Long QT Syndrome overview
|
Long QT Syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Long QT Syndrome overview On the Web |
|
American Roentgen Ray Society Images of Long QT Syndrome overview |
|
Risk calculators and risk factors for Long QT Syndrome overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]
Overview
The long QT syndrome (LQTS) is a heart condition associated with prolongation of repolarisation (recovery) following depolarisation (excitation) of the cardiac ventricles. It is associated with syncope (fainting) and sudden death due toventricular arrhythmias. Arrhythmias in individuals with LQTS are often associated with exercise or excitement. LQTS is associated with the rare, ventricular arrhythmia torsade de pointes, which can deteriorate into ventricular fibrillation and ultimately death.
Individuals with LQTS have a prolongation of the QT interval on the ECG. The Q wave on the ECG corresponds to ventricular depolarization while the T wave corresponds to ventricular repolarization. The QT interval is measured from the Q point to the end of the T wave. While many individuals with LQTS have persistent prolongation of the QT interval, some individuals do not always show the QT prolongation; in these individuals, the QT interval may prolong with the administration of certain medications.
Classification
There are multiple genetic mutations that account for LQTs, but LQT1, LQT2, and LQT3 account for 75% of cases of LQT.
LQT1
LQT1 is the most common type of long QT syndrome, making up about 40 to 55 percent of all cases. This variant will sometimes come to the attention of the cardiologist following a cardiac event during exercise like swimming. The LQT1 gene is KCNQ1 which has been isolated to chromosome 11p15.5. KCNQ1 codes for the voltage-gated potassium channel KvLQT1 that is highly expressed in the heart. It is believed that the product of the KCNQ1 gene produces an alpha subunit that interacts with other proteins (particularly the minK beta subunit) to create the IKs ion channel, which is responsible for the delayed potassium rectifier current of the cardiac action potential.
Mutations to the KCNQ1 gene can be inherited in an autosomal dominant or an autosomal recessive pattern in the same family. In the autosomal recessive mutation of this gene,homozygous mutations in KVLQT1 leads to severe prolongation of the QT interval (due to near-complete loss of the IKs ion channel), and is associated with increased risk of ventricular arrhythmias and congenital deafness. This variant of LQT1 is known as the Jervell and Lange-Nielsen syndrome.
Most individuals with LQT1 show paradoxical prolongation of the QT interval with infusion of epinephrine. This can also unmark latent carriers of the LQT1 gene.
Many missense mutations of the LQT1 gene have been identified. These are often associated with a high risk percentage of symptomatic carriers and sudden death.
LQT2
The LQT2 type is the second most common gene location that is affected in long QT syndrome, making up about 35 to 45 percent of all cases. This variant will sometimes come to the attention of the cardiologist as a result of a cardiac event during the post partum period or after being triggered by an alarm clock. This form of long QT syndrome most likely involves mutations of the human ether-a-go-go related gene (HERG) on chromosome 7. The HERG gene (also known as KCNH2) is part of the rapid component of the potassium rectifying current (IKr). (The IKr current is mainly responsible for the termination of the cardiac action potential, and therefore the length of the QT interval.) The normally functioning HERG gene allows protection against early after depolarizations (EADs).
Most drugs that cause long QT syndrome do so by blocking the IKr current via the HERG gene. These include erythromycin, terfenadine, andketoconazole. The HERG channel is very sensitive to unintended drug binding due to two aromatic amino acids, the tyrosine at position 652 and the phenylalanine at position 656. These amino acid residues are poised so drug binding to them will block the channel from conducting current. Other potassium channels do not have these residues in these positions and are therefore not as prone to blockage.
LQT3
The LQT3 type of long QT syndrome accounts for 5-10% of cases, and cardiac events can occur during sleep. This variant involves a mutation of the gene that encodes the alpha subunit of the Na+ ion channel. This gene is located on chromosome 3p21-24, and is known as SCN5A (also hH1 and NaV1.5). The mutations involved in LQT3 slow the inactivation of the Na+ channel, resulting in prolongation of the Na+ influx during depolarization. Paradoxically, the mutant sodium channels inactivate more quickly, and may open repetitively during the action potential.
A large number of mutations have been characterized as leading to or predisposing LQT3. Calcium has been suggested as a regulator of SCN5A, and the effects of calcium on SCN5A may begin to explain the mechanism by which some these mutations cause LQT3. Furthermore mutations in SCN5A can cause Brugada syndrome, cardiac conduction disease anddilated cardiomyopathy. Rarely some affected individuals can have combinations of these diseases.
Pathophysiology
The pathophysiology of Long QT syndrome involves an inhereted or congenital abnormality in the ion channels leading to prolongation of the action potential and early after depolarization. There is also an imbalance in the sympathetic innervation of heart.
Associated syndromes
A number of syndromes are associated with LQTS.
Jervell and Lange-Nielsen syndrome
The Jervell and Lange-Nielsen syndrome (JLNS) is an autosomal recessive form of LQTS with associated congenital deafness. It is caused specifically by mutation of the KCNE1 and KCNQ1 genes
In untreated individuals with JLNS, about 50 percent die by the age of 15 years due to ventricular arrhythmias.
Romano-Ward syndrome
Romano-Ward syndrome is an autosomal dominant form of LQTS that is not associated with deafness.
Differentiating Long QT Syndrome from Other Disorders
There are multiple causes of QT prolongation that are distinct from Long QT syndrome such as drugs (anti-arrhythmic drugs, anti-psychotic drugs), electrolyte disturbances (hyperkalaemia, hypocalcaemia, hypoglycaemia, hypokalaemia, and hypomagnesemia), neurologic events such as subarachnoid hemorrhage, and anorexia nervosa.
Epidemiology and Demographics
The prevalence of LQTs is 50/100,000 individuals (i.e. 1:2,000).
Risk Stratification
The genetic variant (LQT1-8), the gender and the QT interval are associated with the risk of a cardiac event. A history of prior events (syncope, fainting spells, seizures, sudden death) and a family history of cardiac events are associated with an increased risk of subsequent cardiac events.
Risk Factors for Torsade de Pointes and Sudden Cardiac Death
- Persons with a history of repeated fainting episodes or syncope. If there are more than 2 fainting spells in under 2 years, the risk of an aborted SCD or SCD is increased 18 fold.[1]
- Repeated blackouts or fainting spells in the context of the following are due to a malignant arrhythmia until proven otherwise:
- Exertion
- Loud startling noise
- Postpartum syncope
- Seizures
- A prior history of cardiac arrest.
- Family members of persons with repeated fainting, accidents, seizures or a history of cardiac arrest.
- Persons who are on certain medications that are known to cause a prolonged QT interval on electrocardiogram.
- Persons who are first degree relatives of people with know long QT syndrome.
- Persons who suffer from anorexia nervosa, or who have low levels of magnesium, calcium or potassium in their blood
Natural History
About half the patients with long QT syndrome will have an arrhythmia that degenerates into Torsade de Pointes that may terminate spontaneously or may end in sudden cardiac death.
Complications
Long QT syndrome can result in fatal heart arrhythmias and death. Certain medications can increase the risk of fatal arrhythmias and death in persons with long QT syndrome.
List of Medications to be Avoided in Congenital Long QT Syndrome
- Albuterol
- Alfuzosin
- Amantadine
- Amiodarone
- Amisulpride
- Amitriptyline
- Amphetamine
- Arsenic trioxide
- Artenimol + piperaquine
- Astemizole
- Atazanavir
- Atomoxetine
- Azithromycin
- Bepridil
- Chloral hydrate
- Chloroquine
- Chlorpromazine
- Ciprofloxacin
- Cisapride
- Citalopram
- Clarithromycin
- Clomipramine
- Clozapine
- Cocaine
- Desipramine
- Dexmethylphenidate
- Diphenhydramine
- Diphenhydramine
- Disopyramide
- Dobutamine
- Dofetilide
- Dolasetron
- Domperidone
- Dopamine
- Doxepin
- Dronedarone
- Droperidol
- Ephedrine
- Epinephrine
- Eribulin
- Erythromycin
- Escitalopram
- Famotidine
- Fenfluramine
- Fingolimod
- Flecainide
- Fluconazole
- Fluoxetine
- Foscarnet
- Fosphenytoin
- Galantamine
- Gatifloxacin
- Gemifloxacin
- Granisetron
- Halofantrine
- Haloperidol
- Ibutilide
- Iloperidone
- Imipramine
- Indapamide
- Isoproterenol
- Isradipine
- Itraconazole
- Ketoconazole
- Lapatinib
- Levalbuterol
- Levofloxacin
- Levomethadyl
- Lisdexamfetamine
- Lithium
- Mesoridazine
- Metaproterenol
- Methadone
- Methylphenidate
- Midodrine
- Mirtazapine
- Moexipril / HCTZ
- Moxifloxacin
- Nicardipine
- Nilotinib
- Norepinephrine
- Nortriptyline
- Octreotide
- Ofloxacin
- Ondansetron
- Oxytocin
- Paliperidone
- Paroxetine
- Pentamidine
- Perflutren lipid microspheres
- Phentermine
- Phenylephrine
- Phenylpropanolamine
- Pimozide
- Probucol
- Procainamide
- Protriptyline
- Pseudoephedrine
- Quetiapine
- Quinidine
- Ranolazine
- Ritodrine
- Ritonavir
- Roxithromycin
- Salmeterol
- Sertindole
- Sertraline
- Sevoflurane
- Sibutramine
- Solifenacin
- Sotalol
- Sparfloxacin
- Sunitinib
- Tacrolimus
- Tamoxifen
- Telithromycin
- Terbutaline
- Terfenadine
- Thioridazine
- Tizanidine
- Tolterodine
- Trazodone
- Trimethoprim-Sulfamethoxazole
- Trimipramine
- Vandetanib
- Vardenafil
- Venlafaxine
- Voriconazole
- Ziprasidone
Prognosis
People who are treated with lifestyle modifications and medications live longer than those who are not. For people who are not treated, half of them, mostly those with the inherited form of long QT syndrome, will die within 10 years.
The Jervell and Lange-Nielsen syndrome (JLNS) is an autosomal recessive form of LQTS with associated congenital deafness. It is caused specifically by mutation of the KCNE1 and KCNQ1 genes. In untreated individuals with JLNS, about 50 percent die by the age of 15 years due to ventricular arrhythmias.
Diagnosis
History
You should inquire about the following as part of the thistory:
- Persons with a history of repeated fainting episodes or syncope. If there are more than 2 fainting spells in under 2 years, the risk of an aborted SCD or SCD is increased 18 fold.[2]
- Repeated blackouts or fainting spells in the context of the following are due to a malignant arrhythmia until proven otherwise:
- Exertion
- Loud startling noise
- Postpartum syncope
- Seizures
- A prior history of cardiac arrest.
- Family members of persons with repeated fainting, accidents, seizures or a history of cardiac arrest.
- Persons who are on certain medications that are known to cause a prolonged QT interval on electrocardiogram.
- Persons who are first degree relatives of people with know long QT syndrome.
Symptoms
- Fainting - fainting or syncope is the most common symptom in persons with long QT syndrome. The fainting can occur spontaneously without warning, or in response to certain stressors such as emotional stress, exercise, excitement or loud noises. Often when people are about to faint, they may experience lightheadedness, heart palpitations, blurred vision or weakness.
- Seizures - if the heart continues to beat abnormally, the brain can become deprived of oxygen, which can then cause seizures.
- Sudden death - in some circumstances a fatal arrhytmia that is not quickly intervened on, may cause sudden death.
Electrocardiography
The diagnosis of LQTS is difficult in so far as 2.5% of the healthy population have a prolonged QT interval, and 10% of LQTS patients have a normal QT interval (known as concealed LQTs). The presence of LQTs in the absence of QT prolongation (concealed LQTs) underscores the importance of genetic testing in the diagnosis of LQTs. It should be noted that the QT interval is often overestimated in the presence of a u wave.
How to Measure the QT
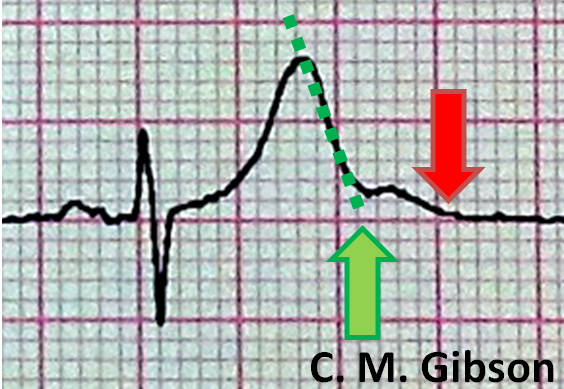
The QT interval is often measured incorrectly. It is measured incorrectly by 33% of EP physicians and 75% of general cardiologists. It is measured incorrectly by <5% of Long QT syndrome experts who deal with this on a frequent basis. [3] The presence of a U wave can often lead to a false diagnosis of QT prolongation. In order to avoid this, the "teach the tangent" or "avoid the tail" rule is applied. In this method, a line is drawn on top of the downslope of the T wave as shown below with the dotted green line. The QT interval is measured where this green dotted line intersects with the isoelectric line as shown by the large green arrow. The red arrow is an incorrect assessment of the QT interval at the end of the U wave. Using the red arrow would lead to a misdiagnosis of QT prolongation.
The LQTS Diagnostic Score
A commonly used criterion to diagnose LQTS is the LQTS "diagnostic score". Its based on several criteria giving points to each. With 4 or more points the probability is high for LQTS, and with 1 or less point the probability is low. Two or 3 points indicates intermediate probability.
- QTc (Defined as QT interval / square root of RR interval)
- >= 480 msec - 3 points
- 460-470 msec - 2 points
- 450 msec and male gender - 1 point
- Torsades de Pointes ventricular tachycardia - 2 points
- T wave alternans - 1 point
- Notched T wave in at least 3 leads - 1 point
- Low heart rate for age (children) - 0.5 points
- Syncope (one cannot receive points both for syncope and Torsades de pointes)
- With stress - 2 points
- Without stress - 1 point
- Congenital deafness - 0.5 points
- Family history (the same family member cannot be counted for LQTS and sudden death)
- Other family members with definite LQTS - 1 point
- Sudden death in immediate family (members before the age 30) - 0.5 points
Electrocardiographic Examples of the Long QT Variants
Shown below are examples of ECGs demonstrating QT prolongation in Long QT syndrome.
- LQT 1 shows 'early onset' broad based, slowly generated T waves
- LQT 2 shows small late T waves. Sometimes these T waves will be notched or double humped in lead V4.
- LQT 3 shows a flat and prolonged ST segment with a 'late onset' T wave that is normal in configuration.
