Pulmonary embolism
| Pulmonary embolism | |
 | |
|---|---|
| ICD-10 | I26 |
| ICD-9 | 415.1 |
| DiseasesDB | 10956 |
| MedlinePlus | 000132 |
| eMedicine | med/1958 emerg/490 radio/582 |
| Cardiology Network |
 Discuss Pulmonary embolism further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Synonyms and Associated Terms: PE
Pulmonary embolism (PE) is a common illness that can cause death and significant disability. PE occurs when there is an acute obstruction of the pulmonary artery (or one of its branches). Most often this is due to a venous thrombus (blood clot from a vein), which has been dislodged from its site of formation and embolizes to the arterial blood supply of one of the lungs. This process is termed thromboembolism.
Patients present with a wide array of symptoms and signs. These may include difficulty breathing, pain in the chest during breathing, and in more severe cases collapse, circulatory instability and sudden death. PE treatment requires rapid and accurate risk stratification before haemodynamic decompensation and the development of cardiogenic shock. Therapeutic application most often consists of an anticoagulant medication, such as heparin and warfarin, and rarely (in severe cases) with thrombolysis or surgery. In other, rarer forms of pulmonary embolism, material other than a blood clot is responsible; this may include fat or bone (usually in association with significant trauma), air (often when diving), clumped tumor cells, and amniotic fluid (affecting mothers during childbirth).
Epidemiology and Demographics
There are between 300,000 and 600,000 cases of pulmonary embolism (PE) in the U.S. each year. Without treatment almost 1/3 of patients will die, usually from recurrent PE. However, with prompt diagnosis and treatment, the mortality rate is only ~ 2 – 8%. Unfortunately, 2/3 of all cases of PE are not diagnosed before the autopsy.
Risk factors
The most common sources of embolism are proximal leg deep venous thrombosis (DVTs) or pelvic vein thromboses. Any risk factor for DVT also increases the risk that the venous clot will dislodge and migrate to the lung circulation, which happens in up to 15% of all DVTs. The conditions are generally regarded as a continuum termed venous thromboembolism (VTE).
The development of thrombosis is classically due to a group of causes named Virchow's triad (alterations in blood flow, factors in the vessel wall and factors affecting the properties of the blood). Often, more than one risk factor is present.
- Alterations in blood flow: immobilization (after surgery, injury or long-distance air travel), pregnancy (also procoagulant), obesity (also procoagulant)
- Factors in the vessel wall: of limited direct relevance in VTE
- Factors affecting the properties of the blood (procoagulant state):
- Estrogen-containing hormonal contraception
- Genetic thrombophilia (factor V Leiden, prothrombin mutation G20210A, protein C deficiency, protein S deficiency, antithrombin deficiency, hyperhomocysteinemia and plasminogen/fibrinolysis disorders).
- Acquired thrombophilia (antiphospholipid syndrome, nephrotic syndrome, paroxysmal nocturnal hemoglobinuria)
Risk Factors Identified in the PIOPED Study Independent risk factors identified in prospective investigation of pulmonary embolism diagnosis (PIOPED) include:
- Immobilization.
- Surgery within the last 3 months, and stroke were also risk factors, but may also relate to immobility.
- History of venous thromboembolism.
- Cancer: found in up to 17% of patients with an idiopathic deep vein thrombosis (DVT).
Risk Factors from the Nurses' Health Study
- Obesity: RR 2.9
- Smoking: 25 – 34 cigarettes / d (RR 1.9), > 35 cig / d (RR 3.3)
- Hypertension: RR 1.9
- Oral contraceptives: RR ~ 2 – 3
- Hormone replacement therapy: RR ~ 2
Risk Factors from the Physician's Health Study
- Factor V Leiden: RR 2.7, found in 40% of patients with idiopathic DVT.
- Use of oral contraceptives by a person with the Factor V mutation increases the risk of venous thromboembolism 35 fold.
- Hyperhomocysteinemia increases the risk of a DVT by a factor of 3.
- Hyperhomocysteinemia with Factor V increases the risk of a DVT by 10 fold.
- Lupus anticoagulant was found in 8.5% of patients with idiopathic DVT.
Pathophysiology and Etiology
Pulmonary embolism and deep vein thrombosis (DVT) should be considered part of the same spectrum of pathophysiology. Most pulmonary emboli result from thromboemboli in the deep veins of the lower extremities, but can also originate in the pelvic, renal, and upper extremity veins, as well as in the right heart. Almost 40% of patients with DVT and no symptoms of pulmonary embolus have evidence of PE on ventilation perfusion scanning (which itself is not 100% sensitive). Approximately 30% of patients with pulmonary embolus have evidence of deep vein thrombosis on ultrasound (U/S) of the lower extremities.
Natural History and Complications
Without treatment almost 1/3 of patients will die, usually from recurrent PE. However, with diagnosis and treatment, the mortality rate is only ~ 2 – 8%. Unfortunately, 2/3 of all cases of PE are not diagnosed before the autopsy.
Diagnosis
The diagnosis of PE is based primarily on the clinical evaluation combined with diagnostic modalities such as spiral CT, V/Q scan, use of the D-dimer and lower extremity ultrasound.
Pretest Probability
In spite of all of nonspecific clinical and lab findings, it has been shown that clinicians are actually fairly good at assigning meaningful clinical probabilities for PE.
- In PIOPED, 67% of the patients labeled as having a high clinical probability (>80% likelihood) had PE, as compared with only 9% of those give a low clinical probability (<20% likelihood).
- Unfortunately, the majority of patients (64%) were assigned an intermediate clinical probability (20 – 80% likelihood), reinforcing the fact that a clinical diagnosis can be difficult.
High Pretest Probability
Many authors, reserve the term high pretest probability for those patients with a clinical presentation consistent with PE, in whom an alternative diagnosis is not apparent (e.g. pneumonia) and who have known risk factors for venous thromboembolism (VTE).
Low Pretest Probability
Low pretest probability patients include those patients with an alternative diagnosis to explain the clinical findings or those without risk factors.
Intermediate Pretest Probability
Intermediate probability patients include those patients not fitting either high or low pretest probability definitions.
Predicting the Risk of Pulmonary Embolism
The decision to do medical imaging is usually based on clinical grounds, i.e. the medical history, symptoms and findings on physical examination.
- Development of the Wells score
The most commonly used method to predict clinical probability, the Wells score, is clinical prediction rule, whose use is complicated by multiple versions being available. In 1995, Wells et al initially developed a prediction rule (based on a literature search) to predict the likelihood of PE, based on clinical criteria.[1] The prediction rule was revised in 1998[2] This prediction rule was further revised when simplified during a validation by Wells et al in 2000.[3] In the 2000 publication, Wells proposed two different scoring systems using cutoffs or 2 or 4 with the same prediction rule.[3] In 2001, Wells published results using the more conservative cutoff of 2 to create three categories.[4] An additional version, the "modified extended version", using the more recent cutoff of 2 but including findings from Wells's initial studies[1][2] were proposed.[5] Most recently, a further study reverted to Wells's earlier use of a cutoff of 4 points[3] to create only two categories.[6]
There are additional prediction rules for PE, such as the Geneva rule. More importantly, the use of any rule is associated with reduction in recurrent thromboembolism.[7]
- Wells score
The Wells score:[8]
- clinically suspected DVT - 3.0 points
- alternative diagnosis is less likely than PE - 3.0 points
- tachycardia - 1.5 points
- immobilization/surgery in previous four weeks - 1.5 points
- history of DVT or PE - 1.5 points
- hemoptysis - 1.0 points
- malignancy (treatment for within 6 months, palliative) - 1.0 points
- Interpretation of the Wells score
Traditional interpretation[3][4]
- Score >6.0 - High (probability 59% based on pooled data[9])
- Score 2.0 to 6.0 - Moderate (probability 29% based on pooled data[9])
- Score <2.0 - Low (probability 15% based on pooled data[9])
Alternate interpretation[3][6]
- Score > 4 - PE likely. Consider diagnostic imaging.
- Score 4 or less - PE unlikely. Consider D-dimer to rule out PE.
Differential Diagnosis
Part of what makes the diagnosis of PE difficult is that the differential diagnosis of the clinical presentation of PE is extensive including a long list of conditions causing chest pain. Whats more, PE can accompany any of the above diagnoses.
- Anemia
- Angina pectoris
- Aortic stenosis
- Atrial fibrillation
- Cardiogenic shock
- Chronic Obstructive Pulmonary Disease
- Cor pulmonale
- Costochondritis
- Emphysema
- Herpes zoster
- Mitral stenosis
- Musculoskeletal pain
- Pleuritis
- Rib fracture
- Pericarditis
- Salicylate intoxication
- Hyperventilation
- Myocardial infarction
- Myocardial ischemia
- Myocarditis
- Bacterial pneumonia
- Community acquired pneumonia
- Pneumothorax
- Septic shock
- Distributive shock
- Hemorrhagic shock
- Sudden cardiac death
- Syncope
- Toxic shock syndrome
- Viral pneumonia
History of Risk Factors
In obtaining the history, the patient should be questioned regarding risk factors for pulmonary embolism. These include a recent history of surgery, immobilization, oral contraceptive use, smoking (particularly risky in the context of oral contraceptive use), cancer or prolonged travel.
Symptoms
- Sudden-onset dyspnea (shortness of breath)
- Chest pain of "pleuritic" nature (worsened by breathing),
- Cough
- Hemoptysis (coughing up blood)
Physical Examination
Vital Signs
collapse, and . About 15% of all cases of sudden death are attributable to PE.
Appearance of the Patient
- The patient may appear anxious
Extremities
More severe cases may be associated with cyanosis (blue discoloration, usually of the lips and fingers)
Thorough assessment should be made for the presence of a deep vein thrombosis
Laboratory Findings
Electrolyte and Biomarker Studies
- The arterial blood gases (ABG):
- Cvitanic and Marino, found that in patients without prior cardiopulmonary disease, 98% of patients with PE had either an increased AaDO2 or hypocapnia.
- They suggest, therefore, that in a patient without cardiopulmonary disease, the probability of PE is very unlikely (i.e. 2%) if they have a normal AaDO2 and a normal PaCO2.
- Other studies by Stein et.al. have not found the (ABG) have a high enough sensitivity, specificity, positive or negative predictive value to either diagnose PE or prevent further testing in patients thought to have PE.
- Cvitanic and Marino, found that in patients without prior cardiopulmonary disease, 98% of patients with PE had either an increased AaDO2 or hypocapnia.
- D-dimers are formed by the degradation of fibrin clot.
- Almost all patients with PE have some endogenous fibrinolysis, and therefore have elevated levels of D-dimer.
- Many other processes, such as pneumonia, congestive heart failure (CHF), myocardial infarction (MI), malignancy, and surgery, are also associated with a mild degree of fibrinolysis, and hence an elevated D-dimer is not specific for pulmonary embolism.
- Its negative predictive value, however, is 91 – 94% (when done by ELISA).
- In 1-3 weeks the BIDMC, and probably the BWH, will likely move to a quantitative latex agglutination that supposedly has the same sensitivity as the ELISA with a more rapid turn-around time.
- Potential problems with this approach include a false-positive U/S rate ~ 3%, and the fact that only ~ 30% of patients with PE documented by V/Q or Pulmonary angiography (PA-gram) had a positive LE U/S.
- Serial U/S or IPGs may get around this problem, but the data is there yet.
Blood tests
In low/moderate suspicion of PE, a normal D-dimer level (shown in a blood test) is enough to exclude the possibility of thrombotic PE.[10]
When a PE is being suspected, a number of blood tests are done, in order to exclude important secondary causes of PE. This includes a full blood count, clotting status (PT, APTT, TT), and some screening tests (erythrocyte sedimentation rate, renal function, liver enzymes, electrolytes). If one of these is abnormal, further investigations might be warranted.
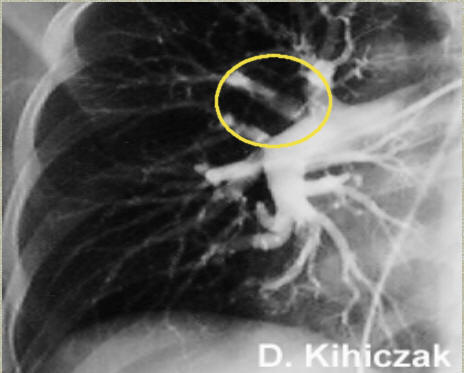
Medical imaging
The gold standard for diagnosing pulmonary embolism (PE) is pulmonary angiography. The PA gram has a sensitivity and specificity of > 95% in diagnosing PE. The estimated false-negative rate is 0.5 – 1.7%. Pulmonary angiography is used less often because of wider acceptance of CT scans, which are non-invasive.
-
Pulmonary angiogram in a patient with pulmonary embolus. A thrombus is observed in the area within the yellow circle. Source: www.e-radiography.net
-
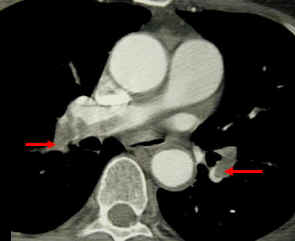
CT pulmonary angiogram. Clots in both the left and the right pulmonary arteries (red arrows). Source: www.lakeridgehealth.on.ca
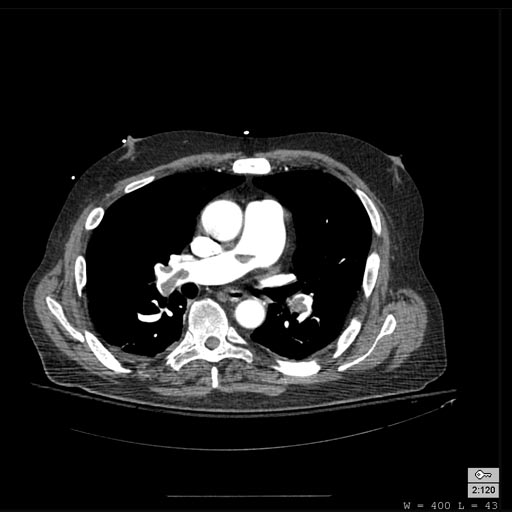
Computed Tomography
Computed tomography with radiocontrast, effectively a pulmonary angiogram imaged by CT and also known as CT pulmonary angiography (CTPA), is increasingly used as the mainstay in diagnosis. Advantages are clinical equivalence, its non-invasive nature, its greater availability to patients, and the possibility of picking up other lung disorders from the differential diagnosis in case there is no pulmonary embolism. Assessing the accuracy of CT pulmonary angiography is hindered by the rapid changes in the number of rows of detectors available in multidetector CT (MDCT) machines.[11] A study with a mixture of 4 slice and 16 slice scanners reported a sensitivity of 83% and a specificity of 96%. This study noted that additional testing is necessary when the clinical probability is inconsistent with the imaging results.[12] MDCT has progressed to be available with 64 slices, each 0.625 mm thick. These machines take 3-4 seconds to scan and may be gated to the heart beat. The sensitivity and specificity of these machines are currently not known.
CT findings in Acute PE
- Thrombus is located centrally within the vascular lumen or occludes the vessel (vessel cut-off sign)
- Commonly causes distention of the involved vessel.
CT findings in Chronic PE
- Eccentric and contiguous changes of the vessel wall
- Reduces the arterial diameter by more than 50%
- Evidence of recanalization within the thrombus
- An arterial web is present
Patient with Shortness of Breath
Patient with Acute RBBB
Ventilation/perfusion scan (or V/Q scan or lung scintigraphy), which shows that some areas of the lung are being ventilated but not perfused with blood (due to obstruction by a clot). This type of examination is used less often because of the more widespread availability of CT technology, however, it may be useful in patients who have an allergy to iodinated contrast or in pregnancy due to lower radiation exposure than CT. * The ventilation/perfusion ratio (V/Q) Scan: The PIOPED data suggests that normal perfusion scans are almost never associated with recurrent pulmonary embolism, even if anticoagulation is withheld.
- High-prob scans, however only identified 41% of patients with PE.
- In the setting of a high pre-test probability, a high-prob scan revealed PE in 95% of cases.
- Unfortunately, 41% of all scans in PIOPED were interpreted as intermediate, and an additional 16% were interpreted as low-prob.
- Upon angiography, however, 30 and 14% of these patients respectively were found to have PE.
- Based on these numbers, there has been a huge movement to abolish the low-prob, and intermediate-prob categories, and have readings either be high-prob, normal, or non-diagnostic.
- It should also be realized that the false-positive rate for high-prob scans was 14%, and that 72% of patients in PIOPED had a clinical – scan combination that required further investigation.
- It has been suggested by some authors that patients with an intermediate pre-test probability of PE a + venous ultrasound would provide the same justification for anticoagulation as would a confirmed PE.
- Spiral CT scanning is now a standard modality to non-invasively diagnose PE.
- Initial studies reported sensitivities for diagnosing emboli to the segmental level (4th order branch) as high as 98%, however subsequent studies have found sensitivities to be lower.
- Obviously, the sensitivity is higher with more proximal clot.
- Although smaller clot, in the subsegmental arteries, is certainly not as physiologically important as the larger, more proximal clot, they may be important predictors of future, larger clots.
- The study by Mayo et.al. concludes that the sensitivity and specificity of CT angio are higher than that of V/Q scans, as is the inter-observer agreement.
- They recommend getting a CT angio as the next test following an indeterminate V/Q scan, however caution that if the pre-test probability is ‘sufficiently high’ a standard angiogram should still be obtained after a negative CT angio.
- van Erkel et.al. performed a cost-effective analysis using spiral CT angio for the diagnosis of PE.
- The use of CT angio in a diagnostic algorithm was by far and away a more cost-effective strategy.
- If the sensitivity of CT angio was < 85%, conventional angiography was associated with a lower mortality, but still remained a more expensive strategy.
Magnetic Resonance Imaging
- Gadolinium-enhanced MRI is also a non-invasive diagnostic modality that has the advantage of no contrast exposure.
- Meaney et.al. examined 30 patients with suspected PE via angiography and Magnetic Resonance Angigraphy (MRA).
- 8 patients had + PA grams, and MRA identified all 5 lobar emboli, in addition to 16 of 17 segmental emboli.
- Another potential benefit of MR, is that is incredibly sensitive, perhaps even better than contrast venography, in imaging clot in the inferior vena cava (IVC) and pelvic veins, and these images can be obtained at the same time as the lung scan.
- Additionally, although MR is more expensive than V/Q scanning, when one takes into account the high number of indeterminate findings on V/Q, the effective cost per diagnosis may be cheaper with MR.
- Meaney et.al. examined 30 patients with suspected PE via angiography and Magnetic Resonance Angigraphy (MRA).
- It needs to be pointed out, that although the criticism of using CT and MR angio lacks sensitivity when examining the subsegmental arteries, inter-reader agreement was only 66% with pulmonary angiography in PIOPED.
Low Probablitity Diagnostic Tests and non-Diagnostic Tests
Tests that are frequently done that are not sensitive for PE, but can be diagnostic.
- Chest X-rays are often done on patients with shortness of breath to help rule-out other causes, such as congestive heart failure and rib fracture. Chest X-rays in PE are rarely normal,[13] but usually lack signs that suggest the diagnosis of PE (e.g. Westermark sign, Hampton hump).
- Only 12% of the CXRs in PIOPED were interpreted as normal
- The most common chest x-ray (CXR) finding is atelectasis, seen in 69%.
- Other, more ‘classic’ findings include
- Westermark sign (focal oligemia)
- Hampton hump (a peripheral wedge-shaped density above the diaphragm)
- Palla's sign (an enlarged right descending posteroanterior).
- Ultrasonography of the legs, also known as leg doppler, in search of deep venous thrombosis (DVT). The presence of DVT, as shown on ultrasonography of the legs, is in itself enough to warrant anticoagulation, without requiring the V/Q or spiral CT scans (because of the strong association between DVT and PE). This may be valid approach in pregnancy, in which the other modalities would increase the risk of birth defects in the unborn child. However, a negative scan does not rule out PE, and low-radiation dose scanning may be required if the mother is deemed at high risk of having pulmonary embolism.
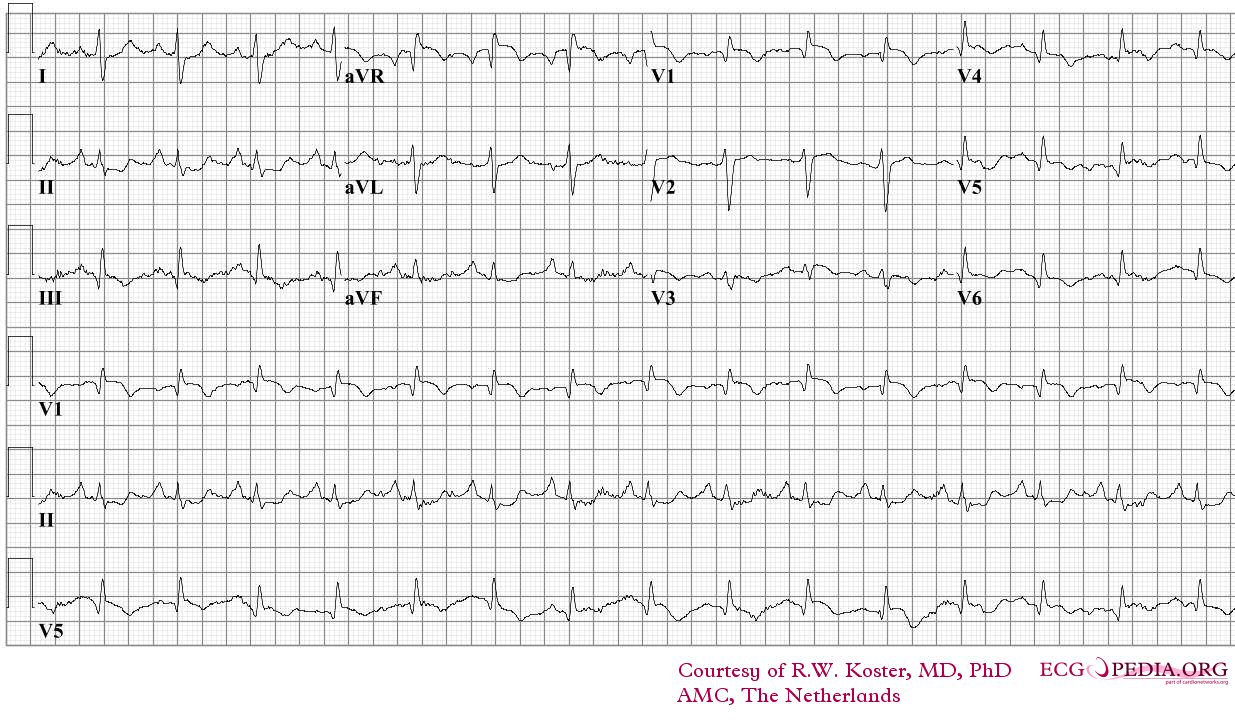
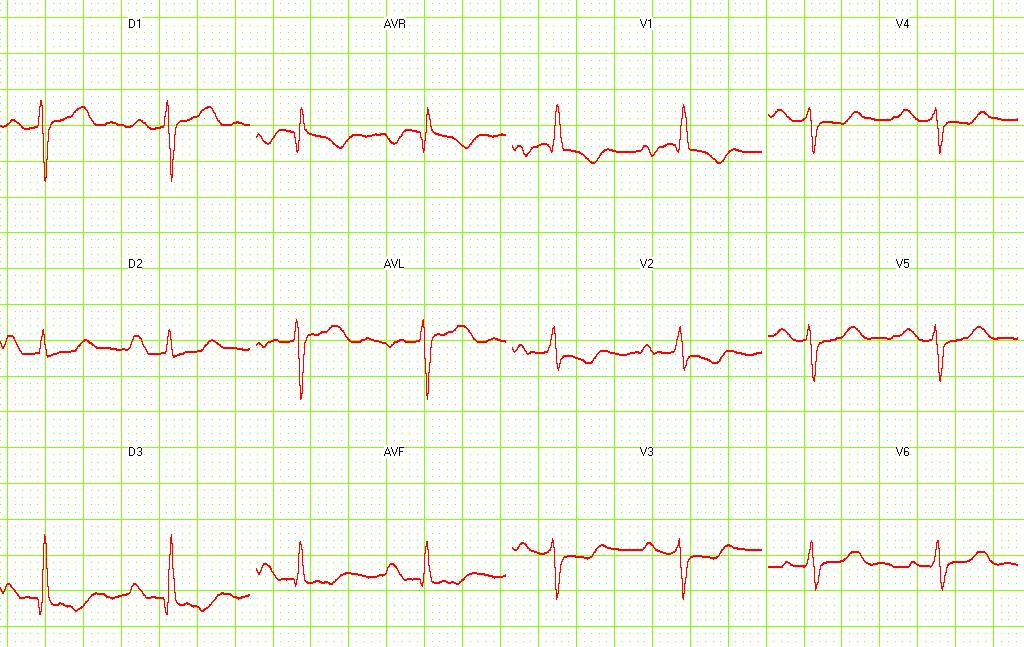
Electrocardiogram
- The most common ECG finding is anterior T-wave inversion.
- This likely represents reciprocal changes reflecting infero-posterior ischemia due to compression of the right coronary artery (RCA) as a result of pressure overload in the right ventricle (RV).
- Sinus tachycardia, right bundle branch block (RBBB), SIQIIITIII, and a normal ECG are also frequently seen, but again are not sensitive or specific
- There may be an S wave in lead 1, a Q wave in lead 3, and a flipped T wave in lead 3 (S1Q3T3 pattern).
An ECG may show signs of right heart strain or acute cor pulmonale in cases of large PEs - the classic signs are a large S wave in lead I, a large Q wave in lead III and an inverted T wave in lead III ("S1Q3T3").[14] This is occasionally (up to 20%) present, but may also occur in other acute lung conditions and has therefore limited diagnostic value; the most commonly seen sign in the ECG is sinus tachycardia.
-
ECG of a patient with pulmonary embolism Image courtesy of ecgpedia
-
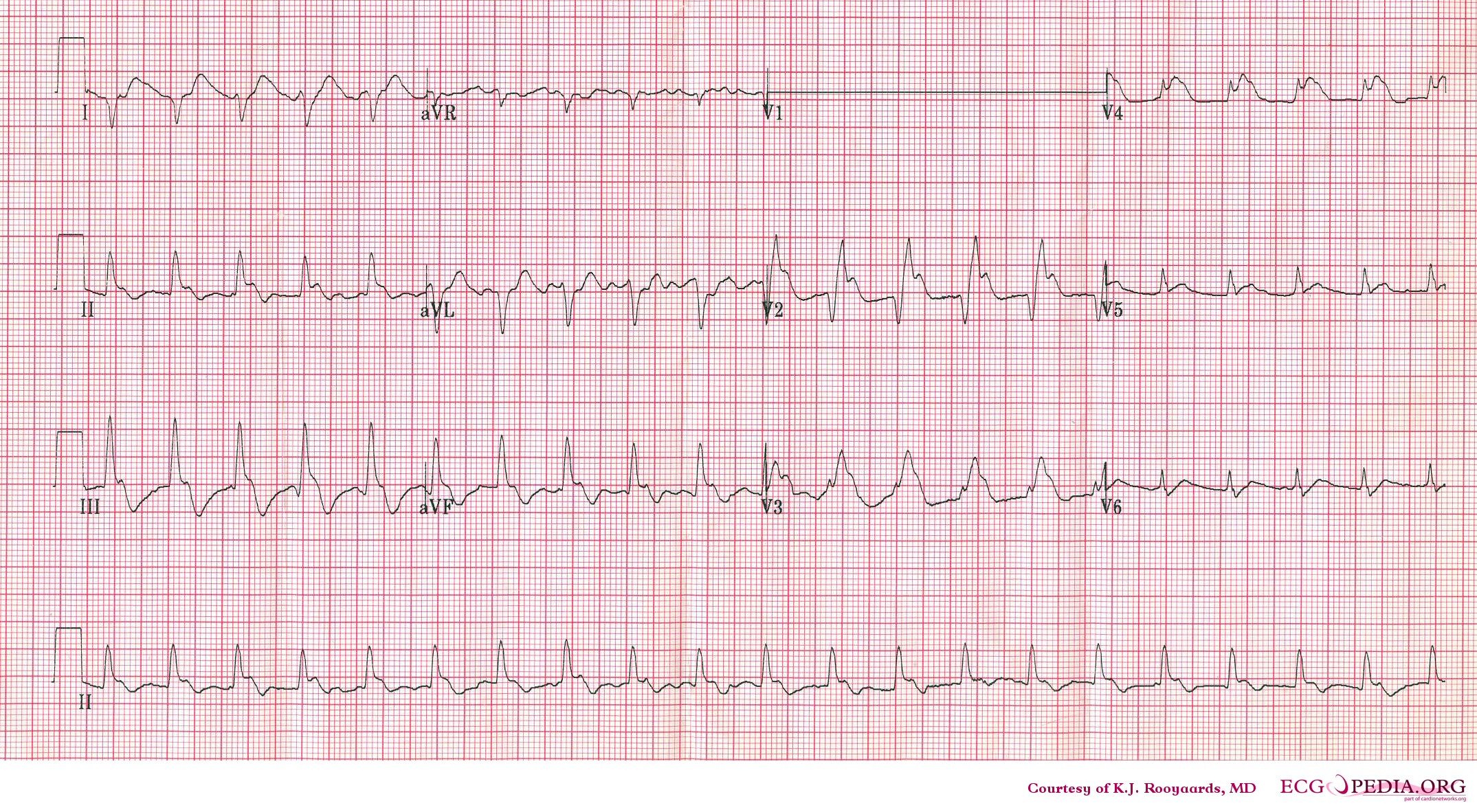
Another example; a patient with pulmonary embolism. Note the tachycardia and right axis.Image courtesy of ecgpedia
-
Pulmonary embolism. S1-Q3 and signs of right frontal axis are shown. Image courtesy of Dr Jose Ganseman Dr Ganseman's webpage: An ultimate source of EKG
Echocardiography findings
Approximately 40% of patients with PE have evidence of right heart strain on echocardiography.
In massive and submassive PE, dysfunction of the right side of the heart can be seen on echocardiography, an indication that the pulmonary artery is severely obstructed and the heart is unable to match the pressure. Some studies (see below) suggest that this finding may be an indication for thrombolysis. Not every patient with a (suspected) pulmonary embolism requires an echocardiogram, but elevations in cardiac troponins or brain natriuretic peptide may indicate heart strain and warrant an echocardiogram.[15]
The specific appearance of the right ventricle on echocardiography is referred to as the McConnell sign. This is the finding of akinesia of the mid-free wall but normal motion of the apex. This phenomenon has a 77% sensitivity and a 94% specificity for the diagnosis of acute pulmonary embolism.[16] Some authors suggest that the findings of right ventricular hypokinesis on echo, in association with a positive LENI is virtually pathognomonic for PE.
Combining tests into algorithms
Recent recommendations for a diagnostic algorithm have been published by the PIOPED investigators; however, these recommendations do not reflect research using 64 slice MDCT.[9] These investigators recommended:
- Low clinical probability. If negative D-dimer, PE is excluded. If positive D-dimer, obtain MDCT and based treatment on results.
- Moderate clinical probability. If negative D-dimer, PE is excluded. However, the authors were not concerned that a negative MDCT with negative D-dimer in this setting has an 5% probability of being false. Presumably, the 5% error rate will fall as 64 slice MDCT is more commonly used. If positive D-dimer, obtain MDCT and based treatment on results.
- High clinical probability. Proceed to MDCT. If positive, treat, if negative, addition tests are needed to exclude PE.
Treatment
In most cases, anticoagulant therapy is the mainstay of treatment. Acutely, supportive treatments, such as oxygen or analgesia, are often required.
Massive PE causing hemodynamic instability (marked decreased oxygen saturation, tachycardia and/or hypotension) is an indication for thrombolysis, the enzymatic destruction of the clot with medication. Some advocate its use also if right ventricular dysfunction can be demonstrated on echocardiography.[17]
Anticoagulation
In most cases, anticoagulant therapy is the mainstay of treatment. Heparin, low molecular weight heparins (such as enoxaparin and dalteparin), or fondaparinux is administered initially, while warfarin therapy is commenced (this may take several days, usually while the patient is in hospital). Warfarin therapy often requires frequent dose adjustment and monitoring of the INR. In PE, INRs between 2.0 and 3.0 are generally considered ideal. If another episode of PE occurs under warfarin treatment, the INR window may be increased to e.g. 2.5-3.5 (unless there are contraindications) or anticoagulation may be changed to a different anticoagulant e.g. low molecular weight heparin. In patients with an underlying malignancy, therapy with a course of low molecular weight heparin may be favored over warfarin based on the results of the CLOT trial.[18] Similarly, pregnant women are often maintained on low molecular weight heparin to avoid the known teratogenic effects of warfarin.
Warfarin therapy is usually continued for 3-6 months, or "lifelong" if there have been previous DVTs or PEs, or none of the usual risk factors is present. An abnormal D-dimer level at the end of treatment might signal the need for continued treatment among patients with a first unprovoked pulmonary embolus.[19]
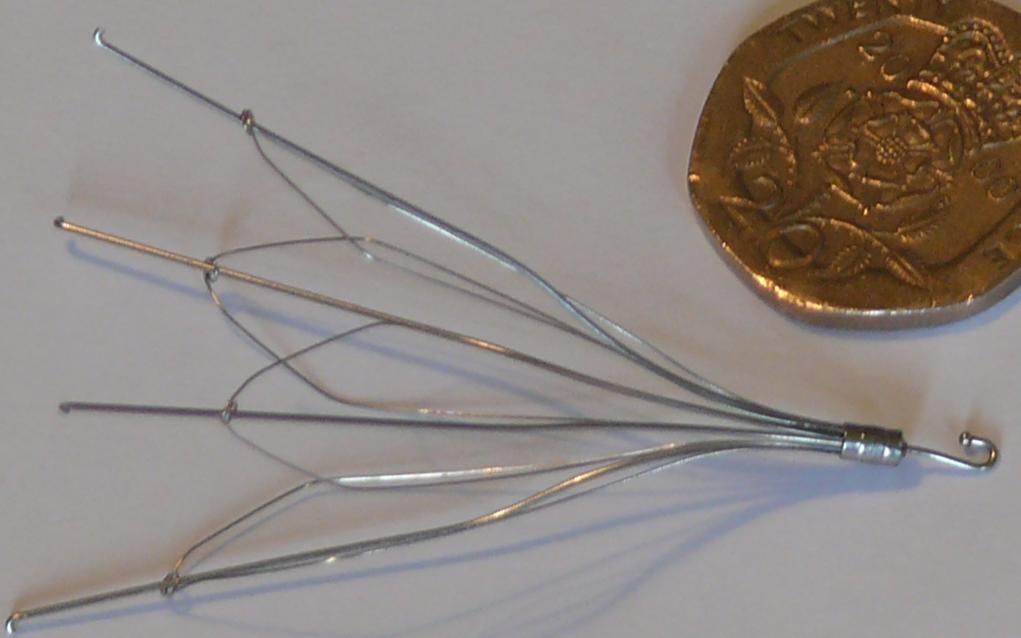
Inferior vena cava filter
If anticoagulant therapy is contraindicated and/or ineffective an inferior vena cava filter may be implanted.[20]
Thrombolysis
Thrombolysis can be given for severe PEs when surgery is not immediately available or possible (e.g. periarrest or during cardiac arrest). The only trial that addressed this issue had 8 patients; the four receiving thrombolysis survived, while the four who received only heparin died.[21] The use of thrombolysis in moderate PEs is still debatable. The aim of the therapy is to dissolve the clot, but there is an attendant risk of bleeding or stroke.[22]
Surgical management of PE
Surgical management of acute pulmonary embolism (pulmonary thrombectomy) is uncommon and has largely been abandoned because of poor long-term outcomes. However, recently, it has gone through a resurgence with the revision of the surgical technique and is thought to benefit selected patients.[23]
Chronic pulmonary embolism leading to pulmonary hypertension (known as chronic thromboembolic hypertension) is treated with a surgical procedure known as a pulmonary thromboendarterectomy.
Prognosis
Mortality from untreated PE is said to be 26%. This figure comes from a trial published in 1960 by Barrit and Jordan[24] which compared anticoagulation against placebo for the management of PE. Barritt and Jordan performed their study in the Bristol Royal Infirmary in 1957. This study is the only placebo controlled trial ever to examine the place of anticoagulants in the treatment of PE, the results of which were so convincing that the trial has never been repeated as to do so would be considered unethical. That said, the reported mortality rate of 26% in the placebo group is probably an overstatement, given that the technology of the day may have detected only severe PEs.
Prognosis depends on the amount of lung that is affected and on the co-existence of other medical conditions; chronic embolisation to the lung can lead to pulmonary hypertension. There is controversy over whether or not small subsegmental PEs need to be treated at all[25] and some evidence exists that patients with subsegmental PEs may do well without treatment.[26][12]
Predicting mortality
The PESI and Geneva prediction rules can estimate mortality and so may guide selection of patients who can be considered for outpatient therapy.[27]
Right ventricular dysfunction on echocardiography and higher than normal concentrations of troponin identify high risk patients who might need escalation of therapy with thrombolysis or embolectomy even if the blood pressure is normal on presentation.
Evaluation for underlying causes for recurrence
After a first PE, the search for secondary causes is usually brief. Only when a second PE occurs, and especially when this happens while still under anticoagulant therapy, a further search for underlying conditions is undertaken. This will include testing ("thrombophilia screen") for Factor V Leiden mutation, antiphospholipid antibodies, protein C and S and antithrombin levels, and later prothrombin mutation, MTHFR mutation, Factor VIII concentration and rarer inherited coagulation abnormalities.
For prevention of recurrences, when patients are admitted to medical wards or when patients undergo surgery, their physicians should prescribe prophylactic measures to prevent PE. After hospital discharge, prophylaxis should continue for about a month for patients at high risk of thromboembolism.
References
- ↑ 1.0 1.1 Wells PS, Hirsh J, Anderson DR, Lensing AW, Foster G, Kearon C, Weitz J, D'Ovidio R, Cogo A, Prandoni P (1995). "Accuracy of clinical assessment of deep-vein thrombosis". Lancet. 345 (8961): 1326–30. doi:doi:10.1016/S0140-6736(95)92535-X Check
|doi=value (help). PMID 7752753. - ↑ 2.0 2.1 Wells PS, Ginsberg JS, Anderson DR, Kearon C, Gent M, Turpie AG, Bormanis J, Weitz J, Chamberlain M, Bowie D, Barnes D, Hirsh J (1998). "Use of a clinical model for safe management of patients with suspected pulmonary embolism". Ann Intern Med. 129 (12): 997–1005. PMID 9867786.
- ↑ 3.0 3.1 3.2 3.3 3.4 Wells P, Anderson D, Rodger M, Ginsberg J, Kearon C, Gent M, Turpie A, Bormanis J, Weitz J, Chamberlain M, Bowie D, Barnes D, Hirsh J (2000). "Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer". Thromb Haemost. 83 (3): 416–20. PMID 10744147.
- ↑ 4.0 4.1 Wells PS, Anderson DR, Rodger M, Stiell I, Dreyer JF, Barnes D, Forgie M, Kovacs G, Ward J, Kovacs MJ (2001). "Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer". Ann Intern Med. 135 (2): 98–107. PMID 11453709.
- ↑ Sanson BJ, Lijmer JG, Mac Gillavry MR, Turkstra F, Prins MH, Büller HR (2000). "Comparison of a clinical probability estimate and two clinical models in patients with suspected pulmonary embolism. ANTELOPE-Study Group". Thromb. Haemost. 83 (2): 199–203. PMID 10739372.
- ↑ 6.0 6.1 van Belle A, Büller H, Huisman M, Huisman P, Kaasjager K, Kamphuisen P, Kramer M, Kruip M, Kwakkel-van Erp J, Leebeek F, Nijkeuter M, Prins M, Sohne M, Tick L (2006). "Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, D-dimer testing, and computed tomography". JAMA. 295 (2): 172–9. doi:10.1001/jama.295.2.172. PMID 16403929.
- ↑ Roy PM, Meyer G, Vielle B, Le Gall C, Verschuren F, Carpentier F, Leveau P, Furber A (2006). "Appropriateness of diagnostic management and outcomes of suspected pulmonary embolism". Ann. Intern. Med. 144 (3): 157–64. PMID 16461959.
- ↑ Neff MJ (2003). "ACEP releases clinical policy on evaluation and management of pulmonary embolism". American family physician. 68 (4): 759–60. PMID 12952389.
- ↑ 9.0 9.1 9.2 9.3 Stein PD, Woodard PK, Weg JG, Wakefield TW, Tapson VF, Sostman HD, Sos TA, Quinn DA, Leeper KV, Hull RD, Hales CA, Gottschalk A, Goodman LR, Fowler SE, Buckley JD (2007). "Diagnostic pathways in acute pulmonary embolism: recommendations of the PIOPED II Investigators". Radiology. 242 (1): 15–21. doi:10.1148/radiol.2421060971. PMID 17185658.
- ↑ Bounameaux H, de Moerloose P, Perrier A, Reber G (1994). "Plasma measurement of D-dimer as diagnostic aid in suspected venous thromboembolism: an overview". Thromb. Haemost. 71 (1): 1–6. PMID 8165626.
- ↑ Schaefer-Prokop C, Prokop M (2005). "MDCT for the diagnosis of acute pulmonary embolism". European radiology. 15 Suppl 4: D37–41. PMID 16479644.
- ↑ 12.0 12.1 Stein PD, Fowler SE, Goodman LR; et al. (2006). "Multidetector computed tomography for acute pulmonary embolism". N. Engl. J. Med. 354 (22): 2317–27. doi:10.1056/NEJMoa052367. PMID 16738268.
- ↑ Worsley D, Alavi A, Aronchick J, Chen J, Greenspan R, Ravin C (1993). "Chest radiographic findings in patients with acute pulmonary embolism: observations from the PIOPED Study". Radiology. 189 (1): 133–6. PMID 8372182.
- ↑ McGinn S, White PD. Acute cor pulmonale resulting from pulmonary embolism. J Am Med Assoc 1935;104:1473–1480.
- ↑ Kucher N, Goldhaber SZ (2003). "Cardiac biomarkers for risk stratification of patients with acute pulmonary embolism". Circulation. 108 (18): 2191–4. doi:10.1161/01.CIR.0000100687.99687.CE. PMID 14597581.
- ↑ McConnell MV, Solomon SD, Rayan ME, Come PC, Goldhaber SZ, Lee RT (1996). "Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism". Am. J. Cardiol. 78 (4): 469–73. PMID 8752195.
- ↑ Goldhaber SZ. Pulmonary embolism. Lancet 2004;363:1295-305. PMID 15094276.
- ↑ Lee AY, Levine MN, Baker RI, Bowden C, Kakkar AK, Prins M, Rickles FR, Julian JA, Haley S, Kovacs MJ, Gent M (2003). "Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer". N Engl J Med. 349 (2): 146–53. PMID 12853587.
- ↑ Palareti G, Cosmi B, Legnani C; et al. (2006). "D-dimer testing to determine the duration of anticoagulation therapy". N. Engl. J. Med. 355 (17): 1780–9. doi:10.1056/NEJMoa054444. PMID 17065639.
- ↑ Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P, Laporte S, Faivre R, Charbonnier B, Barral F, Huet Y, Simonneau G (1998). "A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group". N Engl J Med. 338 (7): 409–15. PMID 9459643.
- ↑ Jerjes-Sanchez C, Ramirez-Rivera A, de Lourdes Garcia M, Arriaga-Nava R, Valencia S, Rosado-Buzzo A, Pierzo JA, Rosas E. Streptokinase and Heparin versus Heparin Alone in Massive Pulmonary Embolism: A Randomized Controlled Trial. J Thromb Thrombolysis 1995;2:227-229. PMID 10608028.
- ↑ Dong B, Jirong Y, Liu G, Wang Q, Wu T. Thrombolytic therapy for pulmonary embolism. Cochrane Database Syst Rev 2006;(2):CD004437. PMID 16625603.
- ↑ Augustinos P, Ouriel K (2004). "Invasive approaches to treatment of venous thromboembolism". Circulation. 110 (9 Suppl 1): I27–34. PMID 15339878.
- ↑ "Anticoagulant drugs in the treatment of pulmonary embolism: a controlled trial". Lancet. 1: 1309&ndash, 1312. 1960. PMID 13797091. Text " Barritt DW, Jorden SC " ignored (help)
- ↑ Le Gal G, Righini M, Parent F, van Strijen M, Couturaud F (2006). "Diagnosis and management of subsegmental pulmonary embolism". J Thromb Haemost. 4 (4): 724–31. PMID 16634736.
- ↑ Perrier A, Bounameaux H (2006). "Accuracy or outcome in suspected pulmonary embolism". N Engl J Med. 354 (22): 2383–5. PMID 16738276.
- ↑ Jiménez D, Yusen RD, Otero R; et al. (2007). "Prognostic models for selecting patients with acute pulmonary embolism for initial outpatient therapy". Chest. 132 (1): 24–30. doi:10.1378/chest.06-2921. PMID 17625081.
Sources
- Bertucci, V., Asch, M.R., Balter, M., Prognosis in a patient with an initial normal pulmonary angiogram, Chest 1994; 105: 1257-1258.
- Cvitanic, O, Marino, P.L., Improved use of arterial blood gas analysis in suspected pulmonary embolism, Chest 1989; 95: 48-51.
- Drucker, E.A., et.al., Acute pulmonary embolism: assessment of helical CT for diagnosis, Radiology 1998; 209: 235-241.
- Ferrari, E., et.al., The ECG in pulmonary embolism: predictive value of negative T waves in precordial leads – 80 case reports, Chest 1997; 111: 537-543.
- Goldhaber, S.Z., et.al., Quantitative plasma D-dimer levels among patients undergoing pulmonary angiography for suspected pulmonary embolism, JAMA 1993; 270: 2819-2822.
- Goldhaber, S.Z., Pulmonary embolism, NEJM 1998; 339: 93-104.
- Mayo, J.R., et.al., Pulmonary embolism: prospective comparison of spiral CT with ventilation-perfusion scintigraphy, Radiology 1997; 205: 447-452.
- Meaney, J.F.M., et.al., Diagnosis of pulmonary embolism with magnetic resonance angiography, NEJM 1997; 336: 1422-1427.
- The PIOPED investigators, Value of the ventilation / perfusion scan in acute pulmonary embolism: results of the prospective investigation of pulmonary embolism diagnosis (PIOPED), JAMA 1990; 263: 2753-2759.
- Remy-Jardin, M., et.al., Diagnosis of pulmonary embolism with spiral CT: comparison with pulmonary angiography and scintigraphy, Radiology 1996; 200: 6999-706.
- Stein, P.D., et.al., Clinical, laboratory, roentgenographic, and electrocardiographic findings in patients with acute pulmonary embolism and no pre-existing cardiac or pulmonary disease, Chest 1991; 100: 598-603.
- Stein, P.D., et.al., Arterial blood gas analysis in the assessment of suspected pulmonary embolism, Chest 1996; 109: 78-81.
- Thompson, B.T., Hales, C.A., Diagnostic strategies for acute pulmonary embolism, in UpToDate, September 10, 1998.
- Van Erkel, A.R., et.al., Spiral CT angiography for suspected pulmonary embolism: a cost-effective analysis, Radiology 1996; 201: 29-36.
Acknowledgements
The content on this page was first contributed by: Editor-In-Chief: C. Michael Gibson, M.S., M.D. [4] and David Feller-Kopman, M.D.
List of contributors:
For Patients
<youtube v=gGrDAGN5pC0/>
External links
- Vascular Disease Foundation
- Venous Disease Coalition
- Goldminer, Pulmonary embolism
- Images of Pulmonary Embolism
- North American Thrombosis Forum
de:Lungenembolie eo:Pulma embolio eu:BTE ko:폐색전증 it:Embolia polmonare nl:Longembolie no:Lungeemboli simple:Pulmonary embolism sr:Плућна емболија