Pericarditis
| Pericarditis | ||
 | ||
|---|---|---|
| Mesothelial cyst of the pericardium. Note the rounded mass in the right costophrenic angle (arrow). Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | ||
| ICD-10 | I01.0, I09.2, I30-I32 | |
| ICD-9 | 420.90 | |
| DiseasesDB | 9820 | |
| MedlinePlus | 000182 | |
| eMedicine | med/1781 emerg/412 | |
| MeSH | C14.280.720 | |
|
WikiDoc Resources for Pericarditis |
|
Articles |
|---|
|
Most recent articles on Pericarditis Most cited articles on Pericarditis |
|
Media |
|
Powerpoint slides on Pericarditis |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Pericarditis at Clinical Trials.gov Clinical Trials on Pericarditis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Pericarditis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Pericarditis Discussion groups on Pericarditis Patient Handouts on Pericarditis Directions to Hospitals Treating Pericarditis Risk calculators and risk factors for Pericarditis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Pericarditis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information click here
| Cardiology Network |
 Discuss Pericarditis further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Diseases of the pericardium overview
Pathophysiology & Etiology
Overview | Pericarditis causes
Differential Diagnosis for Diseases of the Pericardium
Pericarditis differential diagnosis | Acute Pericarditis | Chronic Pericarditis
Clinical presentation
Chest pain, radiating to the back and relieved by sitting up forward and worsened by lying down, is the classical presentation. Other symptoms of pericarditis may include dry cough, fever, fatigue and anxiety. Pericarditis can be misdiagnosed as myocardial infarction, and vice versa.
The classic sign of pericarditis is a friction rub. Other signs include ST-elevation and PR-depression on EKG (all leads); cardiac tamponade (pulsus paradoxus with hypotension), and congestive heart failure (elevated jugular venous pressure with peripheral edema).
Natural History
Most cases of acute idiopathic pericarditis resolve without complications or recurrence. Complications may include:
Types & Forms of Pericarditis
- A. Congenital Diseases of the Pericardium
- B. Acquired Diseases of the Pericardium
Diagnosis
History and Symptoms | Physical Examination | Laboratory Findings
Treatment
Pharmacotherapies
Surgical and Device Based Therapies
Pericardiocentesis
A thoracoscopic approach to creating a pericardial window
A surgical subxiphoid incision to create a pericardial window
Pericardial Stripping for Constrictive Pericarditis
The definitive treatment for constrictive pericarditis is pericardial stripping, which is a surgical procedure where the entire pericardium is peeled away from the heart. This may be effective in up to 50% of patients. This procedure has significant risk involved, since the thickened pericardium is often adherent to the myocardium and coronary arteries.
In patients who have undergone coronary artery bypass surgery with pericardial sparing, there is danger of tearing a bypass graft while removing the pericardium. If any pericardium is not removed, it is possible for bands of pericardium to cause localized constriction which may cause symptoms and signs consistent with constriction.
Treatment Related Videos
- <youtube v=lJ6KzpnjbRg/>
Complications
Fibrinous pericarditis
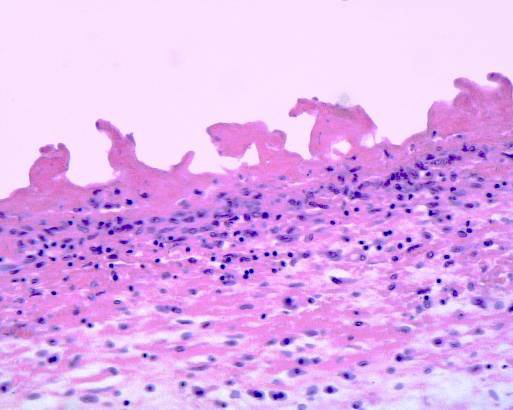
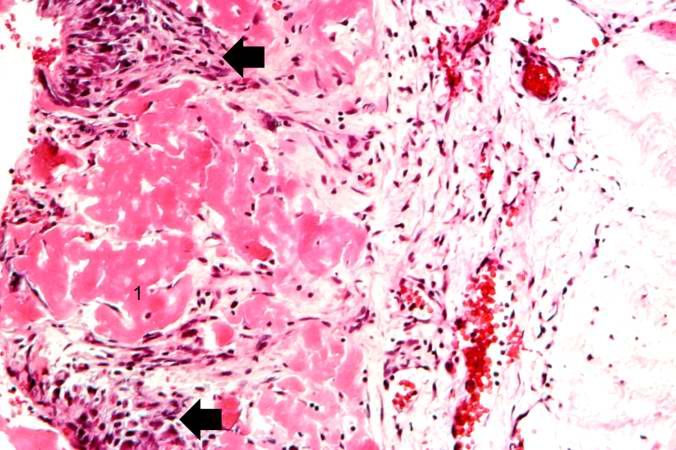
Fibrinous pericarditis is an exudative inflammation.
The pericardium is infiltrated by the fibrinous exudate. This consists of fibrin strands and leukocytes.
Fibrin describes an amorphous, eosinophilic (pink) network. Leukocytes (mainly neutrophils) are found within the fibrin deposits and intrapericardic.
Vascular congestion is also present. The myocardium has no changes. Sometimes referred to as having "Bread and Butter Appearance". Photo at: Atlas of Pathology
Pericarditis due to tuberculosis
Pericarditis caused by tuberculosis is difficult to diagnose, because definitive diagnosis requires culturing Mycobacterium tuberculosis from aspirated pericardial fluid or pericardial biopsy, which requires high technical skill and is often not diagnostic (the yield from culture is low even with optimum specimens).
The Tygerberg scoring system helps the clinician to decide whether pericarditis is due to tuberculosis or whether it is due to another cause:
- Night sweats (1 point),
- Weight loss (1 point),
- Fever (2 point),
- Serum globulin > 40g/l (3 points),
- Blood total leucocyte count <10 x 109/l (3 points);
A total score of 6 or more is highly suggestive of tuberculous pericarditis.[1]
Pericardial fluid with an interferon-γ level greater than 50pg/ml is highly specific for tuberculous pericarditis.
The definitive treatment for constrictive pericarditis is pericardial stripping, which is a surgical procedure where the entire pericardium is peeled away from the heart. This procedure has significant risk involved,[2] with mortality rates of 6% or higher in major referral centers.[3][4] The high risk of the procedure is attributed to adherence of the thickened pericardium to the myocardium and coronary arteries. In patients who have undergone coronary artery bypass surgery with pericardial sparing, there is danger of tearing a bypass graft while removing the pericardium.
Case Examples
Case #1
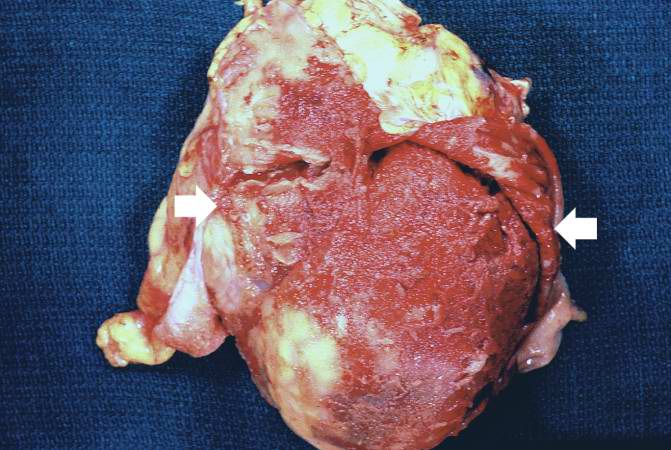
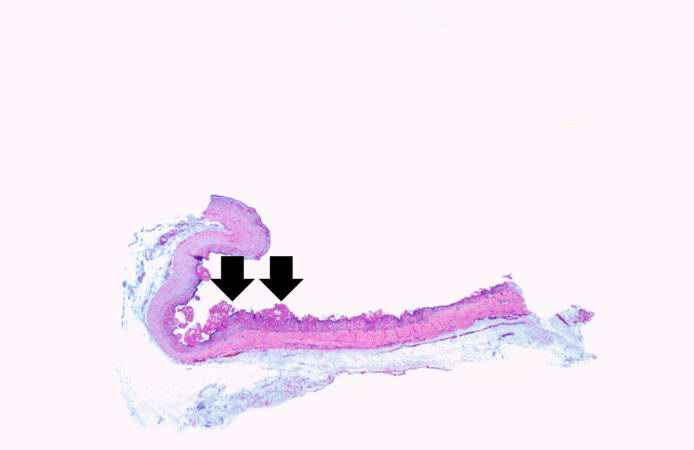
Clinical Summary
This patient is a 36-year-old white male with a history of long-standing renal disease who presents with end-stage kidney disease and a BUN of 112 mg/dL. During the present hospitalization he developed a pericardial friction rub and pericardial and pleural effusions. A semi-elective pericardiectomy was performed.
Autopsy Findings
Submitted for examination was a rectangular segment of gray-tan tissue measuring 9.5 x 8.5 x 0.3 cm. The outer surface was fatty in appearance. The inner surface was rough and covered by a number of fine red papillary projections. The projections were composed of fine strands having the appearance of fibrin.
Histopathological Findings


See Also
- Hemopericardium
- Pneumopericardium
- Chylopericardium
- Pericardial effusion
- Congenital absence of the pericardium
- Pericardial window
- Pericardial sac
- Pericardial friction rub
- Pericardiectomy
- Pericardiocentesis
- Pericardium
Source
References
- ↑ Reuter H, Burgess L, van Vuuren W, Doubell A. (2006). "Diagnosing tuberculous pericarditis". Q J Med. 99: 827&ndash, 39. PMID 17121764.
- ↑ Cinar B, Enc Y, Goksel O, Cimen S, Ketenci B, Teskin O, Kutlu H, Eren E. (2006). "Chronic constrictive tuberculous pericarditis: risk factors and outcome of pericardiectomy". Int J Tuberc Lung Dis. 10 (6): 701–6. PMID 16776460.
- ↑ Chowdhury UK, Subramaniam GK, Kumar AS, Airan B, Singh R, Talwar S, Seth S, Mishra PK, Pradeep KK, Sathia S, Venugopal P (2006). "Pericardiectomy for constrictive pericarditis: a clinical, echocardiographic, and hemodynamic evaluation of two surgical techniques". Ann Thorac Surg. 81 (2): 522–9. doi:10.1016/j.athoracsur.2005.08.009. PMID 16427843.
- ↑ Ling LH, Oh JK, Schaff HV, Danielson GK, Mahoney DW, Seward JB, Tajik AJ (1999). "Constrictive pericarditis in the modern era: evolving clinical spectrum and impact on outcome after pericardiectomy". Circulation. 100 (13): 1380–6. PMID 10500037.
Acknowledgements
The content on this page was first contributed by C. Michael Gibson, M.S., M.D.
Additional Resources
- Adler Y, Finkelstein Y, Guindo J, de la Serna R, Shoenfeld Y, Bayes-Genis A, Sagie A, Bayes de Luna A, Spodick DH. Colchicine treatment for recurrent pericarditis: a decade of experience. Circulation. 1998;97:2183–2185.
- Applegate RJ, Johnston WE, Vinten-Johansen J, Klopfenstein HS, Little WC. Restraining effect of intact pericardium during acute volume leading. Am J Physiol. 1992;262:H1725–H1733.
- Artom G, Koren-Morag N, Spodick DH, Brucato A, Guindo J, Bayesde-Luna A, Brambilla G, Finkelstein Y, Granel B, Bayes-Genis A, Schwammenthal E, Adler Y. Pretreatment with corticosteroids attenuates the efficacy of colchicine in preventing recurrent pericarditis: a multicentre all-case analysis. Eur Heart J. 2005;26:723–727.
- Arunasalam S, Siegel RJ. Rapid resolution of symptomatic acute pericarditis with ketorolac tromethamine: a parenteral nonsteroidal antiinflammatory agent. Am Heart J. 1993;125(pt 1):1455–1458.
- Bonnefoy E, Gordon P, Kirkorian G, Fatemi M, Chevalier P, Touboul P. Serum cardiac troponin I and ST-segment elevation in patients with acute pericarditis. Eur Heart J. 2000;21:832–836.
- Correale E, Maggioni AP, Romano S, Ricciardiello V, Battista R, Salvarola G, Santoro E, Tognoni G, on behalf of the Gruppo Italiano perlo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI). Comparison of frequency, diagnostic and prognostic significance of pericardial involvement in acute myocardial infarction treated with and without thrombolytics. Am J Cardiol. 1993;71:1377–1381.
- Fowler NO. Tuberculous pericarditis. JAMA. 1991;266:99 –103.
- Freeman GL, LeWinter MM. Determinants of the intrapericardial pressure in dogs. J Appl Physiol. 1986;60:758 –764.
- Freeman GL, LeWinter MM. Pericardial adaptations during chronic cardiac dilation in dogs. Circ Res. 1984;54:294 –300.
- Freeman GL, Little WC. Comparison of in situ and in vitro studies of pericardial pressure-volume relation in the dog. Am J Physiol. 1986;251: H421–H427.
- Gunukula SR, Spodick DH. Pericardial disease in renal patients. Semin Nephrol. 2001;21:52–56.
- Hoit BD, Gabel M, Fowler NO. Cardiac tamponade in left ventricular dysfunction. Circulation. 1990;82:1370–1376.
- Imazio M, Bobbio M, Cecchi E, Demarie D, Demichellis B, Pomari F, Moratti M, Gaschino G, Giammaria M, Ghiso A, Belli R, Trinchero R. Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) Trial. Circulation. 2005;112:2012–2016.
- Imazio M, Demichellis B, Cecchi E, Belli R, Ghisio A, Bobbio M, Trinchero R. Cardiac troponin I in acute pericarditis. J Am Coll Cardiol. 2003;42:2144–2148.
- Imazio M, Demichellis B, Parrini I, Gluggia M, Cecchi E, Gaschino G, Demarie D, Ghislo A, Trinchero R. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol. 2004;43:1042–1046.
- Jerjes-Sanchez C, Ramirez-Rivera A, Ibarra-Perez C. The Dressler syndrome after pulmonary embolism. Am J Cardiol. 1996;78:343–345.
- Kansal S, Roitman D, Sheffield LT. Two-dimensional echocardiography of congenital absence of pericardium. Am Heart J. 1985;109:912–915.
- Klopfenstein HS, Schuchard GH, Wann LS, Palmer TE, Hartz AJ, Gross CM, Singh S, Brooks HL. The relative merits of pulsus paradoxus and right ventricular diastolic collapse in the early detection of cardiac tamponade: an experimental echocardiographic study. Circulation. 1985;71: 829–833.
- Knopf WD, Talley JD, Murphy DA. An echo-dense mass in the pericardial space as a sign of left ventricular free wall rupture during acute myocardial infarction. Am J Cardiol. 1987;59:1202.
- Lange RA, Hillis D. Acute pericarditis. N Engl J Med. 2004;351: 2195–2202.
- LeWinter MM, Kabbani S. Pericardial diseases. In: Zipes DP, Libby P, Bonow RO, Braunwald E, eds. Braunwald’s Heart Disease. 7th ed. Philadelphia, Pa: Elsevier Saunders; 2005:1757–1780.
- Maisch B, Ristic D, Pankuweit S. Intrapericardial treatment of autoreactive pericardial effusion with triamcinolone. Eur Heart J. 2002;23: 1503–1508.
- Maisch B, Seferovic PM, Ristic AD, Erbel R, Rienmuller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH, for the Task Force on the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology. Guidelines on the diagnosis and management of pericardial diseases: executive summary. Eur Heart J. 2004;25:587– 610.
- Maisch B. Recurrent pericarditis: mysterious or not so mysterious? Eur Heart J. 2005;26:631– 633.
- Mandell BF. Cardiovascular involvement in systemic lupus erythematosus. Semin Arthritis Rheum. 1987;17:126 –141.
- Miyazaki T, Pride HP, Zipes DP. Prostaglandins in the pericardial fluid modulate neural regulation of cardiac electrophysiological properties. Circ Res. 1990;66:163–175.
- Park JH, Choo SJ, Park SW. Acute pericarditis caused by acrylic bone cement after percutaneous vertebroplasty. Circulation. 2005; 111:e98.
- Permanyer-Miralda G, Sagrista-Sauleda J, Soler-Soler J. Primary acute pericardial disease: a prospective series of 231 consecutive patients. Am J Cardiol. 1985;56:623– 630.
- Permanyer-Miralda G. Acute pericardial disease: approach to the aetiologic diagnosis. Heart. 2004;90:252–254.
- Reddy PS, Curtiss EI, O’Toole JD, Shaver JA. Cardiac tamponade: hemodynamic observations in man. Circulation. 1978;58:265–272.
- Reddy PS, Curtiss EI, Uretsky BF. Spectrum of hemodynamic changes in cardiac tamponade. Am J Cardiol. 1990;66:1487–1491.
- Shabetai R, Fowler NO, Guntheroth WG. The hemodynamics of cardiac tamponade and constrictive pericarditis. Am J Cardiol. 1970;26: 480–489.
- Shabetai R. Pericardial effusion: haemodynamic spectrum. Heart. 2004; 90:255–256.
- Shabetai R. Recurrent pericarditis: recent advances and remaining questions. Circulation. 2005;112:1921–1923.
- Singh S, Wann S, Schuchard GH, Klopfenstein HS, Leimgruber PP, Keelan MH, Brooks HL. Right ventricular and right atrial collapse in patients with cardiac tamponade: a combined echocardiographic and hemodynamic study. Circulation. 1984;70:966–971.
- Spodick DH. Acute cardiac tamponade. N Engl J Med. 2003;349: 684–690.
- Spodick DH. Acute pericarditis: current concepts and practice. JAMA. 2003;289:1150 –1153.
- Spodick DH. Intrapericardial treatment of persistent autoreactive pericarditis / myopericarditis and pericardial effusion. Eur Heart J. 2002;23: 1481–1482.
- Spodick DH. Macrophysiology, microphysiology, and anatomy of the pericardium: a synopsis. Am Heart J. 1992;124:1046 –1051.
- Troughton RW, Asher CR, Klein AL. Pericarditis. Lancet. 2004;363: 717–727.
- Tsang TS, Barnes ME, Hayes SN, Freeman WK, Dearani JA, Butler SL, Seward JB. Clinical and echocardiographic characteristics of significant pericardial effusions following cardiothoracic surgery and outcomes of echo-guided pericardiocentesis for management: Mayo Clinic experience, 1979–1998. Chest. 1999;116:322–331.
- Tsang TS, Oh JK, Seward JB, Tajik AJ. Diagnostic value of echocardiography in cardiac tamponade. Herz. 2000;25:734–740.
- Zayas R, Anguita M, Torres F, Gimenez D, Bergillos F, Ruiz M, Ciudad M, Gallardo A, Valles F. Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol. 1995;75:378 –382.
Suggested Links and Web Resources
- Pericarditis - Mayo Clinic series
- Pericarditis - cardiologychannel.com
- Pericarditis information from Seattle Children's Hospital Heart Center
- Pulsus paradoxus - Journal of Postgraduate Medicine
- http://en.wikipedia.org/wiki/Pericarditis
- SeeMyHeart - Patient Information on Echocardiograms (Heart Ultrasounds)
- American Society of Echocardiography
- Stress Test with Echocardiography from Angioplasty.Org
- Echocardiography information from Children's Hospital Heart Center, Seattle.
- Coronary heart disease And echocardiography
- Echocardiography Resources Simple echocardiography tutorials
- Atlas of Echocardiography Echocardiography Database
- E-chocardiography Internet Journal of Cardiac Ultrasound
- Echobasics Basic introduction to echocardiography - German/Spanish English planned for 2007
- Echocardiography Basic information about echocardiography - HealthwoRx
For Patients
de:Perikarditis
nl:Pericarditis
sv:Hjärtsäcksinflammation