Mycosis fungoides differential diagnosis
|
Cutaneous T cell lymphoma Microchapters |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sowminya Arikapudi, M.B,B.S. [2]
Overview
Cutaneous T cell lymphoma must be differentiated from other diseases such as eczema and psoriasis.
Differentiating Cutaneous T cell lymphoma from other Diseases
- Mycosis fangoides must be differentiated from other diseases such as:[1][2][3][4][5]
- Sezaruy syndrome
- Sezaruy syndrome is more symptoI contrast to patch or plaque MF, SS is much more symptomatic. Sezary syndrome patients tend to present with diffuse skin involvement,not like mycosis fungoides usually evolve through patches and plaques to erythroderma [6]
- In Sezary syndrome infiltration of skin is generally much less dense than plaque in mycosis fungoides (MF)
- Eczema
- Psoriasis
- Pityriasis rubra pilaris
- dermatitis
- Hypereosinophilic syndrome
- Adult T-cell leukemia
- Atopic dermatitis
- Contact dermatitis
- Chronic actinic dermatitis
- Scabies
- Drug eruption
- Graft versus host disease
- Sezaruy syndrome
| Disease | Rash Characteristics | Signs and Symptoms | Associated Conditions | Rash Appearance |
|---|---|---|---|---|
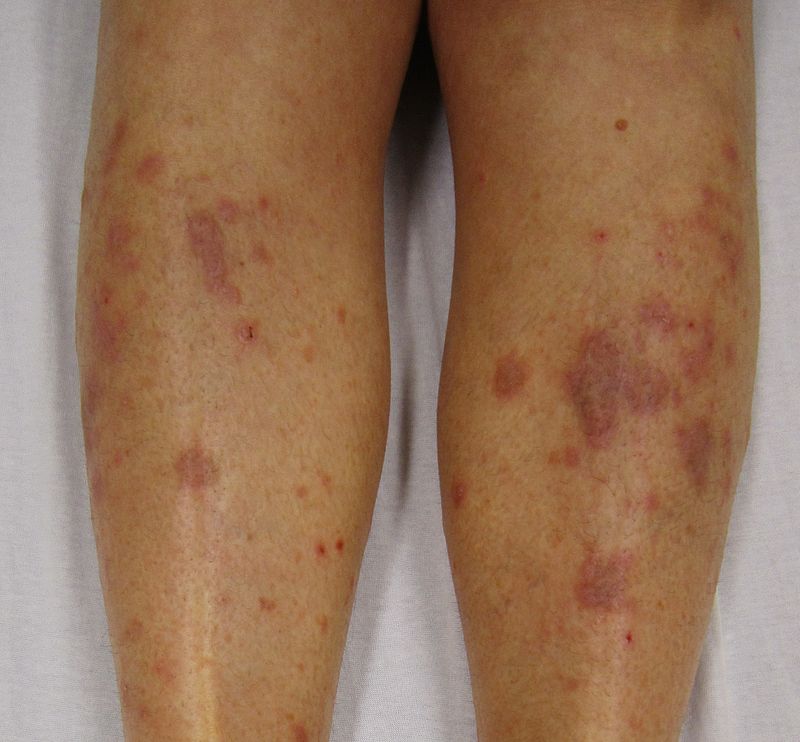
| Cutaneous T cell lymphoma/Mycosis fungoides[7] |
|
|
||
| Pityriasis rosea[8] |
|
|
||
| Pityriasis lichenoides chronica |
|
|
||
| Nummular dermatitis[11] |
|
|
|
|
| Secondary syphilis[12] |
|
|
||
| Bowen’s disease[13] |
|
|
||
| Exanthematous pustulosis[15] |
|
|
||
| Hypertrophic lichen planus[17] |
|
|
|
|
| Sneddon–Wilkinson disease[19] |
|
|
||
| Small plaque parapsoriasis[23] |
|
|
|
|
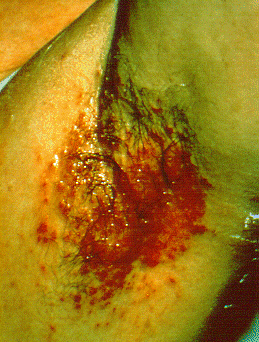
| Intertrigo[25] |
|
|
||
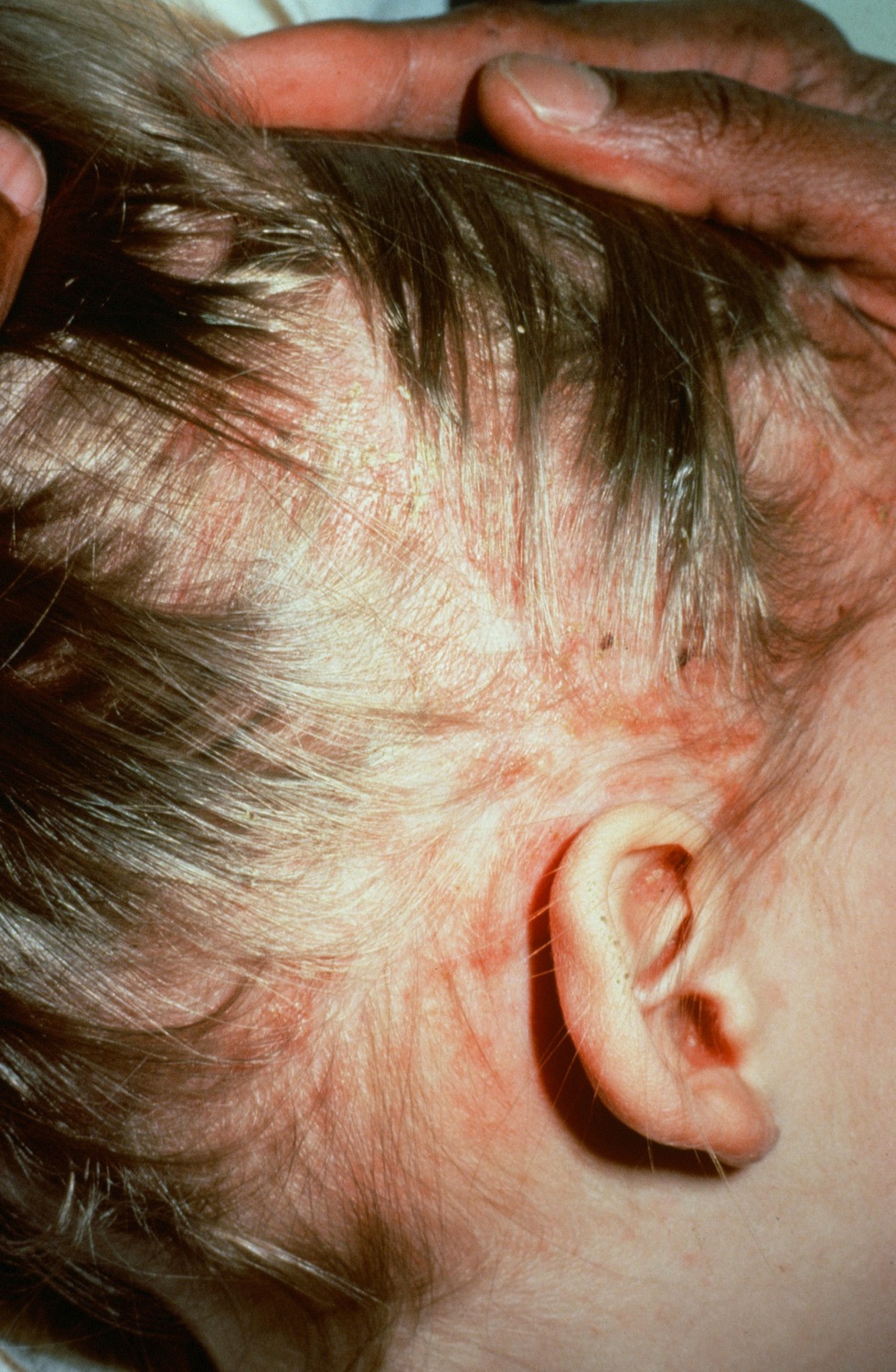
| Langerhans cell histiocytosis[26] |
|
|
|
|
| Tinea manuum/pedum/capitis[30] |
|
|
|
|
| Seborrheic dermatitis |
|
|
References
- ↑ Yamashita T, Abbade LP, Marques ME, Marques SA (2012). "Mycosis fungoides and Sézary syndrome: clinical, histopathological and immunohistochemical review and update". An Bras Dermatol. 87 (6): 817–28, quiz 829–30. PMC 3699909. PMID 23197199.
- ↑ Olek-Hrab K, Silny W (March 2014). "Diagnostics in mycosis fungoides and Sezary syndrome". Rep Pract Oncol Radiother. 19 (2): 72–6. doi:10.1016/j.rpor.2013.11.001. PMC 4054990. PMID 24936324.
- ↑ Klemke CD, Brade J, Weckesser S, Sachse MM, Booken N, Neumaier M, Goerdt S, Nebe TC (September 2008). "The diagnosis of Sézary syndrome on peripheral blood by flow cytometry requires the use of multiple markers". Br. J. Dermatol. 159 (4): 871–80. doi:10.1111/j.1365-2133.2008.08739.x. PMID 18652582.
- ↑ Scala E, Abeni D, Palazzo P, Liso M, Pomponi D, Lombardo G, Picchio MC, Narducci MG, Russo G, Mari A (2012). "Specific IgE toward allergenic molecules is a new prognostic marker in patients with Sézary syndrome". Int. Arch. Allergy Immunol. 157 (2): 159–67. doi:10.1159/000327553. PMID 21985996.
- ↑ Chu AC, Robinson D, Hawk JL, Meacham R, Spittle MF, Smith NP (February 1986). "Immunologic differentiation of the Sézary syndrome due to cutaneous T-cell lymphoma and chronic actinic dermatitis". J. Invest. Dermatol. 86 (2): 134–7. PMID 3528307.
- ↑ Chand K, Sayal SK, Chand S (April 2007). "Cutaneous T-Cell Lymphoma (Mycosis Fungoides)". Med J Armed Forces India. 63 (2): 188–90. doi:10.1016/S0377-1237(07)80076-1. PMC 4925357. PMID 27407986.
- ↑ "Mycosis Fungoides and the Sézary Syndrome Treatment (PDQ®)—Patient Version - National Cancer Institute".
- ↑ Mahajan K, Relhan V, Relhan AK, Garg VK (2016). "Pityriasis Rosea: An Update on Etiopathogenesis and Management of Difficult Aspects". Indian J Dermatol. 61 (4): 375–84. doi:10.4103/0019-5154.185699. PMC 4966395. PMID 27512182.
- ↑ Prantsidis A, Rigopoulos D, Papatheodorou G, Menounos P, Gregoriou S, Alexiou-Mousatou I, Katsambas A (2009). "Detection of human herpesvirus 8 in the skin of patients with pityriasis rosea". Acta Derm. Venereol. 89 (6): 604–6. doi:10.2340/00015555-0703. PMID 19997691.
- ↑ Smith KJ, Nelson A, Skelton H, Yeager J, Wagner KF (1997). "Pityriasis lichenoides et varioliformis acuta in HIV-1+ patients: a marker of early stage disease. The Military Medical Consortium for the Advancement of Retroviral Research (MMCARR)". Int. J. Dermatol. 36 (2): 104–9. PMID 9109005.
- ↑ Jiamton S, Tangjaturonrusamee C, Kulthanan K (2013). "Clinical features and aggravating factors in nummular eczema in Thais". Asian Pac. J. Allergy Immunol. 31 (1): 36–42. PMID 23517392.
- ↑ "STD Facts - Syphilis".
- ↑ Neagu TP, Ţigliş M, Botezatu D, Enache V, Cobilinschi CO, Vâlcea-Precup MS, GrinŢescu IM (2017). "Clinical, histological and therapeutic features of Bowen's disease". Rom J Morphol Embryol. 58 (1): 33–40. PMID 28523295.
- ↑ Murao K, Yoshioka R, Kubo Y (2014). "Human papillomavirus infection in Bowen disease: negative p53 expression, not p16(INK4a) overexpression, is correlated with human papillomavirus-associated Bowen disease". J. Dermatol. 41 (10): 878–84. doi:10.1111/1346-8138.12613. PMID 25201325.
- ↑ Szatkowski J, Schwartz RA (2015). "Acute generalized exanthematous pustulosis (AGEP): A review and update". J. Am. Acad. Dermatol. 73 (5): 843–8. doi:10.1016/j.jaad.2015.07.017. PMID 26354880.
- ↑ Schmid S, Kuechler PC, Britschgi M, Steiner UC, Yawalkar N, Limat A, Baltensperger K, Braathen L, Pichler WJ (2002). "Acute generalized exanthematous pustulosis: role of cytotoxic T cells in pustule formation". Am. J. Pathol. 161 (6): 2079–86. doi:10.1016/S0002-9440(10)64486-0. PMC 1850901. PMID 12466124.
- ↑ Ankad BS, Beergouder SL (2016). "Hypertrophic lichen planus versus prurigo nodularis: a dermoscopic perspective". Dermatol Pract Concept. 6 (2): 9–15. doi:10.5826/dpc.0602a03. PMC 4866621. PMID 27222766.
- ↑ Shengyuan L, Songpo Y, Wen W, Wenjing T, Haitao Z, Binyou W (2009). "Hepatitis C virus and lichen planus: a reciprocal association determined by a meta-analysis". Arch Dermatol. 145 (9): 1040–7. doi:10.1001/archdermatol.2009.200. PMID 19770446.
- ↑ Lutz ME, Daoud MS, McEvoy MT, Gibson LE (1998). "Subcorneal pustular dermatosis: a clinical study of ten patients". Cutis. 61 (4): 203–8. PMID 9564592.
- ↑ Kasha EE, Epinette WW (1988). "Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) in association with a monoclonal IgA gammopathy: a report and review of the literature". J. Am. Acad. Dermatol. 19 (5 Pt 1): 854–8. PMID 3056995.
- ↑ Delaporte E, Colombel JF, Nguyen-Mailfer C, Piette F, Cortot A, Bergoend H (1992). "Subcorneal pustular dermatosis in a patient with Crohn's disease". Acta Derm. Venereol. 72 (4): 301–2. PMID 1357895.
- ↑ Sauder MB, Glassman SJ (2013). "Palmoplantar subcorneal pustular dermatosis following adalimumab therapy for rheumatoid arthritis". Int. J. Dermatol. 52 (5): 624–8. doi:10.1111/j.1365-4632.2012.05707.x. PMID 23489057.
- ↑ Lambert WC, Everett MA (1981). "The nosology of parapsoriasis". J. Am. Acad. Dermatol. 5 (4): 373–95. PMID 7026622.
- ↑ Väkevä L, Sarna S, Vaalasti A, Pukkala E, Kariniemi AL, Ranki A (2005). "A retrospective study of the probability of the evolution of parapsoriasis en plaques into mycosis fungoides". Acta Derm. Venereol. 85 (4): 318–23. doi:10.1080/00015550510030087. PMID 16191852.
- ↑ Janniger CK, Schwartz RA, Szepietowski JC, Reich A (2005). "Intertrigo and common secondary skin infections". Am Fam Physician. 72 (5): 833–8. PMID 16156342.
- ↑ Satter EK, High WA (2008). "Langerhans cell histiocytosis: a review of the current recommendations of the Histiocyte Society". Pediatr Dermatol. 25 (3): 291–5. doi:10.1111/j.1525-1470.2008.00669.x. PMID 18577030.
- ↑ Stull MA, Kransdorf MJ, Devaney KO (1992). "Langerhans cell histiocytosis of bone". Radiographics. 12 (4): 801–23. doi:10.1148/radiographics.12.4.1636041. PMID 1636041.
- ↑ Sholl LM, Hornick JL, Pinkus JL, Pinkus GS, Padera RF (2007). "Immunohistochemical analysis of langerin in langerhans cell histiocytosis and pulmonary inflammatory and infectious diseases". Am. J. Surg. Pathol. 31 (6): 947–52. doi:10.1097/01.pas.0000249443.82971.bb. PMID 17527085.
- ↑ Grois N, Pötschger U, Prosch H, Minkov M, Arico M, Braier J, Henter JI, Janka-Schaub G, Ladisch S, Ritter J, Steiner M, Unger E, Gadner H (2006). "Risk factors for diabetes insipidus in langerhans cell histiocytosis". Pediatr Blood Cancer. 46 (2): 228–33. doi:10.1002/pbc.20425. PMID 16047354.
- ↑ Al Hasan M, Fitzgerald SM, Saoudian M, Krishnaswamy G (2004). "Dermatology for the practicing allergist: Tinea pedis and its complications". Clin Mol Allergy. 2 (1): 5. doi:10.1186/1476-7961-2-5. PMC 419368. PMID 15050029.
- ↑ Schwartz RA, Janusz CA, Janniger CK (2006). "Seborrheic dermatitis: an overview". Am Fam Physician. 74 (1): 125–30. PMID 16848386.
- ↑ Misery L, Touboul S, Vinçot C, Dutray S, Rolland-Jacob G, Consoli SG, Farcet Y, Feton-Danou N, Cardinaud F, Callot V, De La Chapelle C, Pomey-Rey D, Consoli SM (2007). "[Stress and seborrheic dermatitis]". Ann Dermatol Venereol (in French). 134 (11): 833–7. PMID 18033062.