Squamous cell carcinoma of the skin differential diagnosis

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aditya Govindavarjhulla, M.B.B.S. [2], Raviteja Guddeti, M.B.B.S. [3]
Overview
Squamous cell carcinoma should be differentiated from melanoma and basal cell carcinoma. It accounts for 20% of all non-melanomatous tumors, and is fairly invasive contrary to its counterpart, basal cell carcinoma. Squamous cell carcinoma typically presents as a non-healing ulcer or growth on a sun exposed area of the skin.
Differentiating Squamous cell carcinoma from other Diseases
A few conditions that mimic Squamous cell carcinoma include the following:
| Diseases | Skin examination | Diagnosis | Additional findings | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Type | Color | Texture | Size | Distribution | Dermoscopic Findings | Histopathology | |||
| Cutaneous squamous cell carcinoma[1] | SCC in situ (Bowen's disease) |
|
|
|
|
|
|
|
|
| Invasive squamous cell carcinoma |
|
|
|
|
|
| |||
| Keratoacanthoma[2] |
|
|
|
|
|
|
|
| |
| Merkel cell carcinoma[3] |
|
|
|
|
|
|
| ||
| Basal cell carcinoma[4] | Nodular basal cell carcinoma |
|
|
|
|
|
| ||
| Superficial basal cell carcinoma |
|
|
|
|
| ||||
| Sclerosing basal cell carcinoma (morpheaform)[5] |
|
|
|
|
|
|
|
| |
| Prurigo nodules[6][7] |
|
|
|
|
|
|
|
| |
| Melanoma[8] | Melanoma in situ (Lentigo Maligna)[9] |
|
|
|
|
|
|
| |
| Lentigo maligna melanoma[10] |
|
|
|
|
|
|
| ||
| Superficial spreading melanoma[11] |
|
|
|
|
|
|
|
| |
| Nodular melanoma[12][13] |
|
|
|
|
|
|
|
| |
| Acral lentiginous melanoma[14] |
|
|
|
|
|
|
|
| |
| Amelanotic melanoma[15] |
|
|
|
|
|
|
|||
| Common nevus[16][17] |
|
|
|
|
|
|
| ||
| Blue nevus[18] |
|
|
|
|
|
|
| ||
| Spitz nevus[19][20] | Nonpigmented Spitz nevus |
|
|
|
|
|
| ||
| Reed-like Spitz[21] |
|
|
|
|
|
|
|
| |
| Solar lentigo[22] |
|
|
|
|
|
|
|
| |
| Sebaceous hyperplasia[23] |
|
|
|
|
| ||||
| Lichen planus-like keratosis[24] |
|
|
|
|
|
| |||
Squamous cell carcinoma of the mouth must be differentiated from other mouth lesions such as oral candidiasis and aphthous ulcer
| Disease | Presentation | Risk Factors | Diagnosis | Affected Organ Systems | Important features | Picture |
|---|---|---|---|---|---|---|
| Diseases predominantly affecting the oral cavity | ||||||
| Oral Candidiasis |
|
|
|
Localized candidiasis
Invasive candidasis |
|
 |
| Herpes simplex oral lesions |
|
|
|
|
 | |
| Aphthous ulcers |
|
|
|
|
|
 |
| Squamous cell carcinoma |
|
|
 | |||
| Leukoplakia |
|
|
|
|
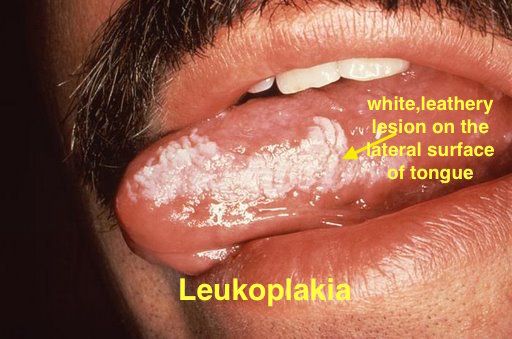 | |
| Melanoma |
|
|
|
|
 | |
| Fordyce spots |
|
|
|
|
 | |
| Burning mouth syndrome |
|
|
||||
| Torus palatinus |
|
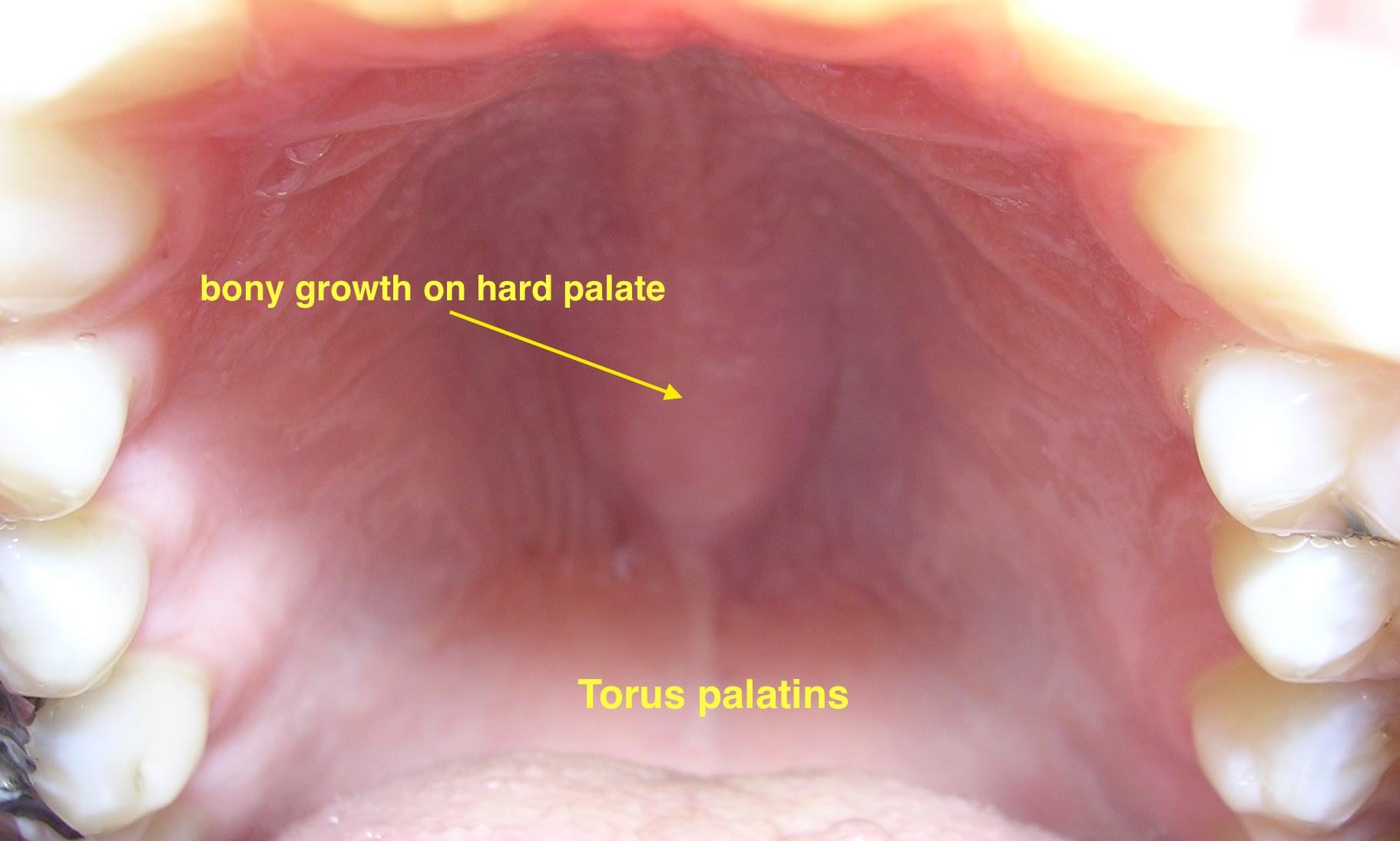 | ||||
| Diseases involving oral cavity and other organ systems | ||||||
| Behcet's disease |
|
|
|
 | ||
| Crohn's disease |
|
|
|
|||
| Agranulocytosis |
|
|
||||
| Syphilis[27] |
|
|
|
 | ||
| Coxsackie virus |
|
|
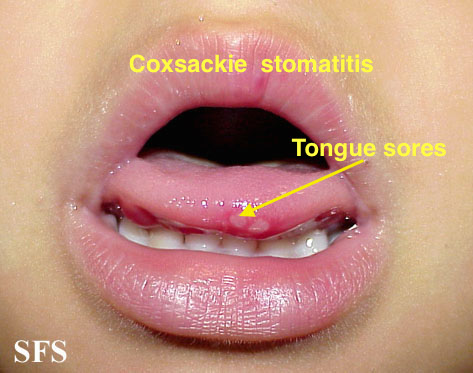 | |||
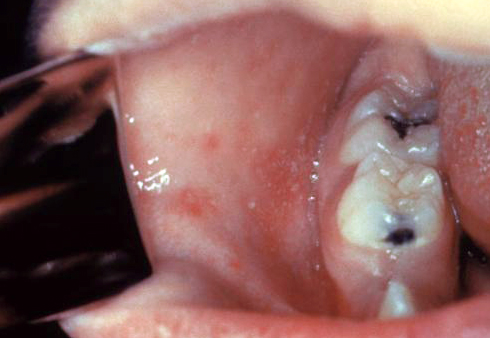
| Chicken pox |
|
|
|
|
 | |
| Measles |
|
|
|
 | ||
References
- ↑ Petter G, Haustein UF (2000). "Histologic subtyping and malignancy assessment of cutaneous squamous cell carcinoma". Dermatol Surg. 26 (6): 521–30. PMID 10848931.
- ↑ Kwiek B, Schwartz RA (2016). "Keratoacanthoma (KA): An update and review". J Am Acad Dermatol. 74 (6): 1220–33. doi:10.1016/j.jaad.2015.11.033. PMID 26853179.
- ↑ Albores-Saavedra J, Batich K, Chable-Montero F, Sagy N, Schwartz AM, Henson DE (2010). "Merkel cell carcinoma demographics, morphology, and survival based on 3870 cases: a population based study". J Cutan Pathol. 37 (1): 20–7. doi:10.1111/j.1600-0560.2009.01370.x. PMID 19638070.
- ↑ Wolberink EA, Pasch MC, Zeiler M, van Erp PE, Gerritsen MJ (2013). "High discordance between punch biopsy and excision in establishing basal cell carcinoma subtype: analysis of 500 cases". J Eur Acad Dermatol Venereol. 27 (8): 985–9. doi:10.1111/j.1468-3083.2012.04628.x. PMID 22759209.
- ↑ Wrone DA, Swetter SM, Egbert BM, Smoller BR, Khavari PA (1996). "Increased proportion of aggressive-growth basal cell carcinoma in the Veterans Affairs population of Palo Alto, California". J Am Acad Dermatol. 35 (6): 907–10. PMID 8959949.
- ↑ Errichetti E, Piccirillo A, Stinco G (2015). "Dermoscopy of prurigo nodularis". J Dermatol. 42 (6): 632–4. doi:10.1111/1346-8138.12844. PMID 25808786.
- ↑ Weigelt N, Metze D, Ständer S (2010). "Prurigo nodularis: systematic analysis of 58 histological criteria in 136 patients". J Cutan Pathol. 37 (5): 578–86. doi:10.1111/j.1600-0560.2009.01484.x. PMID 20002240.
- ↑ Witt C, Krengel S (2010). "Clinical and epidemiological aspects of subtypes of melanocytic nevi (Flat nevi, Miescher nevi, Unna nevi)". Dermatol Online J. 16 (1): 1. PMID 20137743.
- ↑ Connolly KL, Giordano C, Dusza S, Busam KJ, Nehal K (2019). "Follicular involvement is frequent in lentigo maligna: Implications for treatment". J Am Acad Dermatol. 80 (2): 532–537. doi:10.1016/j.jaad.2018.07.071. PMC 6333487. PMID 30266559.
- ↑ Connolly KL, Giordano C, Dusza S, Busam KJ, Nehal K (2019). "Follicular involvement is frequent in lentigo maligna: Implications for treatment". J Am Acad Dermatol. 80 (2): 532–537. doi:10.1016/j.jaad.2018.07.071. PMC 6333487. PMID 30266559.
- ↑ Argenziano G, Ferrara G, Francione S, Di Nola K, Martino A, Zalaudek I (2009). "Dermoscopy--the ultimate tool for melanoma diagnosis". Semin Cutan Med Surg. 28 (3): 142–8. doi:10.1016/j.sder.2009.06.001. PMID 19782937.
- ↑ Argenziano G, Soyer HP, Chimenti S, Talamini R, Corona R, Sera F; et al. (2003). "Dermoscopy of pigmented skin lesions: results of a consensus meeting via the Internet". J Am Acad Dermatol. 48 (5): 679–93. doi:10.1067/mjd.2003.281. PMID 12734496.
- ↑ Menzies, Scott W.; Moloney, Fergal J.; Byth, Karen; Avramidis, Michelle; Argenziano, Giuseppe; Zalaudek, Iris; Braun, Ralph P.; Malvehy, Josep; Puig, Susana; Rabinovitz, Harold S.; Oliviero, Margaret; Cabo, Horacio; Bono, Riccardo; Pizzichetta, Maria A.; Claeson, Magdalena; Gaffney, Daniel C.; Soyer, H. Peter; Stanganelli, Ignazio; Scolyer, Richard A.; Guitera, Pascale; Kelly, John; McCurdy, Olivia; Llambrich, Alex; Marghoob, Ashfaq A.; Zaballos, Pedro; Kirchesch, Herbert M.; Piccolo, Domenico; Bowling, Jonathan; Thomas, Luc; Terstappen, Karin; Tanaka, Masaru; Pellacani, Giovanni; Pagnanelli, Gianluca; Ghigliotti, Giovanni; Ortega, Blanca Carlos; Crafter, Greg; Ortiz, Ana María Perusquía; Tromme, Isabelle; Karaarslan, Isil Kilinc; Ozdemir, Fezal; Tam, Anthony; Landi, Christian; Norton, Peter; Kaçar, Nida; Rudnicka, Lidia; Slowinska, Monika; Simionescu, Olga; Di Stefani, Alessandro; Coates, Elliot; Kreusch, Juergen (2013). "Dermoscopic Evaluation of Nodular Melanoma". JAMA Dermatology. 149 (6): 699. doi:10.1001/jamadermatol.2013.2466. ISSN 2168-6068.
- ↑ Phan A, Dalle S, Touzet S, Ronger-Savlé S, Balme B, Thomas L (2010). "Dermoscopic features of acral lentiginous melanoma in a large series of 110 cases in a white population". Br J Dermatol. 162 (4): 765–71. doi:10.1111/j.1365-2133.2009.09594.x. PMID 19922528.
- ↑ Steglich RB, Meotti CD, Ferreira MS, Lovatto L, de Carvalho AV, de Castro CG (2012). "Dermoscopic clues in the diagnosis of amelanotic and hypomelanotic malignant melanoma". An Bras Dermatol. 87 (6): 920–3. PMC 3699915. PMID 23197217.
- ↑ Witt C, Krengel S (2010). "Clinical and epidemiological aspects of subtypes of melanocytic nevi (Flat nevi, Miescher nevi, Unna nevi)". Dermatol Online J. 16 (1): 1. PMID 20137743.
- ↑ Bauer J, Garbe C (2003). "Acquired melanocytic nevi as risk factor for melanoma development. A comprehensive review of epidemiological data". Pigment Cell Res. 16 (3): 297–306. PMID 12753404.
- ↑ Granter SR, McKee PH, Calonje E, Mihm MC, Busam K (2001). "Melanoma associated with blue nevus and melanoma mimicking cellular blue nevus: a clinicopathologic study of 10 cases on the spectrum of so-called 'malignant blue nevus'". Am J Surg Pathol. 25 (3): 316–23. PMID 11224601.
- ↑ Luo S, Sepehr A, Tsao H (2011). "Spitz nevi and other Spitzoid lesions part I. Background and diagnoses". J Am Acad Dermatol. 65 (6): 1073–84. doi:10.1016/j.jaad.2011.04.040. PMC 3217183. PMID 22082838.
- ↑ Argenziano G, Agozzino M, Bonifazi E, Broganelli P, Brunetti B, Ferrara G; et al. (2011). "Natural evolution of Spitz nevi". Dermatology. 222 (3): 256–60. doi:10.1159/000326109. PMID 21494025.
- ↑ Pedrosa AF, Lopes JM, Azevedo F, Mota A (2016). "Spitz/Reed nevi: a review of clinical-dermatoscopic and histological correlation". Dermatol Pract Concept. 6 (2): 37–41. doi:10.5826/dpc.0602a07. PMC 4866625. PMID 27222770.
- ↑ Tanaka M, Sawada M, Kobayashi K (2011). "Key points in dermoscopic differentiation between lentigo maligna and solar lentigo". J Dermatol. 38 (1): 53–8. doi:10.1111/j.1346-8138.2010.01132.x. PMID 21175756.
- ↑ Sato T, Tanaka M (2014). "Linear sebaceous hyperplasia on the chest". Dermatol Pract Concept. 4 (1): 93–5. doi:10.5826/dpc.0401a16. PMC 3919849. PMID 24520522.
- ↑ Morgan MB, Stevens GL, Switlyk S (2005). "Benign lichenoid keratosis: a clinical and pathologic reappraisal of 1040 cases". Am J Dermatopathol. 27 (5): 387–92. PMID 16148406.
- ↑ Ann M. Gillenwater, Nadarajah Vigneswaran, Hanadi Fatani, Pierre Saintigny & Adel K. El-Naggar (2013). "Proliferative verrucous leukoplakia (PVL): a review of an elusive pathologic entity!". Advances in anatomic pathology. 20 (6): 416–423. doi:10.1097/PAP.0b013e3182a92df1. PMID 24113312. Unknown parameter
|month=ignored (help) - ↑ Andrès E, Zimmer J, Affenberger S, Federici L, Alt M, Maloisel F. (2006). "Idiosyncratic drug-induced agranulocytosis: Update of an old disorder". Eur J Intern Med. 17 (8): 529–35. Text "pmid 17142169" ignored (help)
- ↑ title="By Internet Archive Book Images [No restrictions], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File:A_manual_of_syphilis_and_the_venereal_diseases%2C_(1900)_(14595882378).jpg"
- ↑ "Dermatology Atlas".
- ↑ Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE (2000). "Individual and community risks of measles and pertussis associated with personal exemptions to immunization". JAMA. 284 (24): 3145–50. PMID 11135778.
- ↑ Ratnam S, West R, Gadag V, Williams B, Oates E (1996). "Immunity against measles in school-aged children: implications for measles revaccination strategies". Can J Public Health. 87 (6): 407–10. PMID 9009400.