- Always work on a clean surface and wash your hands before performing the procedure.
- Allow the vial of Antihemophilic factor (recombinant) and the pre-filled syringe to come to room temperature.
- Remove the plastic flip-top cap from the Antihemophilic factor (recombinant) vial to expose the rubber stopper. (Figure A).
- Wipe the top of the vial with an alcohol swab and allow the rubber stopper of the vial to dry.
- Peel back the paper cover from the vial adapter package revealing the adapter spike without removing the adapter from the package (Figure B).
- With the concentrate vial on an even surface, insert the adapter spike into the rubber stopper. The adapter snaps to the vial when done (Figure C).
- Peel back the paper cover from the pre-filled syringe package. Connect plunger rod attaching the threaded end of the plunger rod to the solvent syringe, turning clockwise until a slight resistance is felt (Figure D). Avoid contact with shaft.
- Break off the tamper-proof plastic tip from the syringe by snapping the perforation of the cap. Do not touch the inside of the cap or the syringe tip (Figure E).
- Remove the adapter packaging and connect the syringe to the vial adapter by turning clockwise until resistance is felt (Figure F).
- Slowly inject all liquid from syringe into the concentrate vial (Figure G).
- Without removing the syringe, dissolve the concentrate powder in the vial by gently moving or swirling a few times. DO NOT SHAKE. Wait until all the powder dissolves completely.
- Inspect the final solution for particles. The solution should be clear, colorless, and free from visible particles. Do not use if solution is cloudy or has particulate matter.
- Turn the vial and syringe upside down (still attached).
- Slowly withdraw the solution into the syringe. Make sure that all liquid is transferred to the syringe (Figure H).
- Detach the filled syringe from the vial adapter by turning counter clockwise.

- Do not refrigerate the solution after reconstitution. Use the solution within 3 hours after reconstitution.
- If solution is not used within this time period, close the filled syringe with the tamper-proof plastic tip, and discard.
Monitoring
- For Intravenous use after reconstitution.
Dose
- Each vial of Antihemophilic factor (recombinant) is labeled with the actual Factor VIII potency expressed in international units (IU).
- One IU of Factor VIII activity is defined by the quantity of Factor VIII in one mL of normal human pooled plasma.
- Calculation of the required dose of Factor VIII is based on the empirical finding that 1 IU Factor VIII per kg body weight raises the plasma Factor VIII activity by approximately 2% of normal activity or 2 IU/dL when assessed using the one stage clotting assay.
- Use the following formulae to determine the required dose:

- Dose and duration of therapy depend on the severity of the Factor VIII deficiency, the location and extent of the bleeding, and the patient’s clinical condition.
On-demand Treatment and Control of Bleeding Episodes
- A guide for dosing Antihemophilic factor (recombinant) for the on-demand treatment and control of bleeding episodes is provided in TABLE 1 .
- Selected dosing regimen should maintain plasma Factor VIII activity levels at or above the plasma levels (in % of normal or in IU/dL) outlined in the table.

Perioperative Management
- A guide for dosing Antihemophilic factor (recombinant) during surgery (perioperative management) is provided in TABLE 2 .
- Dosing should aim at maintaining a plasma Factor VIII activity level at or above the plasma levels (in % of normal or in IU/dL) outlined in the table.

Routine Prophylaxis
- A guide for dosing Antihemophilic factor (recombinant) for routine prophylaxis to reduce the frequency of bleeding is provided in TABLE 3 .
- Exact dosing should be defined by the patient’s clinical status and response.

IV Compatibility
There is limited information regarding the compatibility of Antihemophilic factor (recombinant) and IV administrations.
Overdosage
There is limited information regarding Antihemophilic factor (recombinant) overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
There is limited information regarding Antihemophilic factor (recombinant) Pharmacology in the drug label.
Mechanism of Action
Antihemophilic factor (recombinant) temporarily replaces the missing clotting Factor VIII that is needed for effective hemostasis.
Structure
- Antihemophilic factor (recombinant), Antihemophilic Factor (Recombinant), is a sterile, non-pyrogenic, lyophilized powder for reconstitution for intravenous injection.
- The product is supplied in single-use vials containing nominal Factor VIII potencies of 250, 500, 1000 or 2000 IU.
- When reconstituted with 2.5 mL of solvent (Sterile Water for Injection), the respective nominal concentrations are 100, 200, 400 or 800 IU/mL.
- The reconstituted product contains the following excipients per mL: 18 mg sodium chloride, 5.4 mg sucrose, 5.4 mg L-arginine hydrochloride, 0.3 mg calcium chloride dihydrate, 1.2 mg poloxamer 188, and 1.2 mg sodium citrate dehydrate.
* The concentration of each of the excipients is the same for all potencies.
- Antihemophilic factor (recombinant) contains no preservatives.
- Each vial of Antihemophilic factor (recombinant) is labeled with the actual Factor VIII potency expressed in IU determined using one-stage clotting assay, using a reference material calibrated against a World Health Organization (WHO) International Standard for Factor VIII concentrates.
- One IU, as defined by the WHO standard for human Factor VIII concentrates, is approximately equal to the level of Factor VIII activity in 1 mL of fresh pooled, normal, human plasma.
- The mean specific activity of NUWIQ is 8124 IU/mg total protein.
- B-domain deleted recombinant coagulation Factor VIII (BDD-rFVIII) is the active ingredient in Antihemophilic factor (recombinant).
- BDD-rFVIII is a recombinant glycoprotein (a heterodimer) with an approximate molecular mass of 170 kDa, comprising the Factor VIII domains A1-A2 (so-called heavy chain of ~90 kDa) and A3-C1-C2 (so-called light chain of ~80 kDa), whereas the B-domain, present in the full-length plasma-derived Factor VIII, has been deleted.
- The purified protein consists of 1440 amino acids.
- The amino acid sequence is comparable to the B-domain deleted form of human plasma Factor VIII(90 + 80 kDa).
- BDD-rFVIII is produced by recombinant DNA technology in genetically modified human embryonic kidney (HEK) 293F cells with no animal or human derived materials added during the manufacturing process or to the final product.
- As NUWIQ is produced using a human cell-line, it contains post-translational modifications comparable to human plasma-derived Factor VIII and is devoid of Neu5Gc or α-1,3-Gal epitopes that may be present in products produced in animal cells.
- Furthermore, BDD-rFVIII is fully sulfated at Tyr1680.
- The active substance is concentrated and purified by a series of chromatography steps, which also includes two dedicated viral clearance steps: solvent/detergent (S/D) treatment for virus inactivation and 20 nm nanofiltration for removal of viruses.
Pharmacodynamics
- Hemophilia A is a bleeding disorder characterized by a deficiency of functional coagulation Factor VIII, resulting in a prolonged plasma clotting time as measured by the activated partial thromboplastin time (aPTT) assay.
- Treatment with Antihemophilic factor (recombinant) normalizes the aPTT over the effective dosing period.
Pharmacokinetics
- The pharmacokinetics (PK) of Antihemophilic factor (recombinant) were evaluated in an open-label, multicenter clinical study of 22 (20 adults and 2 adolescents) previously treated patients (PTPs) with severe Hemophilia A.
- The PK parameters ( TABLE 4 ) were based on plasma Factor VIII activity measured by the one-stage clotting assay after a single intravenous infusion of a 50 IU/kg dose.
- The PK profile obtained after 6 months of repeated dosing was comparable with the PK profile obtained after the first dose.

Pediatric Pharmacokinetics
- PK of pediatric patients is presented in TABLE 5 for the age groups 2 to 5 years and 6 to 12 years.
- They were based on plasma Factor VIII activity measured by the one-stage clotting assay after a single intravenous infusion of 50 IU/kg dose.
- Compared to adults and adolescents, IVR and T 1/2 were lower and systemic drug clearance (based on per kg bodyweight) was substantially higher in children 2 to 5 yr of age.
- IVR analysis after 3 and 6 months of prophylactic treatment yielded comparable results with the IVR after the first dose.
- As in the adult population, similar PK values were obtained using the chromogenic and the one-stage assay.
- The values in TABLE 5 reflect those obtained using the one-stage assay.

Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Long-term studies in animals to evaluate the carcinogenic potential of Antihemophilic factor (recombinant) or studies to determine the effects of Nuwiq on genotoxicity or fertility have not been performed.
Clinical Studies
- The efficacy of Antihemophilic factor (recombinant) was evaluated in three multi-center, open-label, prospective clinical trials in PTPs with severe Hemophilia A.
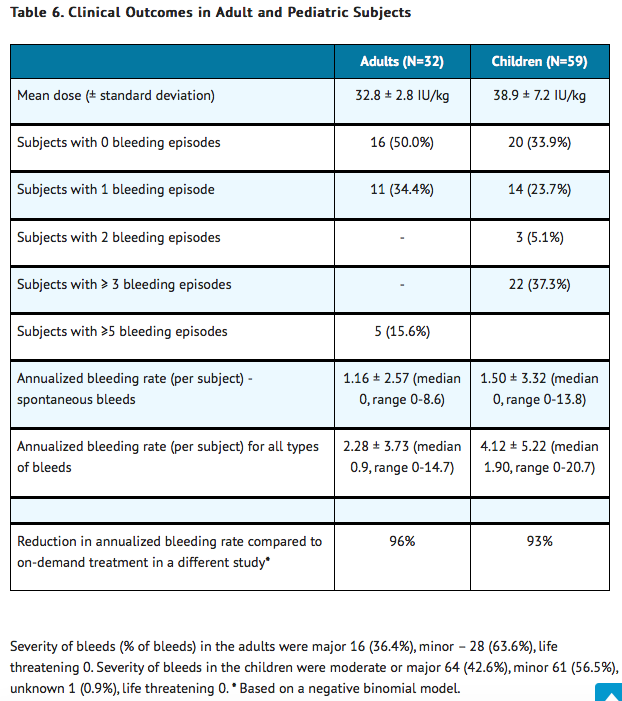
- For routine prophylaxis, the efficacy of Antihemophilic factor (recombinant) was evaluated in two multi-center studies, one in adult patients (n = 32) and one in pediatric patients (n = 59). * For the treatment of bleeding episodes, efficacy was evaluated in one multi-center study in adolescents (n = 2) and adults (n = 20) who were treated on-demand only, and also in patients who experienced breakthrough bleeding episodes in the two prophylaxis studies.
- Across all studies, subjects undergoing surgical procedures were evaluated for hemostatic efficacy during perioperative management.
On-demand Treatment and Control of Bleeding Episodes
- A total of 1124 bleeding episodes in 69 subjects (35 adults, 2 adolescents, and 32 children) were treated with Antihemophilic factor (recombinant).
- Response to each treatment was assessed by the patients using an ordinal scale of excellent (abrupt pain relief and/or unequivocal improvement in objective signs of bleeding within approximately 8 hours after a single infusion), good (definite pain relief and/or improvement in signs of bleeding within approximately 8–12 hours after an infusion requiring up to 2 infusions for complete resolution), moderate (probable or slight beneficial effect within approximately 12 hours after the first infusion requiring more than two infusions for complete resolution), or none (no improvement within 12 hours, or worsening of symptoms, requiring more than 2 infusions for complete resolution).
- The majority of treated bleeding episodes (n = 986) was from the study where patients only received on-demand treatment.
- 642 (65%) bleeding episodes occurred spontaneously, 341 (35%) were traumatic, and 3 (0.3%) bleeding episodes were due to other causes.
- The mean dose per injection used to treat a bleeding episode was 32 IU/kg.
- Hemostatic efficacy in response to Antihemophilic factor (recombinant) treatment was rated as excellent or good in 94% and as moderate in 6% of the bleeds.
- In case of breakthrough bleeding episodes, the mean dose per injection used to treat a bleeding episode was 33.3 IU/kg in adults (n=15 with 30 bleeding episodes) and 45 IU/kg in pediatric patients (n=32 with 108 bleeding episodes).
- The median number of injections to treat a bleeding episode was 1.
- Hemostatic efficacy was excellent or good in 100% of bleeds in adults and 82% of bleeds in pediatric patients.
Perioperative Management of Bleeding
- Across all studies, the efficacy of Antihemophilic factor (recombinant) as surgical prophylaxis was assessed in a total of 33 surgical procedures in 19 patients; 20 procedures in 7 patients were classed as minor and 13 procedures in 12 patients were classed as major.
- Antihemophilic factor (recombinant) pre-operative dosing ranged from 35 IU/kg to 50 IU/kg per infusion.
- The total number of infusions administered ranged from 1 to 5 for minor and 4 to 35 for major surgeries; one surgery required an injection of Antihemophilic factor (recombinant) during surgery.
- The efficacy of surgical prophylaxis was rated for each case by a surgeon and a hematologist, taking into account both the intra- and postoperative assessment.
- Hemostasis efficacy was rated at the end of the surgery by the surgeon and postoperatively by the surgeon and hematologist using ordinal scales as follows:
- Excellent: Intra-operative: intra-operative blood loss lower than or equal to the average expected blood loss for the type of procedure performed in a patient with normal hemostasis;. Postoperative: No postoperative bleeding or oozing that was not due to complications of surgery. All postoperative bleeding (due to complications of surgery) was controlled with Antihemophilic factor (recombinant) as anticipated for the type of procedure.
- Good: Intra-operative: intra-operative blood loss was higher than average expected blood loss but lower than or equal to the maximal expected blood loss for the type of procedure in a patient with normal hemostasis; Postoperative: No postoperative bleeding or oozing that was not due to complications of surgery. Control of postoperative bleeding due to complications of surgery required increased dosing with Antihemophilic factor (recombinant) or additional infusions, not originally anticipated for the type of procedure.
- Moderate: Intra-operative: Intra-operative blood loss was higher than maximal expected blood loss for the type of procedure performed in a patient with normal hemostasis, but hemostasis was controlled. Postoperative: Some postoperative bleeding and oozing that was not due to complications of surgery; control of postoperative bleeding required increased dosing with Antihemophilic factor (recombinant) or additional infusions, not originally anticipated for the type of procedure.
- None: Intra-operative: Hemostasis was uncontrolled necessitating a change in clotting factor replacement regimen. Postoperative: Extensive uncontrolled postoperative bleeding and oozing. Control of postoperative bleeding required use of an alternate FVIII concentrate.
- Efficacy for major surgeries was rated as excellent in 9 (69%) cases and as good in 3 (23%) cases.
- In 1 (8%) case, efficacy was rated as moderate.
- The efficacy of all minor surgeries was rated as excellent.
Routine Prophylaxis
- In the study evaluating the efficacy and safety of Antihemophilic factor (recombinant) for routine prophylaxis in 32 adult subjects (29 White, 3 Asian), the product was given every other day with a dose of 30-40 IU/kg for at least 6 months.
- In another study evaluating the safety, immunogenicity and hemostatic efficacy in 59 pediatric subjects aged 2 to 12 years (all White, 29 were 2 to 5 years old, and 30 between 6 and 12 years), subjects received Antihemophilic factor (recombinant) prophylactically every other day or 3 times per week for at least 6 months.
- Clinical outcomes are summarized in TABLE 6 .
How Supplied
- Antihemophilic factor (recombinant) is supplied in packages comprising a single-use vial containing nominally 250, 500, 1000, or 2000 international units (IU) of Factor VIII potency, a pre-filled syringe with 2.5 mL solvent (Water for Injection), a vial adapter, a butterfly needle and two alcohol swabs. The actual amount of Antihemophilic factor (recombinant) in IU is stated on each carton and vial.
- Components used in the packaging of Antihemophilic factor (recombinant) are not made with natural rubber latex.

Storage
Storage and Handling
- Store Antihemophilic factor (recombinant) in the original package to protect the Antihemophilic factor (recombinant) vials from light.
- Store Antihemophilic factor (recombinant) in powder form at 2 – 8°C (35 – 46°F) for up to 24 months. Do not freeze.
- During the shelf life, the product may be kept at room temperature [up to 25°C (77°F)] for a single period not exceeding 3 months.
- After storage at room temperature, do not return the product to the refrigerator.
- Do not use after the expiration date.
- Keep the reconstituted solution at room temperature. * Do not refrigerate after reconstitution.
- Use the reconstituted solution immediately or within 3 hours after reconstitution.
- Discard any remaining solution.
Images
Drug Images
{{#ask: Page Name::Antihemophilic factor (recombinant) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel









{{#ask: Label Page::Antihemophilic factor (recombinant) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Advise patients to read the FDA-approved patient labeling ( PATIENT INFORMATION and INSTRUCTIONS FOR USE )
- Because hypersensitivity reactions are possible with Antihemophilic factor (recombinant) , inform patients of the early signs of hypersensitivity reactions, including hives, generalized urticaria, tightness of the chest, wheezing, hypotension, and anaphylaxis. Advise patients to stop the injection if any of these symptoms arise and contact their physician, and seek prompt emergency treatment.
- Advise patients to contact their physician or treatment center for further treatment and/or assessment if they experience a lack of clinical response to Factor VIII replacement therapy, as this may be a manifestation of an inhibitor.
- Advise patients to consult with their healthcare provider prior to traveling. While traveling, patients should be advised to bring an adequate supply of Antihemophilic factor (recombinant) based on their current treatment regimen.
Precautions with Alcohol
Alcohol-Antihemophilic factor (recombinant) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
NUWIQ®, Antihemophilic Factor (Recombinant)
Look-Alike Drug Names
There is limited information regarding Antihemophilic factor (recombinant) Look-Alike Drug Names in the drug label.
Price
References
The contents of this FDA label are provided by the National Library of Medicine.