Leukemia: Difference between revisions
No edit summary |
m (Bot: Removing from Primary care) |
||
| (135 intermediate revisions by 17 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | {{Leukemia}} | ||
}} | |||
'''For patient information click [[Leukemia (patient information)|here]]''' | |||
{{ | {{CMG}}; {{AE}} {{SMP}}, {{USAMA}}, {{SSH}}; {{GRR}} {{Nat}} | ||
{{SK}} Leukaemia | |||
==Overview== | ==Overview== | ||
'''Leukemia | '''Leukemia''' (Greek leukos, “white”; haima, “blood”) can be defined as a group of [[hematopoietic stem cell]] [[malignancies]] due to [[genetic]] abnormalities that may lead to clonal proliferation of these cells. These group of diseases are classified based on the type of [[hematopoietic stem cell]] involved and the duration of the disease. The leukemias are the most common malignancies among children younger than 15 years. Among them, [[ALL|Acute Lymphoblastic Leukemia (ALL)]] is the most common leukemia and accounts for 77% of childhood leukemia. However, [[CLL|Chronic Lymphocytic Leukemia (CLL)]] is the most common form of leukemia in adults, and it accounts for 30% of all leukemias in the United States. The increased rate of proliferation and decreased rate of [[apoptosis]] in this progeny of cells may compromise normal [[bone marrow]] function and ultimately result in marrow failure. Clinical manifestations, diagnosis, laboratory findings, and therapy are different according to the type of malignancy. | ||
== | ==Classification== | ||
Leukemia may be classified as follows: | |||
<br><br> | |||
{{Family tree/start}} | |||
{{Family tree | | | | | | | | | B01 | | | |B01= Leukemia}} | |||
{{Family tree | | | | |,|-|-|-|-|^|-|-|-|-|.| | }} | |||
{{Family tree | | | | C01 | | | | | | | | C02 |C01= Lymphoid progeny| C02= Myeloid progeny}} | |||
{{Family tree | |,|-|-|^|-|-|.| | | |,|-|-|^|-|-|.| | }} | |||
{{Family tree | D01 | | | | D02 | | D03 | | | | D04 | D01= [[Acute lymphoblastic leukemia]] (ALL) | D02= [[Chronic lymphocytic leukemia]] (CLL) | D03= [[Acute Myeloid Leukemia]] (AML) | D04= [[Chronic myeloid leukemia]] (CML)}} | |||
{{Family tree/end}} | |||
<br><br><br> | |||
==Differentiating Leukemia from other Diseases== | |||
Leukemia must be differentiated from various diseases that cause [[weight loss]], [[night sweats]], [[hepatosplenomegaly]], and palpable [[lymph node]]s, such as [[hairy cell leukaemia|hairy cell leukemia]], prolymphocytic leukemia, [[follicular lymphoma]], and [[mantle cell lymphoma]]. Based on the expression of cell surface markers, the table below differentiates different types of leukemia from other diseases that cause similar clinical presentations:<ref name="H">Hoffbrand V, Moss P. Essential Haematology. John Wiley & Sons; 2011</ref> | |||
The | {| | ||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" + |Disease | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" + |Etiology | |||
! colspan="4" align="center" style="background:#4479BA; color: #FFFFFF;" + |Clinical Manifestation | |||
! colspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" + |Laboratory Findings | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" + |Gold standard diagnosis | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;" + |Associated findings | |||
|- | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Demography | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |History | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Symptoms | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Signs | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Lab | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Histopathology | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Acute myelogenous leukemia]]<ref name="pmid30410824">{{cite journal |vauthors=Saif A, Kazmi SFA, Naseem R, Shah H, Butt MO |title=Acute Myeloid Leukemia: Is That All There Is? |journal=Cureus |volume=10 |issue=8 |pages=e3198 |date=August 2018 |pmid=30410824 |doi=10.7759/cureus.3198 |url=}}</ref><ref name="pmid23526416">{{cite journal |vauthors=Estey EH |title=Acute myeloid leukemia: 2013 update on risk-stratification and management |journal=Am. J. Hematol. |volume=88 |issue=4 |pages=318–27 |date=April 2013 |pmid=23526416 |doi=10.1002/ajh.23404 |url=}}</ref> | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Clonal proliferation of malignant myeloid blast cells in the [[bone marrow]] | |||
* Genetic abnormalities t(8;21), inv(16), and t(15;17) | |||
| align="left" style="background:#F5F5F5;" + | | |||
* The most common leukemia in adults | |||
* Median age of 63 years old | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Smoking]], previous [[chemotherapy]] or [[radiation therapy]], [[myelodysplastic syndrome]], and exposure to the chemical [[benzene]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Fatigue]] | |||
* [[Bleeding]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Bone [[tenderness]] | |||
* [[Dyspnea]] | |||
* Leukemia cutis | |||
* Swelling of the [[Gingiva|gums]] | |||
* Chloroma | |||
* Rare LAP | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Anemia]] | |||
* [[Thrombocytopenia]] | |||
* [[Leukocytosis]] or [[leukopenia]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Leukemic blasts | |||
* Positive [[Auer rod|Auer rods]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Flow cytometry]] > 20% blasts of [[myeloid]] lineage | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Persistent or frequent [[infections]] | |||
* Fatal within weeks or months if left untreated | |||
* [[Down syndrome]] or [[Bloom syndrome]] | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Acute lymphoblastic leukemia]]<ref name="pmid30302234">{{cite journal |vauthors=Sawalha Y, Advani AS |title=Management of older adults with acute lymphoblastic leukemia: challenges & current approaches |journal=Int J Hematol Oncol |volume=7 |issue=1 |pages=IJH02 |date=March 2018 |pmid=30302234 |pmc=6176956 |doi=10.2217/ijh-2017-0023 |url=}}</ref><ref name="pmid23841506">{{cite journal |vauthors=Portell CA, Advani AS |title=Novel targeted therapies in acute lymphoblastic leukemia |journal=Leuk. Lymphoma |volume=55 |issue=4 |pages=737–48 |date=April 2014 |pmid=23841506 |doi=10.3109/10428194.2013.823493 |url=}}</ref> | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Arrest of [[lymphoblasts]] | |||
* Chromosomal translocations: t(9;22) , t(12;21), t(5;14), t(1;19) | |||
| align="left" style="background:#F5F5F5;" + | | |||
* The most common cancer in children | |||
*Peak 2-5 years of age | |||
*Boys > girls | |||
| align="left" style="background:#F5F5F5;" + | | |||
* History of [[cancer]] | |||
* History of drug exposure | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Generalized [[weakness]] | |||
* [[Fatigue]] | |||
* [[Bleeding]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Hepatosplenomegaly]] | |||
* [[Lymphadenopathy|LAP]] | |||
* [[Dyspnea]] | |||
* [[Pallor]] | |||
* [[Papilledema]] | |||
* [[Meningism|Nuchal rigidity]] | |||
* [[Cranial nerve palsy]] | |||
* [[Testicle|Testicular]] enlargement | |||
* [[Mediastinal mass]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Anemia]] | |||
* [[Thrombocytopenia]] | |||
* Normal or slightly increased [[White blood cells|WBC]] counts | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Lymphoblast|Lymphoblasts]] | |||
* Atypical cells | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Bone marrow examination|Bone marrow biopsy]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[CNS]] involvement | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Chronic myelogenous leukemia]]<ref name="pmid25814082">{{cite journal |vauthors=Saußele S, Silver RT |title=Management of chronic myeloid leukemia in blast crisis |journal=Ann. Hematol. |volume=94 Suppl 2 |issue= |pages=S159–65 |date=April 2015 |pmid=25814082 |doi=10.1007/s00277-015-2324-0 |url=}}</ref><ref name="pmid30285354">{{cite journal |vauthors=Eden RE, Coviello JM |title= |journal= |volume= |issue= |pages= |date= |pmid=30285354 |doi= |url=}}</ref> | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Dysregulated production and uncontrolled proliferation of mature and maturing [[Granulocyte|granulocytes]] | |||
* [[BCR/ABL|BCR-ABL1]] fusion gene | |||
* [[Dominance relationship|Autosomal dominant]] mutation | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Median age 50 years old | |||
| align="center" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Generalized weakness | |||
* [[Fatigue]] | |||
* [[Satiety|Early satiety]] | |||
* Abdominal fullness | |||
* Bleeding | |||
| align="left" style="background:#F5F5F5;" + | | |||
*Asymptomatic | |||
*[[Blast crisis]] | |||
*Excessive [[Perspiration|sweating]] | |||
* [[Papilledema]] | |||
* [[Tenderness]] over the lower [[sternum]] | |||
* [[Hepatosplenomegaly]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Anemia]] | |||
* [[White blood cells|WBC]] > 100,000/microL | |||
* Absolute [[basophilia]] and [[eosinophilia]] | |||
* [[Platelet|Plt]] > 600,000 to 700,000/microL | |||
* Low [[leukocyte alkaline phosphatase]] | |||
* High [[uric acid]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* All cells of the neutrophilic series, from [[Myeloblast|myeloblasts]] to mature [[Neutrophil|neutrophils]] | |||
* [[Myelocyte]] bulge | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Bone marrow examination|Bone marrow biopsy]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Acute [[Gout|gouty arthritis]] | |||
* Venous obstruction | |||
|- | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Disease | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Etiology | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Demography | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |History | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Symptoms | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Signs | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Lab | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Histopathology | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Gold standard diagnosis | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Associated findings | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |'''[[Chronic lymphocytic leukemia]]'''<ref name="pmid266906142">{{cite journal |vauthors=Rai KR, Jain P |title=Chronic lymphocytic leukemia (CLL)-Then and now |journal=Am. J. Hematol. |volume=91 |issue=3 |pages=330–40 |date=March 2016 |pmid=26690614 |doi=10.1002/ajh.24282 |url=}}</ref> | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Progressive accumulation of monoclonal [[B cell|B lymphocytes]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* The most common leukemia in adults in western countries | |||
* M > F | |||
* Median age 70 years old | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Positive family history | |||
* Exposure to [[Herbicide|herbicides]] or [[Insecticide|insecticides]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Bleeding | |||
* Abdominal pain | |||
* Generalized [[weakness]] | |||
* [[Anorexia]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* LAP (Most common sign) | |||
* [[Hepatosplenomegaly]] | |||
* [[Skin lesion|Skin lesions]] (leukemia cutis) | |||
* [[Sleep hyperhidrosis|Night sweats]] | |||
* [[Muscle wasting]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Anemia]] | |||
* [[Thrombocytopenia]] | |||
* Absolute [[lymphocytosis]] >5000 cells/μl | |||
* [[Neutropenia]] | |||
* Positive direct Coombs test | |||
* [[Hypogammaglobulinemia]] | |||
* Elevated [[lactate dehydrogenase]] and [[beta-2 microglobulin]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Presence of smudge cells | |||
* Monoclonality of [[Light chain|kappa]] and [[Lambda (anatomy)|lambda]] producing [[B cell|B cells]] | |||
* Express [[CD19]], [[CD20]], [[CD23]], and [[CD5]] on the [[cell]] surface | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Flow cytometry]] of the [[Venous blood|peripheral blood]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Extranodal involvement of [[skin]], [[kidney]], [[lung]], [[Spinal cord|spine]] | |||
* [[Membranoproliferative glomerulonephritis]] | |||
* [[Autoimmune hemolytic anemia]] | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Hairy cell leukemia]]<ref name="pmid29110361">{{cite journal |vauthors=Troussard X, Cornet E |title=Hairy cell leukemia 2018: Update on diagnosis, risk-stratification, and treatment |journal=Am. J. Hematol. |volume=92 |issue=12 |pages=1382–1390 |date=December 2017 |pmid=29110361 |pmc=5698705 |doi=10.1002/ajh.24936 |url=}}</ref><ref name="pmid29118233">{{cite journal |vauthors=Wierda WG, Byrd JC, Abramson JS, Bhat S, Bociek G, Brander D, Brown J, Chanan-Khan A, Coutre SE, Davis RS, Fletcher CD, Hill B, Kahl BS, Kamdar M, Kaplan LD, Khan N, Kipps TJ, Lancet J, Ma S, Malek S, Mosse C, Shadman M, Siddiqi T, Stephens D, Wagner N, Zelenetz AD, Dwyer MA, Sundar H |title=Hairy Cell Leukemia, Version 2.2018, NCCN Clinical Practice Guidelines in Oncology |journal=J Natl Compr Canc Netw |volume=15 |issue=11 |pages=1414–1427 |date=November 2017 |pmid=29118233 |doi=10.6004/jnccn.2017.0165 |url=}}</ref> | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Accumulation of small mature [[B cell]] lymphoid cells with abundant [[cytoplasm]] and "hairy" projections | |||
* [[BRAF]] mutation | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Uncommon | |||
* Median age 50 to 55 years old | |||
* M >> F | |||
* More common in Caucasians than Blacks | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Exposures to [[ionizing radiation]], [[Pesticide|pesticides]], and farming | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Generalized weakness | |||
* [[Fatigue]] | |||
* [[Satiety|Early satiety]] | |||
* Abdominal fullness | |||
* Bleeding | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Asymptomatic | |||
* [[Splenomegaly]] | |||
* Spontaneous [[splenic rupture]] | |||
* [[Rash|Skin rash]] | |||
* [[Ascites]] | |||
* [[Pleural effusion]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Cytopenia]] | |||
* [[Leukocytosis]] in 10 to 20 percent | |||
* [[Azotemia]] | |||
* Abnormal [[liver function tests]] | |||
* [[Hypergammaglobulinemia]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Pancytopenia]] with [[monocytopenia]] and circulating tumor cells characteristic of HCL | |||
* Dry [[bone marrow]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Analysis of [[Venous blood|peripheral blood]] + [[immunophenotyping]] by [[flow cytometry]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Vasculitis]] | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |Large granular lymphocytic leukemia<ref name="pmid28128670">{{cite journal |vauthors=Matutes E |title=Large granular lymphocytic leukemia. Current diagnostic and therapeutic approaches and novel treatment options |journal=Expert Rev Hematol |volume=10 |issue=3 |pages=251–258 |date=March 2017 |pmid=28128670 |doi=10.1080/17474086.2017.1284585 |url=}}</ref><ref name="pmid28717070">{{cite journal |vauthors=Oshimi K |title=Clinical Features, Pathogenesis, and Treatment of Large Granular Lymphocyte Leukemias |journal=Intern. Med. |volume=56 |issue=14 |pages=1759–1769 |date=2017 |pmid=28717070 |pmc=5548667 |doi=10.2169/internalmedicine.56.8881 |url=}}</ref> | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Clonal proliferation of [[Cytotoxic T cell|cytotoxic T cells]] | |||
* Dysregulation of [[apoptosis]] through abnormalities in the Fas/Fas ligand pathway | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Rare | |||
* Median age 60 years | |||
* M = F | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Autoimmune diseases | |||
* [[Lymphoproliferative disorders|Lymphoproliferative]] disorders | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Generalized [[weakness]] | |||
* [[Fatigue]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Mostly asymptomatic | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Modest [[lymphocytosis]] | |||
* [[Neutropenia]] | |||
* [[Anemia]] | |||
* [[Thrombocytopenia]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Large [[Lymphocyte|lymphocytes]] with a condensed round or oval nucleus, abundant pale basophilic cytoplasm, and small azurophilic granules | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Biopsy and flow cytometry + T-cell receptor gene rearrangement studies | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Recurrent bacterial infection | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Chronic neutrophilic leukemia]]<ref name="pmid29512199">{{cite journal |vauthors=Elliott MA, Tefferi A |title=Chronic neutrophilic leukemia: 2018 update on diagnosis, molecular genetics and management |journal=Am. J. Hematol. |volume=93 |issue=4 |pages=578–587 |date=August 2018 |pmid=29512199 |doi=10.1002/ajh.24983 |url=}}</ref> | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Mature granulocytic proliferation in the blood and [[bone marrow]] | |||
* Point mutations in the [[CSF3R]] gene | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Very rare | |||
* M = F | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Multiple myeloma]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Generalized [[weakness]] | |||
* [[Fatigue]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Hepatosplenomegaly]] | |||
* [[Pruritus]] | |||
* [[Gout]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Peripheral blood [[neutrophilia]] (> 25 x 10<sup>9</sup>/L) with myeloid precursors (promyelocytes, myelocytes, metamyelocytes) | |||
* Elevated [[leukocyte alkaline phosphatase]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Toxic granulation in the [[Neutrophil|neutrophils]] | |||
* Nuclear hypersegmentation | |||
* Increased myeloid:erythroid ratio > 20:1 | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[World Health Organization|WHO]] diagnostic criteria include leukocytosis of ≥ 25 x 109/L | |||
* More than 80% neutrophils, | |||
* Less than 10% circulating neutrophil precursors with blasts | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Poor prognosis | |||
* Absence of the Philadelphia chromosome or a BCR/ABL fusion gene | |||
|- | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Disease | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Etiology | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Demography | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |History | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Symptoms | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Signs | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Lab | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Histopathology | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Gold standard diagnosis | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Associated findings | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Chronic eosinophilic leukemia]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* There is no known cause for chronic eosinophilic leukemia. | |||
* It hasn't been linked to a specific chromosome or genetic abnormality. | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Unknown | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Unknown | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Constitutional | |||
* [[Rash]] | |||
* [[Rhinitis]] | |||
* [[Gastritis]] | |||
* [[Thromboembolism]]<nowiki/>related | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Hypertension]] | |||
* [[Eczema]], [[mucosal]][[ulcers]], [[erythema]] | |||
* [[Angioedema]] | |||
* [[Ataxia]] | |||
* [[Anemia]] | |||
* [[Lymphadenopathy]] | |||
* [[Hepatosplenomegaly]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
*[[Leukocytosis]] with left shift | |||
*[[Eosinophilia]] | |||
*[[Basophilia]] | |||
*[[Monocytosis]] | |||
*[[Anemia]] | |||
*[[Thrombocytopenia]] | |||
*↑ [[B12]] levels | |||
*↑ [[LDH]] | |||
== | | align="left" style="background:#F5F5F5;" + | | ||
* Hypercelluar with ↑ [[eosinophilic]]<nowiki/> precursors, ↑ [[eosinophils]], and atypical [[mononuclear cells]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* | | align="left" style="background:#F5F5F5;" + | | ||
*[[Heart failure]] [[Lung fibrosis]] | |||
*[[Encephalopathy]] | |||
*Erythema annulare centrifugam | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Chronic monocytic leukemia electrocardiogram|Chronic monocytic leukemia]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Prolymphocytic leukemia]] (PLL) | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[T-cell large granular lymphocyte leukemia|T-cell large granular lymphocytic leukemia]] (TLGL) | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
|- | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Disease | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Etiology | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Demography | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |History | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Symptoms | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Signs | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Lab | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Histopathology | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Gold standard diagnosis | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Associated findings | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Aggressive NK-cell leukemia]] (ANKL) | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Adult T-cell leukemia|Adult T-cell leukemia/lymphoma]] (ATLL)<ref name="wiki1">Human T-lymphotropic virus. Wikipedia (2015) https://en.wikipedia.org/wiki/Human_T-lymphotropic_virus#Transmission Accessed on November, 3 2015</ref><ref name="pmid18042693">{{cite journal |vauthors=Matutes E |title=Adult T-cell leukaemia/lymphoma |journal=J. Clin. Pathol. |volume=60 |issue=12 |pages=1373–7 |year=2007 |pmid=18042693 |pmc=2095573 |doi=10.1136/jcp.2007.052456 |url=}}</ref><ref name="wiki">Adult T-cell leukemia/lymphoma. Wikipedia (2015) https://en.wikipedia.org/wiki/Adult_T-cell_leukemia/lymphoma Accessed on November, 3 2015</ref><ref name="pmid20425378">{{cite journal| author=Mahieux R, Gessain A| title=Adult T-cell leukemia/lymphoma and HTLV-1. | journal=Curr Hematol Malig Rep | year= 2007 | volume= 2 | issue= 4 | pages= 257-64 | pmid=20425378 | doi=10.1007/s11899-007-0035-x | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20425378 }}</ref><ref name="wiki2">Adult T-cell leukemia/lymphoma. Wikipedia (2015) https://en.wikipedia.org/wiki/Adult_T-cell_leukemia/lymphoma Accessed on November, 3 2015</ref><ref name="pmid180426932">{{cite journal| author=Matutes E| title=Adult T-cell leukaemia/lymphoma. | journal=J Clin Pathol | year= 2007 | volume= 60 | issue= 12 | pages= 1373-7 | pmid=18042693 | doi=10.1136/jcp.2007.052456 | pmc=PMC2095573 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18042693 }}</ref> | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Adult T-cell leukemia is caused by an infection with [[HTLV]]. | |||
* Common [[genetic mutation]]s involved in the development of adult T-cell leukemia can be found [[Adult T-cell leukemia pathophysiology|here]]. | |||
| align="left" style="background:#F5F5F5;" + | | |||
* The incidence of adult T-cell leukemia increases with age, and the median age at diagnosis is 57 years. | |||
* Males are more commonly affected with adult T-cell leukemia than females. | |||
* The male to female ratio is approximately 1.4 to 1. | |||
| align="left" style="background:#F5F5F5;" + | | |||
:* [[Abdominal pain]] | |||
:* [[Constipation]] | |||
:* [[Nausea]] and [[vomiting]] | |||
:* [[Fatigue]] | |||
:* Generalized [[weakness]] | |||
:* [[Cough]] | |||
:* Recurrent [[infection]]s | |||
| align="left" style="background:#F5F5F5;" + | | |||
:* [[Fever]] | |||
:* [[Weight loss]] | |||
:* Recurrent [[bleeding]] | |||
:* [[Anorexia]] | |||
:* [[Night sweat]]s | |||
:* [[Bone pain]] | |||
:* [[Hypercalcemia]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Sezary syndrome]]<ref name="pmid21883142">{{cite journal |vauthors=Wong HK, Mishra A, Hake T, Porcu P |title=Evolving insights in the pathogenesis and therapy of cutaneous T-cell lymphoma (mycosis fungoides and Sezary syndrome) |journal=Br. J. Haematol. |volume=155 |issue=2 |pages=150–66 |date=October 2011 |pmid=21883142 |pmc=4309373 |doi=10.1111/j.1365-2141.2011.08852.x |url=}}</ref><ref name="pmid27121473">{{cite journal |vauthors=Woollard WJ, Pullabhatla V, Lorenc A, Patel VM, Butler RM, Bayega A, Begum N, Bakr F, Dedhia K, Fisher J, Aguilar-Duran S, Flanagan C, Ghasemi AA, Hoffmann RM, Castillo-Mosquera N, Nuttall EA, Paul A, Roberts CA, Solomonidis EG, Tarrant R, Yoxall A, Beyers CZ, Ferreira S, Tosi I, Simpson MA, de Rinaldis E, Mitchell TJ, Whittaker SJ |title=Candidate driver genes involved in genome maintenance and DNA repair in Sézary syndrome |journal=Blood |volume=127 |issue=26 |pages=3387–97 |date=June 2016 |pmid=27121473 |doi=10.1182/blood-2016-02-699843 |url=}}</ref><ref name="pmid266071833">{{cite journal |vauthors=Wilcox RA |title=Cutaneous T-cell lymphoma: 2016 update on diagnosis, risk-stratification, and management |journal=Am. J. Hematol. |volume=91 |issue=1 |pages=151–65 |date=January 2016 |pmid=26607183 |pmc=4715621 |doi=10.1002/ajh.24233 |url=}}</ref><ref name="pmid25386354">{{cite journal |vauthors=Horesh N, Horowitz NA |title=Does gender matter in non-hodgkin lymphoma? Differences in epidemiology, clinical behavior, and therapy |journal=Rambam Maimonides Med J |volume=5 |issue=4 |pages=e0038 |date=October 2014 |pmid=25386354 |pmc=4222427 |doi=10.5041/RMMJ.10172 |url=}}</ref><ref name="pmid24421750">{{cite journal |vauthors=Al Hothali GI |title=Review of the treatment of mycosis fungoides and Sézary syndrome: A stage-based approach |journal=Int J Health Sci (Qassim) |volume=7 |issue=2 |pages=220–39 |date=June 2013 |pmid=24421750 |pmc=3883611 |doi= |url=}}</ref><ref name="pmid266071835">{{cite journal |vauthors=Wilcox RA |title=Cutaneous T-cell lymphoma: 2016 update on diagnosis, risk-stratification, and management |journal=Am. J. Hematol. |volume=91 |issue=1 |pages=151–65 |date=January 2016 |pmid=26607183 |pmc=4715621 |doi=10.1002/ajh.24233 |url=}}</ref><ref name="pmid231971992">{{cite journal |vauthors=Yamashita T, Abbade LP, Marques ME, Marques SA |title=Mycosis fungoides and Sézary syndrome: clinical, histopathological and immunohistochemical review and update |journal=An Bras Dermatol |volume=87 |issue=6 |pages=817–28; quiz 829–30 |date=2012 |pmid=23197199 |pmc=3699909 |doi= |url=}}</ref><ref name="pmid23074497">{{cite journal |vauthors= |title=Extracorporeal photophoresis: an evidence-based analysis |journal=Ont Health Technol Assess Ser |volume=6 |issue=6 |pages=1–82 |date=2006 |pmid=23074497 |pmc=3379535 |doi= |url=}}</ref> | |||
| align="left" style="background:#F5F5F5;" + | | |||
* The cause of Sezary syndrome has not been identified. | |||
* Sezary syndrome might have one or more of the [[chromosomal]] [[abnormalities]], such as the loss or gain of [[Genetics|genetic]]. | |||
| align="left" style="background:#F5F5F5;" + | | |||
* The prevalence of Sezary syndrome is exact unknown. | |||
*The median age at diagnosis of [[Sézary syndrome]] is 60 years of age. | |||
*Sezary syndrome is more commonly observed among [[Old age|elderly]] [[Patient|patients]]. | |||
*[[Male|Males]] are more commonly affected with Sezary syndrome than [[Female|females]](2:1). | |||
| align="left" style="background:#F5F5F5;" + | | |||
*The majority of sezary syndrome [[Patient|patients]] present with developing [[lymphadenopathy]] and [[erythroderma]] for weeks to months. | |||
*Early clinical features of Sezary syndrome include: | |||
:*Mimic [[psoriasis]] | |||
:*[[Chronic (medical)|Chronic]] [[eczema]] | |||
:*[[Atopic dermatitis (patient information)|Atopic dermatitis]] | |||
:*[[Leprosy]] | |||
:*Lichenoid [[pityriasis]] | |||
*In Sezary syndrome single or multiple [[Lesion|lesions]] (thin [[erythematous]] [[Plaque|plaques]] or flat patch) is a typical [[skin]] involvement in the [[gluteal]] region or [[Thigh|thighs]]. <ref name="Olsen2015">{{cite journal|last1=Olsen|first1=Elise A.|title=Evaluation, Diagnosis, and Staging of Cutaneous Lymphoma|journal=Dermatologic Clinics|volume=33|issue=4|year=2015|pages=643–654|issn=07338635|doi=10.1016/j.det.2015.06.001}}</ref> | |||
*[[Patient|Patients]] with Sezary syndrome often have a history of several years of [[Eczema|eczematous]] or [[dermatitis]] [[skin]] [[Lesion|lesions]] before the [[diagnosis]] is finally established. | |||
| align="left" style="background:#F5F5F5;" + | | |||
* Widespread [[erythema]] | |||
** In Sezary syndrome widespread [[erythema]] can be finely scaly, indurated, or even resemble livido [[reticularis]] | |||
* Indurated | |||
* Resemble livido [[reticularis]] | |||
* [[Erythema]](Not seen in some [[Patient|patients]]) | |||
* The severity of [[erythema]] [[body surface area]] (BSA) involved may wax and wane(>80% of BSA) | |||
* | * Patches and [[Plaque|plaques]] to [[erythroderma]] | ||
* | * [[Keratosis pilaris]] | ||
* [[Alopecia]] ([[hair loss]]) | |||
* [[Ectropion]] | |||
* [[Keratoderma]] | |||
* [[Hypertrophy (medical)|Hypertrophic]] [[Nail (anatomy)|nails]] | |||
* Erosions | |||
* [[Lichenification]] | |||
* [[Trouble]] regulating [[Body Temperature|body temperature]] | |||
* [[Abnormal|Abnormalities]] of [[fingernails]] and [[toenails]] | |||
* [[Lymphadenopathy]] | |||
* [[Viscera|Viscer]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
|+ | | align="left" style="background:#F5F5F5;" + | | ||
! | | align="left" style="background:#F5F5F5;" + | | ||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Myelodysplastic syndrome]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
*Constitutional symptoms | |||
*[[Bleeding]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
*[[Pallor]] | |||
*[[Petechiae]] | |||
*[[Organomegaly]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
* [[Pancytopenia]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
*Hypercellular/ normocellular [[bone marrow]] with [[Dysplastic change|dysplastic]] changes | |||
*Macro-ovalocytes | |||
*Basophilic stippling | |||
*[[Howell-Jolly body]] | |||
| align="left" style="background:#F5F5F5;" + |Biopsy | |||
| align="left" style="background:#F5F5F5;" + | | |||
*[[Leukemia]] transformation | |||
*Acquired pseudo-Pelger-Huët anomaly | |||
*Infection | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Myeloproliferative disorders]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Leukemoid reaction]] | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
| align="left" style="background:#F5F5F5;" + | | |||
|} | |} | ||
==Epidemiology and Demographics== | |||
===Prevalence=== | |||
* | * In the United States, the age-adjusted [[prevalence]] of leukemia is 75.3 per 100,000 in 2011.<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | ||
===Incidence=== | |||
* | * The delay-adjusted [[incidence]] of leukemia in 2011 was estimated as 15.48 per 100,000 individuals in the United States. | ||
* | * In 2011, the age-adjusted incidence of leukemia was 13.66 per 100,000 individuals in the United States. | ||
===Age=== | |||
* The overall age-adjusted incidence of leukemia in the United States between 2007 and 2011 was 13 per 100,000 occurrences. The age-adjusted incidence of leukemia by age category is: | |||
** Under 65 years: 6.5 per 100,000 | |||
** 65 and over: 57.9 per 100,000 | |||
* | * Shown below is a table depicting the overall age-adjusted incidence of leukemia per 100,000 individuals by age in the United States between 2007 and 2011 for the different types of leukemia. | ||
{| style="cellpadding=0; cellspacing= 0; width: 600px;" | |||
|- | |||
| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" | || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Acute lymphoblastic leukemia'''|| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" | '''Chronic lymphocytic leukemia'''|| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Acute myeloid leukemia'''|| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Chronic myeloid leukemia''' | |||
|- | |||
| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''All ages'''|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" | 1.7 || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |4.4|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |3.8 || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |1.7 | |||
|- | |||
| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''<65''' || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |1.7 || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |1.4|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" | 1.8 || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |0.9 | |||
|- | |||
| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''≥65''' || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" | 1.6 || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |25.2 || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |17.5|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |6.8 | |||
|} | |||
===Gender=== | |||
* In the United States, the age-adjusted prevalence of leukemia by gender in 2011 was: | |||
** In males: 92.7 per 100,000 | |||
** In females: 60.7 per 100,000 | |||
* In the United States, the delay-adjusted incidence of leukemia by gender in 2011 was: | |||
** In males: 19.93 per 100,000 persons | |||
** In females: 11.89 per 100,000 persons | |||
* In the United States, the age-adjusted incidence of leukemia by gender on 2011 was: | |||
** In males: 17.58 per 100,000 persons | |||
** In females: 10.49 per 100,000 persons | |||
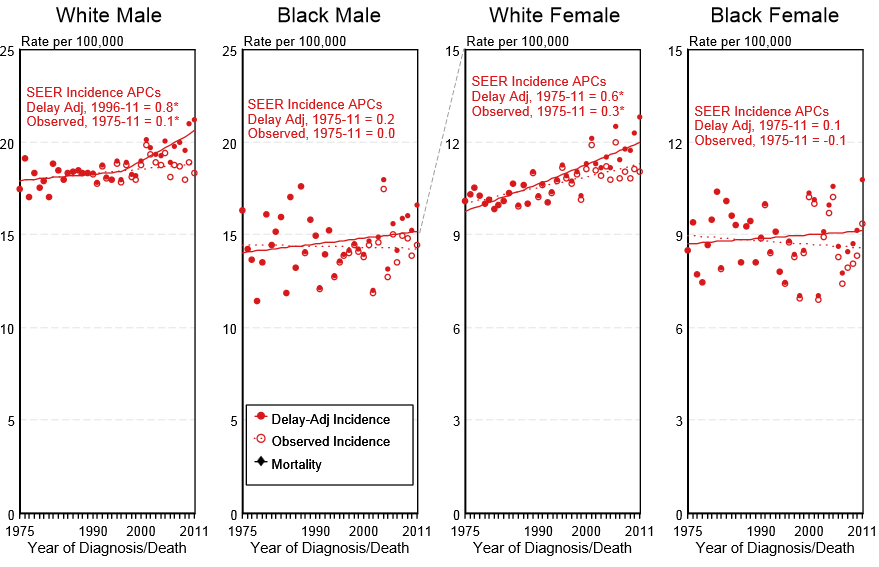
* Shown below is an image depicting the delay-adjusted incidence and observed incidence of leukemia by gender and race in the United States between 1975 and 2011. These graphs were gathered from [[SEER]]: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute. | |||
[[Image:Incidence of leukemia by gender and race in USA.PNG|700px|thumb|These graphs are adapted from [[SEER]]: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute. - Delay-adjusted [[incidence]] and observed [[incidence]] of leukemia by gender and race in the United States between 1975 and 2011]] | |||
==== | ===Race=== | ||
* Shown below is a table depicting the age-adjusted prevalence of leukemia by race in 2011 in the United States. | |||
{| style="cellpadding=0; cellspacing= 0; width: 600px;" | |||
|- | |||
| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" | || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''All Races''' || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''White''' || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Black''' || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Asian/Pacific Islander''' || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Hispanic''' | |||
|- | |||
| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Age-adjusted prevalence'''|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |75.3 per 100,000|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |83.5 per 100,000|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |45.9 per 100,000|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |41.2 per 100,000|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |57.1 per 100,000 | |||
|} | |||
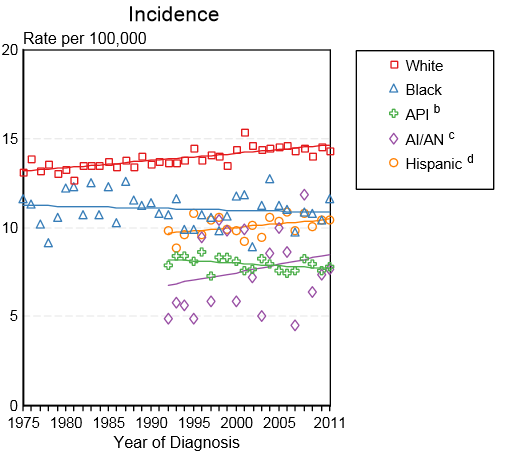
* Shown below is an image depicting the incidence of leukemia by race in the United States between 1975 and 2011. | |||
[[Image:Incidence of leukemia by race in USA.PNG|Incidence of leukemia by race in the United States between 1975 and 2011]] | |||
<small> API: Asian/Pacific Islander; AI/AN: American Indian/ Alaska Native</small> | |||
==== | ==Prognosis== | ||
===5-Year Survival=== | |||
* Between 2004 and 2010, the 5-year relative survival of patients with leukemia was 60.3%. | |||
* | * When stratified by age, the 5-year relative survival of patients with leukemia was 68.5% (44.1% for patients <65 and ≥ 65 years of age respectively). | ||
* Shown below is a table depicting the 5-year relative survival of patients by the type of leukemia in the United States between 2004 and 2010. | |||
{| style="cellpadding=0; cellspacing= 0; width: 800px;" | |||
|- | |||
| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" | || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Acute lymphoblastic leukemia'''|| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" | '''Chronic lymphocytic leukemia'''|| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Acute myeloid leukemia'''|| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Chronic myeloid leukemia''' | |||
|- | |||
=== | | style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''5-year survival'''|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="center" | 70% || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="center" |83.5%|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="center" |25.4% || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="center" |59.9% | ||
|} | |||
== | |||
''' | |||
''' | |||
''' | |||
# | |||
# | |||
''' | |||
== | |||
= | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Medicine]] | |||
[[Category: | |||
[[Category:Hematology]] | [[Category:Hematology]] | ||
[[Category: | [[Category:Immunology]] | ||
[[Category:Oncology]] | [[Category:Oncology]] | ||
[[Category:Up-To-Date]] | |||
[[ | [[Category:Differential diagnosis]] | ||
[[ | |||
Latest revision as of 22:30, 29 July 2020
|
Leukemia Microchapters |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Seyedmahdi Pahlavani, M.D. [2], Usama Talib, BSc, MD [3], Sadaf Sharfaei M.D.[4]; Grammar Reviewer: Natalie Harpenau, B.S.[5]
Synonyms and keywords: Leukaemia
Overview
Leukemia (Greek leukos, “white”; haima, “blood”) can be defined as a group of hematopoietic stem cell malignancies due to genetic abnormalities that may lead to clonal proliferation of these cells. These group of diseases are classified based on the type of hematopoietic stem cell involved and the duration of the disease. The leukemias are the most common malignancies among children younger than 15 years. Among them, Acute Lymphoblastic Leukemia (ALL) is the most common leukemia and accounts for 77% of childhood leukemia. However, Chronic Lymphocytic Leukemia (CLL) is the most common form of leukemia in adults, and it accounts for 30% of all leukemias in the United States. The increased rate of proliferation and decreased rate of apoptosis in this progeny of cells may compromise normal bone marrow function and ultimately result in marrow failure. Clinical manifestations, diagnosis, laboratory findings, and therapy are different according to the type of malignancy.
Classification
Leukemia may be classified as follows:
| Leukemia | |||||||||||||||||||||||||||||||||||||||
| Lymphoid progeny | Myeloid progeny | ||||||||||||||||||||||||||||||||||||||
| Acute lymphoblastic leukemia (ALL) | Chronic lymphocytic leukemia (CLL) | Acute Myeloid Leukemia (AML) | Chronic myeloid leukemia (CML) | ||||||||||||||||||||||||||||||||||||
Differentiating Leukemia from other Diseases
Leukemia must be differentiated from various diseases that cause weight loss, night sweats, hepatosplenomegaly, and palpable lymph nodes, such as hairy cell leukemia, prolymphocytic leukemia, follicular lymphoma, and mantle cell lymphoma. Based on the expression of cell surface markers, the table below differentiates different types of leukemia from other diseases that cause similar clinical presentations:[1]
| Disease | Etiology | Clinical Manifestation | Laboratory Findings | Gold standard diagnosis | Associated findings | ||||
|---|---|---|---|---|---|---|---|---|---|
| Demography | History | Symptoms | Signs | Lab | Histopathology | ||||
| Acute myelogenous leukemia[2][3] |
|
|
|
|
|
|
| ||
| Acute lymphoblastic leukemia[4][5] |
|
|
|
|
|
| |||
| Chronic myelogenous leukemia[6][7] |
|
|
|
|
|
|
| ||
| Disease | Etiology | Demography | History | Symptoms | Signs | Lab | Histopathology | Gold standard diagnosis | Associated findings |
| Chronic lymphocytic leukemia[8] |
|
|
|
|
|
|
| ||
| Hairy cell leukemia[9][10] |
|
|
|
|
|
|
|
||
| Large granular lymphocytic leukemia[11][12] |
|
|
|
|
|
|
| ||
| Chronic neutrophilic leukemia[13] |
|
|
|
|
|
| |||
| Disease | Etiology | Demography | History | Symptoms | Signs | Lab | Histopathology | Gold standard diagnosis | Associated findings |
| Chronic eosinophilic leukemia |
|
|
|
|
|
|
| ||
| Chronic monocytic leukemia | |||||||||
| Prolymphocytic leukemia (PLL) | |||||||||
| T-cell large granular lymphocytic leukemia (TLGL) | |||||||||
| Disease | Etiology | Demography | History | Symptoms | Signs | Lab | Histopathology | Gold standard diagnosis | Associated findings |
| Aggressive NK-cell leukemia (ANKL) | |||||||||
| Adult T-cell leukemia/lymphoma (ATLL)[14][15][16][17][18][19] |
|
|
|
||||||
| Sezary syndrome[20][21][22][23][24][25][26][27] |
|
|
|
|
|||||
| Myelodysplastic syndrome |
|
|
Biopsy |
| |||||
| Myeloproliferative disorders | |||||||||
| Leukemoid reaction | |||||||||
Epidemiology and Demographics
Prevalence
- In the United States, the age-adjusted prevalence of leukemia is 75.3 per 100,000 in 2011.[29]
Incidence
- The delay-adjusted incidence of leukemia in 2011 was estimated as 15.48 per 100,000 individuals in the United States.
- In 2011, the age-adjusted incidence of leukemia was 13.66 per 100,000 individuals in the United States.
Age
- The overall age-adjusted incidence of leukemia in the United States between 2007 and 2011 was 13 per 100,000 occurrences. The age-adjusted incidence of leukemia by age category is:
- Under 65 years: 6.5 per 100,000
- 65 and over: 57.9 per 100,000
- Shown below is a table depicting the overall age-adjusted incidence of leukemia per 100,000 individuals by age in the United States between 2007 and 2011 for the different types of leukemia.
| Acute lymphoblastic leukemia | Chronic lymphocytic leukemia | Acute myeloid leukemia | Chronic myeloid leukemia | |
| All ages | 1.7 | 4.4 | 3.8 | 1.7 |
| <65 | 1.7 | 1.4 | 1.8 | 0.9 |
| ≥65 | 1.6 | 25.2 | 17.5 | 6.8 |
Gender
- In the United States, the age-adjusted prevalence of leukemia by gender in 2011 was:
- In males: 92.7 per 100,000
- In females: 60.7 per 100,000
- In the United States, the delay-adjusted incidence of leukemia by gender in 2011 was:
- In males: 19.93 per 100,000 persons
- In females: 11.89 per 100,000 persons
- In the United States, the age-adjusted incidence of leukemia by gender on 2011 was:
- In males: 17.58 per 100,000 persons
- In females: 10.49 per 100,000 persons
- Shown below is an image depicting the delay-adjusted incidence and observed incidence of leukemia by gender and race in the United States between 1975 and 2011. These graphs were gathered from SEER: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute.
Race
- Shown below is a table depicting the age-adjusted prevalence of leukemia by race in 2011 in the United States.
| All Races | White | Black | Asian/Pacific Islander | Hispanic | |
| Age-adjusted prevalence | 75.3 per 100,000 | 83.5 per 100,000 | 45.9 per 100,000 | 41.2 per 100,000 | 57.1 per 100,000 |
- Shown below is an image depicting the incidence of leukemia by race in the United States between 1975 and 2011.
API: Asian/Pacific Islander; AI/AN: American Indian/ Alaska Native
Prognosis
5-Year Survival
- Between 2004 and 2010, the 5-year relative survival of patients with leukemia was 60.3%.
- When stratified by age, the 5-year relative survival of patients with leukemia was 68.5% (44.1% for patients <65 and ≥ 65 years of age respectively).
- Shown below is a table depicting the 5-year relative survival of patients by the type of leukemia in the United States between 2004 and 2010.
| Acute lymphoblastic leukemia | Chronic lymphocytic leukemia | Acute myeloid leukemia | Chronic myeloid leukemia | |
| 5-year survival | 70% | 83.5% | 25.4% | 59.9% |
References
- ↑ Hoffbrand V, Moss P. Essential Haematology. John Wiley & Sons; 2011
- ↑ Saif A, Kazmi S, Naseem R, Shah H, Butt MO (August 2018). "Acute Myeloid Leukemia: Is That All There Is?". Cureus. 10 (8): e3198. doi:10.7759/cureus.3198. PMID 30410824. Vancouver style error: initials (help)
- ↑ Estey EH (April 2013). "Acute myeloid leukemia: 2013 update on risk-stratification and management". Am. J. Hematol. 88 (4): 318–27. doi:10.1002/ajh.23404. PMID 23526416.
- ↑ Sawalha Y, Advani AS (March 2018). "Management of older adults with acute lymphoblastic leukemia: challenges & current approaches". Int J Hematol Oncol. 7 (1): IJH02. doi:10.2217/ijh-2017-0023. PMC 6176956. PMID 30302234.
- ↑ Portell CA, Advani AS (April 2014). "Novel targeted therapies in acute lymphoblastic leukemia". Leuk. Lymphoma. 55 (4): 737–48. doi:10.3109/10428194.2013.823493. PMID 23841506.
- ↑ Saußele S, Silver RT (April 2015). "Management of chronic myeloid leukemia in blast crisis". Ann. Hematol. 94 Suppl 2: S159–65. doi:10.1007/s00277-015-2324-0. PMID 25814082.
- ↑ Eden RE, Coviello JM. PMID 30285354. Missing or empty
|title=(help) - ↑ Rai KR, Jain P (March 2016). "Chronic lymphocytic leukemia (CLL)-Then and now". Am. J. Hematol. 91 (3): 330–40. doi:10.1002/ajh.24282. PMID 26690614.
- ↑ Troussard X, Cornet E (December 2017). "Hairy cell leukemia 2018: Update on diagnosis, risk-stratification, and treatment". Am. J. Hematol. 92 (12): 1382–1390. doi:10.1002/ajh.24936. PMC 5698705. PMID 29110361.
- ↑ Wierda WG, Byrd JC, Abramson JS, Bhat S, Bociek G, Brander D, Brown J, Chanan-Khan A, Coutre SE, Davis RS, Fletcher CD, Hill B, Kahl BS, Kamdar M, Kaplan LD, Khan N, Kipps TJ, Lancet J, Ma S, Malek S, Mosse C, Shadman M, Siddiqi T, Stephens D, Wagner N, Zelenetz AD, Dwyer MA, Sundar H (November 2017). "Hairy Cell Leukemia, Version 2.2018, NCCN Clinical Practice Guidelines in Oncology". J Natl Compr Canc Netw. 15 (11): 1414–1427. doi:10.6004/jnccn.2017.0165. PMID 29118233.
- ↑ Matutes E (March 2017). "Large granular lymphocytic leukemia. Current diagnostic and therapeutic approaches and novel treatment options". Expert Rev Hematol. 10 (3): 251–258. doi:10.1080/17474086.2017.1284585. PMID 28128670.
- ↑ Oshimi K (2017). "Clinical Features, Pathogenesis, and Treatment of Large Granular Lymphocyte Leukemias". Intern. Med. 56 (14): 1759–1769. doi:10.2169/internalmedicine.56.8881. PMC 5548667. PMID 28717070.
- ↑ Elliott MA, Tefferi A (August 2018). "Chronic neutrophilic leukemia: 2018 update on diagnosis, molecular genetics and management". Am. J. Hematol. 93 (4): 578–587. doi:10.1002/ajh.24983. PMID 29512199.
- ↑ Human T-lymphotropic virus. Wikipedia (2015) https://en.wikipedia.org/wiki/Human_T-lymphotropic_virus#Transmission Accessed on November, 3 2015
- ↑ Matutes E (2007). "Adult T-cell leukaemia/lymphoma". J. Clin. Pathol. 60 (12): 1373–7. doi:10.1136/jcp.2007.052456. PMC 2095573. PMID 18042693.
- ↑ Adult T-cell leukemia/lymphoma. Wikipedia (2015) https://en.wikipedia.org/wiki/Adult_T-cell_leukemia/lymphoma Accessed on November, 3 2015
- ↑ Mahieux R, Gessain A (2007). "Adult T-cell leukemia/lymphoma and HTLV-1". Curr Hematol Malig Rep. 2 (4): 257–64. doi:10.1007/s11899-007-0035-x. PMID 20425378.
- ↑ Adult T-cell leukemia/lymphoma. Wikipedia (2015) https://en.wikipedia.org/wiki/Adult_T-cell_leukemia/lymphoma Accessed on November, 3 2015
- ↑ Matutes E (2007). "Adult T-cell leukaemia/lymphoma". J Clin Pathol. 60 (12): 1373–7. doi:10.1136/jcp.2007.052456. PMC 2095573. PMID 18042693.
- ↑ Wong HK, Mishra A, Hake T, Porcu P (October 2011). "Evolving insights in the pathogenesis and therapy of cutaneous T-cell lymphoma (mycosis fungoides and Sezary syndrome)". Br. J. Haematol. 155 (2): 150–66. doi:10.1111/j.1365-2141.2011.08852.x. PMC 4309373. PMID 21883142.
- ↑ Woollard WJ, Pullabhatla V, Lorenc A, Patel VM, Butler RM, Bayega A, Begum N, Bakr F, Dedhia K, Fisher J, Aguilar-Duran S, Flanagan C, Ghasemi AA, Hoffmann RM, Castillo-Mosquera N, Nuttall EA, Paul A, Roberts CA, Solomonidis EG, Tarrant R, Yoxall A, Beyers CZ, Ferreira S, Tosi I, Simpson MA, de Rinaldis E, Mitchell TJ, Whittaker SJ (June 2016). "Candidate driver genes involved in genome maintenance and DNA repair in Sézary syndrome". Blood. 127 (26): 3387–97. doi:10.1182/blood-2016-02-699843. PMID 27121473.
- ↑ Wilcox RA (January 2016). "Cutaneous T-cell lymphoma: 2016 update on diagnosis, risk-stratification, and management". Am. J. Hematol. 91 (1): 151–65. doi:10.1002/ajh.24233. PMC 4715621. PMID 26607183.
- ↑ Horesh N, Horowitz NA (October 2014). "Does gender matter in non-hodgkin lymphoma? Differences in epidemiology, clinical behavior, and therapy". Rambam Maimonides Med J. 5 (4): e0038. doi:10.5041/RMMJ.10172. PMC 4222427. PMID 25386354.
- ↑ Al Hothali GI (June 2013). "Review of the treatment of mycosis fungoides and Sézary syndrome: A stage-based approach". Int J Health Sci (Qassim). 7 (2): 220–39. PMC 3883611. PMID 24421750.
- ↑ Wilcox RA (January 2016). "Cutaneous T-cell lymphoma: 2016 update on diagnosis, risk-stratification, and management". Am. J. Hematol. 91 (1): 151–65. doi:10.1002/ajh.24233. PMC 4715621. PMID 26607183.
- ↑ Yamashita T, Abbade LP, Marques ME, Marques SA (2012). "Mycosis fungoides and Sézary syndrome: clinical, histopathological and immunohistochemical review and update". An Bras Dermatol. 87 (6): 817–28, quiz 829–30. PMC 3699909. PMID 23197199.
- ↑ "Extracorporeal photophoresis: an evidence-based analysis". Ont Health Technol Assess Ser. 6 (6): 1–82. 2006. PMC 3379535. PMID 23074497.
- ↑ Olsen, Elise A. (2015). "Evaluation, Diagnosis, and Staging of Cutaneous Lymphoma". Dermatologic Clinics. 33 (4): 643–654. doi:10.1016/j.det.2015.06.001. ISSN 0733-8635.
- ↑ Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.