Leukemoid reaction
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Shyam Patel [2] Associate Editor(s)-in-Chief: Jogeet Singh Sekhon, M.D. [3]
Overview
Leukemoid reaction is a reversible increase in production of white blood cells in response to a stimulus, with white blood cell count of more than 25,000-30,000 per mm3 . Leukocytosis is increase in white blood cell count of more than 10,000 per mm3 and when the count exceeds 25,000 per mm3, with more than 2% immature white blood cells but absence of any blast cells, differentiating it from leukemias. Leukemoid reaction is classified according to the type of hematopoietic lineage of the bone marrow. Leukemoid reactions are mostly triggered by bacterial or viral infections. Leukemoid reaction is differentiated from leukemias by the absence of blast cells on peripheral blood film and high LAP score. Leukemoid reaction can lead to serious complications such as tumor lysis syndrome and DIC. The treatment includes treating the underlying cause and leukapheresis.
Historical Perspective
- Leukemoid reaction was discovered in 1926 by Krumbharr.
Classification
Leukemoid reaction can be classified according to the type of hematopoietic lineage of the bone marrow[1].
- Reactions of myeloid type:
- Neutrophilic leukemoid reactions
- Eosinophilic leukemoid reactions
- Reactions of lymphoid type:
- Lymphomonocytic leukemoid reactions
- Lymphocytic leukemoid reactions
- Plasmocytic leukemoid reactions
- Leukemoid reaction with blast cells
- Secondary (reactive) thrombocytosis
- Secondary erythrocytosis
- Mixed forms of leukemoid reactions
- Rare forms of leukemoid reaction
- Leukemoid reactions of basophilic type.
Pathophysiology
- Leukemoid reaction is a reversible increase in production of white blood cells in response to a stimulus, with white blood cell count of more than 25000-30000 per mm3[1].
- Leukocytosis is increase in white blood cell count of more than 10000 per mm3 and when the count exceeds 25000, with more than 2% immature white blood cells but absence of any blasts, differentiating it from leukemias.[2]
- Leukemoid reaction is classified according to the type of hematopoietic lineage of the bone marrow.
- It is a reactive, functional condition of hematopoietic, lymphatic and immune systems secondary to various diseases accompanied by the development of immature white blood cells in the peripheral blood.
- Leukemoid reaction is diagnosed after the exclusion of a malignant hematological disorder and is a transient condition. white blood cells return to normal when the underlying causes disappear.
- There are no signs of inhibition of normal hematopoiesis.
- Leukemoid reactions are mostly triggered by bacterial or viral infections, emergency stress irritants, and by various bacterial and non-bacterial stimulants causing sensitization.
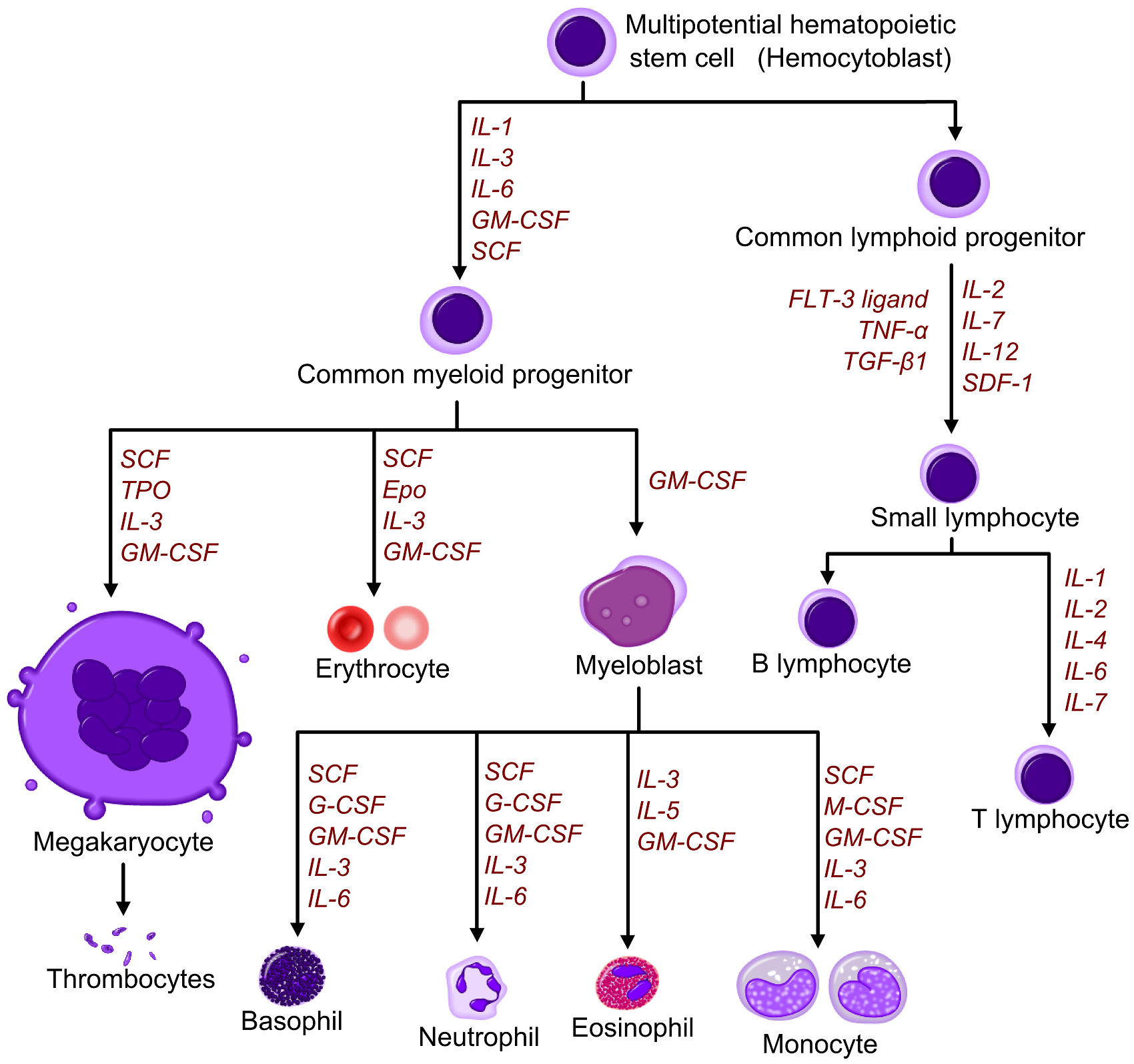
- The sensitization causes up-regulation of growth or survival factors (eg, granulocyte colony-stimulating factor, granulocyte-macrophage colony-stimulating factor, c-kit ligand), adhesion molecules (eg, CD11b/CD18), and various cytokines (eg, interleukin-1, interleukin-3, interleukin-6, interleukin-8, tumor necrosis factor).
- There is activation of normal hematopoiesis and excessive blood cells output to peripheral blood (reactive hyperplasia of leukopoietic tissue) and output of immature blood cells into peripheral blood.
- The image below demonstrates a graphic figure that illustrates hematopoietic growth factors in leukocytosis.[3]
- Reactions of myeloid type are characterized by a shift to the left, from an increased number of stab cells to singular blast cells with presence of all intermediate forms.
- There is an increase in immature granulocytes of myeloid lineage.
- Neutrophilic leukemoid reactions develop in Infections (sepsis, scarlet fever, abscess, diphtheria, lobar pneumonia, tuberculosis, dysentery, etc), exposure to ionizing radiation, Injuries of the skull, intoxication (uremia, CO poisoning), bone marrow metastases of malignant tumors[4][5].
- Eosinophilic reactions develop in allergic processes or in diseases with allergies, as well as in parasitic diseases. They are characterized by the development of a great number of eosinophils, about 90% of leukocytes.
- Lymphomonocytic leukemoid reactions develop in infectious mononucleosis, there are atypical mononuclear cells, called "lymphomonocytes" which are modulated T- and NK-lymphocytes, which get to the bloodstream by initiation of B lymphocytes. The number of atypical mononuclear cells can be increased in any viral infection[6].
- Lymphocytic leukemoid reactions develop in acute viral and bacterial infections and are characterized by leukocytosis with absolute lymphocytosis.
- Plasmocytic leukemoid reactions occur in diseases caused by protozoa (toxoplasmosis), viral infections (chickenpox, measles, rubella). Increased level of plasma cells (2%) in splenomegaly, blood and bone marrow.
- Leukemoid reactions with blast cells develop in severe viral infections (cytomegalovirus, etc.). Blast transformation of B-lymphocytes may be observed in the bone marrow, lymph nodes, and peripheral blood.
- Secondary absolute erythrocytosis is caused by increased erythropoiesis, relative hemoconcentration and polycythemia. It is characterized by increased red blood cell count.
- Secondary thrombocytosis is possible in malignant tumors, inflammatory diseases, following bleeding, hemolytic crises, after surgical operations and splenectomy.
Causes
- Neutrophilic leukemoid reactions [7][8][9][10]:
- Infections - sepsis, scarlet fever, abscess, diphtheria, lobar pneumonia, tuberculosis, dysentery
- Exposure to ionizing radiation.
- Injuries of the skull.
- Intoxication (uremia, CO-poisoning).
- Bone marrow metastases of malignant tumors - Lymphogranulomatosis
- Steroid hormones therapy
- Eosinophilic reactions :
- Lymphomonocytic leukemoid reactions:
- Lymphocytic leukemoid reaction:
- Plasmocytic leukemoid reactions:
- Diseases caused by protozoa (toxoplasmosis), and viral infections (chickenpox, measles, rubella).
- Thrombocytosis:
- Primary thrombocytosis- chronic myeloproliferative diseases.
- Secondary thrombocytosis-
- Malignant tumors
- Inflammatory diseases
- Following bleeding
- Hemolytic crises
- After surgical operations and splenectomy.
- Leukemoid reactions of basophilic type:
Differentiating Leukemoid reaction from Other Diseases
Leukemoid reaction is differentiated from leukemia by following ways[11][12]:
| Differentiating features | Leukemia | Leukemoid reaction |
|---|---|---|
| Causes | Carcinogens | Infectious agents, biologically active substances and
products of tissue destruction |
| Pathogenesis | The transformation of normal haematopoietic
cells to a tumor |
Activation of normal hematopoiesis and exit of immature leukocytes
into the bloodstream |
| Duration | Chronic | Temporary and reversible |
| Genetic level | Defect | No defect |
| Splenomegaly | Present | Not present |
| Peripheral blood | Immature cells, pancytopenia | Mature and immature granulocytes with left shift |
| Bone marrow | Increase in blasts and immature cells | Myeloid hyperplasia and normal morphology |
| LAP score | Low | High |
| Toxic granules (suggestive of infection) | Absent | Present |
| Dohle inclusion bodies | Absent | Present |
Leukemoid reaction should be differentiated from other causes of leucocytosis. The below table discusses different causes of leucocytosis:
| Category | Condition | Etiology | Mechanism | Congenital | Acquried | Clinical manifestations | Para−clinical findings | Gold standard | Associated findings | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demography | History | Symptoms | Signs | ||||||||||||||||||||||||||
| Lab Findings | |||||||||||||||||||||||||||||
| Physiologic | Increased bone marrow production | Demargination of peripheral blood neutrophils | Appearance | Fever | Abdominal pain | BP | Asplenia | Hepatosplenomegaly | Lymphadenopathy | Joint involvement | Other | CBC | PBS | Bone marrow exam | ESR/CRP | BUN/Cr | LFT | ||||||||||||
| Autonomous | Reactive | WBC | HB | Plt | |||||||||||||||||||||||||
| Hematologic | Hereditary neutrophilia[13] | − | + | − | − | + | − | Rare autosomal dominant genetic disorder |
|
Normal | − | − | Nl | − | + | − | − | − | ↑ | Nl | Nl |
|
Nl | Nl | Nl | Nl | Molecular testing |
| |
| Myeloproliferative neoplasms[14] |
|
− | + | − | − | + | + | Elderly | Exposure to | ± | + | Nl | − | + | − | − | ↑/↓ | ↓ | ↑/↓ |
|
|
↑ | Nl | Nl | Bone marrow examination + clinical manifestation |
| |||
| Polycythemia vera[15] |
|
− | + | − | − | + | − | Mean age >60 years old |
|
− | − | ↑ | − | + | + | − |
|
Nl to ↑ | ↑ | ↑ |
|
Nl | Nl | Nl | Bone marrow examination + clinical manifestation | ||||
| Microangiopathic hemolytic anemia (MAHA)[16] | − | + | − | − | + | + | Any |
|
+ | + | ↓ | − | + | − | − | ↑ | ↓ | ↑ |
|
NA | ↑ | ↑ | ↑ | Bone marrow examination + clinical manifestation |
| ||||
| Leukoerythroblastosis[17] |
|
− | + | − | − | − | + | Any | − | + | Nl | − | + | − | − | ↑ | ↓ | ↓ |
|
|
↑ | Nl | ↑ | Bone marrow biopsy |
| ||||
| Immunology/
Rheumatology |
Condition | Etiology | Physiologic | Autonomous increased bone marrow production | Reactive increased bone marrow production | Demargination of peripheral blood neutrophils | Congenital | Acquried | Demography | History | Appearance | Fever | Abdominal pain | BP | Asplenia | Hepatosplenomegaly | Lymphadenopathy | Joint involvement | Other signs | WBC | HB | Plt | PBS | Bone marrow exam | ESR/CRP | BUN/Cr | LFT | Gold standard | Associated findings |
| Leukocyte adhesion deficiency[18] |
|
− | + | − | − | + | − | Rare autosomal recessive, LAD II more in Middle East and Brazil |
|
|
+ | − | Nl | − | − | − | − |
|
↑ | ↓ | ↓/↑ |
|
|
Nl | Nl | Nl | Flow cytometry |
| |
| Cryopyrin-associated periodic syndromes[19] |
|
− | + | − | − | + | − | Autosomal dominant autoinflammatory syndrome |
|
+ | − | Nl | − | − | − | + | ↑ | ↓ | ↓/↑ |
|
|
↑ | Nl | ↑ | Genetic tests | ||||
| Rheumatoid arthritis[20][21] |
|
− | + | − | − | − | + | Any, more in young women, between 30-60 years old |
|
|
+ | − | Nl | − | − | − | + |
|
↑ | ↓ | ↑ |
|
NA | ↑ | Nl | Nl | Clinical manifestation + positive anti-CCP antibodies |
| |
| Juvenile onset rheumatoid arthritis[22] |
|
− | + | − | − | − | + | Children under the age of 16 |
|
|
+ | − | Nl | − | − | + | + | ↑ | ↓ | ↑ |
|
NA | ↑ | Nl | Nl | Clinical manifestation + laboratory findings |
| ||
| Adult Still's disease[23] |
|
− | + | − | − | − | + | Rare autoimmune disease | NA |
|
+ | − | Nl | − | − | + | + | ↑ | ↓ | ↑ |
|
NA | ↑ | Nl | Nl | Diagnosis of exclusion |
| ||
| Kawasaki disease[24] |
|
− | + | − | − | − | + | Autoimmune disease, more in Asian ethnicity boys | NA | + | + | Nl | − | − | + | + |
|
↑ | ↓ | ↑ |
|
NA | ↑ | Nl | Nl | Diagnostic criteria |
| ||
| IBD[25] | − | + | − | − | − | + | Autoimmune disease, more in young |
|
+ | + | Nl | − | + | + | + | ↑ | ↓ | ↑ |
|
NA | ↑ | Nl | Nl | Colonoscopy and biopsy | |||||
| Sarcoidosis[26] |
|
− | + | − | − | − | + | Autoimmune disease, more in young African American women |
|
+ | + | Nl | − | + | +
Bilateral hilar adenopathy |
+ | ↑ | ↓ | ↑ |
|
NA | ↑ | Nl | Nl | Diagnosis of exclusion |
| |||
| Chronic hepatitis[27] | − | + | − | − | − | + | Elderly |
|
+ | + | ↓ | − | + | + | + | ↑ | ↓ | ↑ |
|
NA | ↑ | ↑ | ↑ | Liver biopsy | |||||
| Sweet syndrome[28] |
|
− | + | − | − | − | + | Rare | + | + | Nl | − | − | + | + | ↑ | ↓ | ↑ |
|
|
↑ | Nl | Nl | Diagnostic criteria |
| ||||
| Acute gout[29] | − | + | − | − | − | + | Older males |
|
+ | − | − | − | − | + | ↑ | ↓ | ↑ |
|
NA | ↑ | ↑ | Nl | Clinical manifestation |
| |||||
| Medication | Condition | Etiology | Physiologic | Autonomous increased bone marrow production | Reactive increased bone marrow production | Demargination of peripheral blood neutrophils | Congenital | Acquried | Demography | History | Appearance | Fever | Abdominal pain | BP | Asplenia | Hepatosplenomegaly | Lymphadenopathy | Joint involvement | Other signs | WBC | HB | Plt | PBS | Bone marrow exam | ESR/CRP | BUN/Cr | LFT | Gold standard | Associated findings |
| Steroid[30] |
|
− | − | + | + | − | + | Any | − | + | Nl to ↓ | − | − | − | − | ↑ | Nl to ↓ | ↑ |
|
|
↑ | ↑ | Nl | Clinical manifestation + history of drug consumption |
| ||||
| Filgrastim (Myeloid growth factor)[31] |
|
− | − | + | + | − | + | Any | + | − | Nl to ↓ | − | − | − | + | ↑ | Nl to ↓ | ↑ | NA | NA | ↑ | Nl | Nl | Clinical manifestation + history of drug consumption |
| ||||
| Lithium[32] |
|
− | − | + | + | − | + | Any |
|
− | − | Nl | − | − | − | − |
|
↑ | Nl to ↓ | ↑ | NA | NA | Nl | ↑ | Nl | Clinical manifestation + history of drug consumption | |||
| Catecholamines |
|
− | − | + | + | − | + | Any |
|
− | − | Nl to ↓ | − | − | − | − | ↑ | ↑ | ↑ |
|
|
↑ | Nl | Nl | Clinical manifestation + history of drug consumption |
| |||
| ATRA[34] |
|
− | − | + | + | − | + | Any | − | − | Nl | − | − | − | − | ↑ | Nl | Nl | NA | NA | ↑ | Nl | ↑ | Clinical manifestation + history of drug consumption | |||||
| Other | Condition | Etiology | Physiologic | Autonomous increased bone marrow production | Reactive increased bone marrow production | Demargination of peripheral blood neutrophils | Congenital | Acquried | Demography | History | Appearance | Fever | Abdominal pain | BP | Asplenia | Hepatosplenomegaly | Lymphadenopathy | Joint involvement | Other signs | WBC | HB | Plt | PBS | Bone marrow exam | ESR/CRP | BUN/Cr | LFT | Gold standard | Associated findings |
| Infections[35] | − | + | + | + | − | + | Any |
|
|
+ | + | Nl to ↓ | − | ± | ± | ± | ↑ | ↓ | ↑ |
|
|
↑ | Nl | Nl | Clinical manifestation+ culture |
| |||
| Allergy[36] |
|
− | + | + | + | − | + | Any |
|
− | − | Nl to ↓ | − | − | − | − | ↑ | ↑ | ↑ |
|
|
↑ | Nl | Nl | Clinical manifestation | − | |||
| Post splenectomy[37] |
|
− | − | + | + | − | + | Any |
|
|
± | − | Nl | + | − | − | − | − | ↑ | ↓ | ↑ |
|
|
↑ | Nl | Nl | Clinical manifestation |
| |
| Cigarette smoking[38] |
|
− | − | + | + | − | + | Any | − | − | Nl | − | − | − | − | ↑ | ↑ | ↑ | NA | NA | Nl | Nl | Nl | Clinical manifestation | − | ||||
| Stress/exercise[39] |
|
+ | − | + | − | − | + | Athlete |
|
− | − | Nl | − | − | − | − | − | ↑ | ↑ | ↑ |
|
|
↑ | Nl | Nl | Clinical manifestation | − | ||
| Infancy[40] | Physiologic | + | − | − | − | − | + | Infancy | − |
|
− | − | Nl | − | − | − | − | − | ↑ | ↑ | ↑ | NA | NA | Nl | Nl | Nl | Clinical manifestation | − | |
| Pregnancy[41] | Physiologic | + | − | − | − | − | + | Pregnancy | − |
|
− | − | Nl | − | − | − | − | − | ↑ | ↓ | ↑ | NA | NA | Nl | Nl | Nl | Clinical manifestation | − | |
| Platelet clumping[42] | Spurious | − | − | − | − | − | + | Any | − |
|
− | − | Nl | − | − | − | − | − | ↑ | Nl | ↑ |
|
Nl | Nl | Nl | Nl | Clinical manifestation | − | |
| Mixed cryoglobulinemia[43] | Spurious | − | − | − | − | − | + | Any | − | − | Nl | − | − | − | + | ↑ | Nl to ↓ | ↑ |
|
Nl | Nl | Nl | Nl | Skin biopsy | |||||
| Category | Condition | Etiology | Physiologic | Autonomous increased bone marrow production | Reactive increased bone marrow production | Demargination of peripheral blood neutrophils | Congenital | Acquried | Demography | History | Appearance | Fever | Abdominal pain | BP | Asplenia | Hepatosplenomegaly | Lymphadenopathy | Joint involvement | Other signs | WBC | HB | Plt | PBS | Bone marrow exam | ESR/CRP | BUN/Cr | LFT | Gold standard | Associated findings |
Epidemiology and Demographics
Age
- Patients of all age groups may develop leukemoid reaction[1][44].
- Normal white blood cell count changes with age.
- Leukemoid reaction in neonates is more common, compared to children and adults.
Gender
- Leukemoid reaction affects men and women equally.
Race
- There is no racial predilection for the development of leukemoid reaction.
Risk Factors
- Common risk factors in the development of leukocytosis, include:[1]
Screening
No screening is done for leukemoid reaction.
Natural History, Complications, and Prognosis
History
The majority of patients with leukemoid reaction have the following complaints[45][46]
- Early clinical features, include:
Complications
- Common complications of leukemoid reaction, include:
Prognosis
- Prognosis generally depends on the underlying etiologies.
- If the white blood cell count reaches more than 50,000 per mm3, life threatening complications can occur.
Diagnosis
Symptoms
- Leukemoid reaction is usually symptomatic.
- Symptoms of leukemoid reaction are often unspecific, such as[47]:
- Obtain history of the following:
- Clinical features
- Duration (e.g. days, weeks, months)
- Remainder of complete blood count
Laboratory findings
- Laboratory findings consistent with the diagnosis of leukemoid reaction, include:[45]:
- White blood cell count above the normal range, greater than 25,000 per mm3.
- Bone marrow aspiration revealing hyperplasia of normal hematopoietic cells in proliferative reactions.
- Presence of blast and immature forms of leukocyte, platelet and erythrocytes in the proliferative reactions.
- Peripheral blood smear showing myelocytes, metamyelocytes, promyelocytes, and few myeloblasts.
- Leukocyte alkaline phosphatase score more than 100.
Electrocardiogram
No specific ECG changes in leukemoid reaction.
X-Ray
No specific x ray changes in leukemoid reaction.
Echocardiography and Ultrasound
No echocardiography and ultrasound findings.
CT
No CT scan findings in leukemoid reaction.
MRI
No specific MRI findings in leukemoid reaction.
Treatment
Medical Therapy
- The treatment of leukemoid reaction depends on the underlying cause.[45]
- Measures to reduce white blood cell count include:
- Leukapheresis or exchange blood transfusion.
- Hydration
- Urine alkalinization
- Administration of allopurinol or rasburicase to reduce serum uric acid and minimize tumor lysis syndrome.
Surgery
The treatment depends on the underlying cause. In general, there is no role for surgery.
Primary prevention
Prevention and treatment of infections.
Secondary prevention
Treatment of underlying cause and reduction of white blood cell count.
See also
References
- ↑ 1.0 1.1 1.2 1.3 Abramson N, Melton B (2000). "Leukocytosis: basics of clinical assessment". Am Fam Physician. 62 (9): 2053–60. PMID 11087187.
- ↑ Ward HN, Reinhard EH (1971). "Chronic idiopathic leukocytosis". Ann Intern Med. 75 (2): 193–8. PMID 5558646.
- ↑ Leukocytosis. Wikipedia. https://en.wikipedia.org/wiki/Leukocytosis Accessed on May 23, 2016
- ↑ Wanahita A, Goldsmith EA, Musher DM (2002). "Conditions associated with leukocytosis in a tertiary care hospital, with particular attention to the role of infection caused by clostridium difficile". Clin Infect Dis. 34 (12): 1585–92. doi:10.1086/340536. PMID 12032893.
- ↑ Lawrence YR, Raveh D, Rudensky B, Munter G (2007). "Extreme leukocytosis in the emergency department". QJM. 100 (4): 217–23. doi:10.1093/qjmed/hcm006. PMID 17314214.
- ↑ McBride JA, Dacie JV, Shapley R (1968). "The effect of splenectomy on the leucocyte count". Br J Haematol. 14 (2): 225–31. PMID 5635603.
- ↑ Spencer RP, McPhedran P, Finch SC, Morgan WS (1972). "Persistent neutrophilic leukocytosis associated with idiopathic functional asplenia". J Nucl Med. 13 (3): 224–6. PMID 5058244.
- ↑ Foster NK, Martyn JB, Rangno RE, Hogg JC, Pardy RL (1986). "Leukocytosis of exercise: role of cardiac output and catecholamines". J Appl Physiol (1985). 61 (6): 2218–23. doi:10.1152/jappl.1986.61.6.2218. PMID 3804928.
- ↑ Brodeur GM, Dahl GV, Williams DL, Tipton RE, Kalwinsky DK (1980). "Transient leukemoid reaction and trisomy 21 mosaicism in a phenotypically normal newborn". Blood. 55 (4): 691–3. PMID 6444534.
- ↑ Harvey Y, Bleakley S, Blombery P, Bain BJ (2018). "Marked leukemoid reaction in a patient with metastatic breast carcinoma". Am J Hematol. 93 (2): 306–307. doi:10.1002/ajh.24849. PMID 28699170.
- ↑ Sakka V, Tsiodras S, Giamarellos-Bourboulis EJ, Giamarellou H (2006). "An update on the etiology and diagnostic evaluation of a leukemoid reaction". Eur J Intern Med. 17 (6): 394–8. doi:10.1016/j.ejim.2006.04.004. PMID 16962944.
- ↑ Updyke KM, Morales-Lappot J, Lee T (2017). "Atypical Presentation of Chronic Myelogenous Leukemia". Cureus. 9 (5): e1280. doi:10.7759/cureus.1280. PMC 5484601. PMID 28656128.
- ↑ Herring, William Benjamin; Smith, Laurin Gresham; Walker, Richard Isley; Herion, John Carroll (1974). "Hereditary neutrophilia". The American Journal of Medicine. 56 (5): 729–734. doi:10.1016/0002-9343(74)90642-1. ISSN 0002-9343.
- ↑ Tefferi A (February 2010). "Leukocytosis as a risk factor for thrombosis in myeloproliferative neoplasms-biologically plausible but clinically uncertain". Am. J. Hematol. 85 (2): 93–4. doi:10.1002/ajh.21614. PMID 20052751.
- ↑ Boiocchi L, Gianelli U, Iurlo A, Fend F, Bonzheim I, Cattaneo D, Knowles DM, Orazi A (November 2015). "Neutrophilic leukocytosis in advanced stage polycythemia vera: hematopathologic features and prognostic implications". Mod. Pathol. 28 (11): 1448–57. doi:10.1038/modpathol.2015.100. PMID 26336886.
- ↑ Morton JM, George JN (June 2016). "Microangiopathic Hemolytic Anemia and Thrombocytopenia in Patients With Cancer". J Oncol Pract. 12 (6): 523–30. doi:10.1200/JOP.2016.012096. PMID 27288467.
- ↑ Canbolat Ayhan A, Timur C, Ayhan Y, Kes G (June 2014). "Leukoerythroblastosis Mimicking Leukemia: A case report". Iran J Pediatr. 24 (3): 332–3. PMC 4276592. PMID 25562031.
- ↑ Levy-Mendelovich S, Rechavi E, Abuzaitoun O, Vernitsky H, Simon AJ, Lev A, Somech R (April 2016). "Highlighting the problematic reliance on CD18 for diagnosing leukocyte adhesion deficiency type 1". Immunol. Res. 64 (2): 476–82. doi:10.1007/s12026-015-8706-5. PMID 26434744.
- ↑ Labrousse M, Kevorkian-Verguet C, Boursier G, Rowczenio D, Maurier F, Lazaro E, Aggarwal M, Lemelle I, Mura T, Belot A, Touitou I, Sarrabay G (September 2018). "Mosaicism in autoinflammatory diseases: Cryopyrin-associated periodic syndromes (CAPS) and beyond. A systematic review". Crit Rev Clin Lab Sci. 55 (6): 432–442. doi:10.1080/10408363.2018.1488805. PMID 30035647.
- ↑ Scott DL, Wolfe F, Huizinga TW (September 2010). "Rheumatoid arthritis". Lancet. 376 (9746): 1094–108. doi:10.1016/S0140-6736(10)60826-4. PMID 20870100.
- ↑ Glant TT, Mikecz K, Rauch TA (February 2014). "Epigenetics in the pathogenesis of rheumatoid arthritis". BMC Med. 12: 35. doi:10.1186/1741-7015-12-35. PMC 3936819. PMID 24568138.
- ↑ Naz S, Mushtaq A, Rehman S, Bari A, Maqsud A, Khan MZ, Ahmad TM (June 2013). "Juvenile rheumatoid arthritis". J Coll Physicians Surg Pak. 23 (6): 409–12. doi:06.2013/JCPSP.409412 Check
|doi=value (help). PMID 23763801. - ↑ Kadavath S, Efthimiou P (February 2015). "Adult-onset Still's disease-pathogenesis, clinical manifestations, and new treatment options". Ann. Med. 47 (1): 6–14. doi:10.3109/07853890.2014.971052. PMID 25613167.
- ↑ Sundel RP (2015). "Kawasaki disease". Rheum. Dis. Clin. North Am. 41 (1): 63–73, viii. doi:10.1016/j.rdc.2014.09.010. PMID 25399940.
- ↑ Zhang YZ, Li YY (January 2014). "Inflammatory bowel disease: pathogenesis". World J. Gastroenterol. 20 (1): 91–9. doi:10.3748/wjg.v20.i1.91. PMC 3886036. PMID 24415861.
- ↑ Modaresi Esfeh J, Culver D, Plesec T, John B (March 2015). "Clinical presentation and protocol for management of hepatic sarcoidosis". Expert Rev Gastroenterol Hepatol. 9 (3): 349–58. doi:10.1586/17474124.2015.958468. PMID 25473783.
- ↑ Gish RG, Given BD, Lai CL, Locarnini SA, Lau JY, Lewis DL, Schluep T (September 2015). "Chronic hepatitis B: Virology, natural history, current management and a glimpse at future opportunities". Antiviral Res. 121: 47–58. doi:10.1016/j.antiviral.2015.06.008. PMID 26092643.
- ↑ Das A, Burmeister R, Chhaya R, Eisenga B, Kumar A (September 2018). "Sweet Syndrome in a Patient With Systemic Lupus Erythematosus". J Clin Rheumatol. doi:10.1097/RHU.0000000000000904. PMID 30247226.
- ↑ Dalbeth N, Zhong CS, Grainger R, Khanna D, Khanna PP, Singh JA, McQueen FM, Taylor WJ (March 2014). "Outcome measures in acute gout: a systematic literature review". J. Rheumatol. 41 (3): 558–68. doi:10.3899/jrheum.131244. PMC 4217650. PMID 24334652.
- ↑ Shoenfeld Y, Gurewich Y, Gallant LA, Pinkhas J (November 1981). "Prednisone-induced leukocytosis. Influence of dosage, method and duration of administration on the degree of leukocytosis". Am. J. Med. 71 (5): 773–8. PMID 7304648.
- ↑ Crawford J, Armitage J, Balducci L, Becker PS, Blayney DW, Cataland SR, Heaney ML, Hudock S, Kloth DD, Kuter DJ, Lyman GH, McMahon B, Rugo HS, Saad AA, Schwartzberg LS, Shayani S, Steensma DP, Talbott M, Vadhan-Raj S, Westervelt P, Westmoreland M, Dwyer M, Ho M (October 2013). "Myeloid growth factors". J Natl Compr Canc Netw. 11 (10): 1266–90. PMID 24142827.
- ↑ Aiff H, Attman PO, Aurell M, Bendz H, Ramsauer B, Schön S, Svedlund J (May 2015). "Effects of 10 to 30 years of lithium treatment on kidney function". J. Psychopharmacol. (Oxford). 29 (5): 608–14. doi:10.1177/0269881115573808. PMID 25735990.
- ↑ Bedoui S, Lechner S, Gebhardt T, Nave H, Beck-Sickinger AG, Straub RH, Pabst R, von Hörsten S (November 2002). "NPY modulates epinephrine-induced leukocytosis via Y-1 and Y-5 receptor activation in vivo: sympathetic co-transmission during leukocyte mobilization". J. Neuroimmunol. 132 (1–2): 25–33. PMID 12417430.
- ↑ Bi KH, Jiang GS (December 2006). "Relationship between cytokines and leukocytosis in patients with APL induced by all-trans retinoic acid or arsenic trioxide". Cell. Mol. Immunol. 3 (6): 421–7. PMID 17257495.
- ↑ Horasan ES, Dağ A, Ersoz G, Kaya A (October 2013). "Surgical site infections and mortality in elderly patients". Med Mal Infect. 43 (10): 417–22. doi:10.1016/j.medmal.2013.07.009. PMID 24012414.
- ↑ Davis M, van der Hilst J (2018). "Mimickers of Urticaria: Urticarial Vasculitis and Autoinflammatory Diseases". J Allergy Clin Immunol Pract. 6 (4): 1162–1170. doi:10.1016/j.jaip.2018.05.006. PMID 29871797. Vancouver style error: initials (help)
- ↑ Bilello JF, Sharp VL, Dirks RC, Kaups KL, Davis JW (2018). "After the embo: predicting non-hemorrhagic indications for splenectomy after angioembolization in patients with blunt trauma". Trauma Surg Acute Care Open. 3 (1): e000159. doi:10.1136/tsaco-2017-000159. PMC 5887792. PMID 29766137.
- ↑ Lymperaki E, Makedou K, Iliadis S, Vagdatli E (2015). "Effects of acute cigarette smoking on total blood count and markers of oxidative stress in active and passive smokers". Hippokratia. 19 (4): 293–7. PMC 5033137. PMID 27688691.
- ↑ Simpson RJ, Kunz H, Agha N, Graff R (2015). "Exercise and the Regulation of Immune Functions". Prog Mol Biol Transl Sci. 135: 355–80. doi:10.1016/bs.pmbts.2015.08.001. PMID 26477922.
- ↑ Nouatin O, Gbédandé K, Ibitokou S, Vianou B, Houngbegnon P, Ezinmegnon S, Borgella S, Akplogan C, Cottrell G, Varani S, Massougbodji A, Moutairou K, Troye-Blomberg M, Deloron P, Luty AJ, Fievet N (2015). "Infants' Peripheral Blood Lymphocyte Composition Reflects Both Maternal and Post-Natal Infection with Plasmodium falciparum". PLoS ONE. 10 (11): e0139606. doi:10.1371/journal.pone.0139606. PMC 4651557. PMID 26580401.
- ↑ Perseghin P (December 2015). "Erythrocyte exchange and leukapheresis in pregnancy". Transfus. Apher. Sci. 53 (3): 279–82. doi:10.1016/j.transci.2015.11.007. PMID 26621538.
- ↑ Castrillo A, Álvarez I, Tolksdorf F (April 2015). "In vitro evaluation of platelet concentrates suspended in additive solution and treated for pathogen reduction: effects of clumping formation". Blood Transfus. 13 (2): 281–6. doi:10.2450/2014.0162-14. PMC 4385077. PMID 25369589.
- ↑ Cacoub P, Comarmond C, Domont F, Savey L, Saadoun D (September 2015). "Cryoglobulinemia Vasculitis". Am. J. Med. 128 (9): 950–5. doi:10.1016/j.amjmed.2015.02.017. PMID 25837517.
- ↑ Hoofien A, Yarden-Bilavski H, Ashkenazi S, Chodick G, Livni G (2018). "Leukemoid reaction in the pediatric population: etiologies, outcome, and implications". Eur J Pediatr. 177 (7): 1029–1036. doi:10.1007/s00431-018-3155-5. PMID 29696475.
- ↑ 45.0 45.1 45.2 Ellison TA, Mandal K (2018). "Leukemoid reaction: Case report". J Thorac Cardiovasc Surg. 155 (4): e117–e118. doi:10.1016/j.jtcvs.2017.08.125. PMID 29366572.
- ↑ Wang Z, Cai Q, Li G, Jiang N, Niu Y (2017). "Giant Pheochromocytoma With Leukemoid Reaction: A Case Report". Urology. 99: e17–e19. doi:10.1016/j.urology.2016.08.021. PMID 27720771.
- ↑ Agrawal D, Kurwale N, Sharma BS (2016). "Leukocytosis after routine cranial surgery: A potential marker for brain damage in intracranial surgery". Asian J Neurosurg. 11 (2): 109–13. doi:10.4103/1793-5482.145066. PMC 4802930. PMID 27057215.