Intravascular large B-cell lymphoma: Difference between revisions
| (56 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
{{ | {{SI}} | ||
{{CMG}}; {{AE}} {{AS}}{{sali}} | |||
}} | |||
{{ | |||
{{SK}} Intravascular lymphomatosis, angiotropic large cell lymphoma, angio-endotheliotropic (intravascular) lymphoma, angioendotheliomatosis proliferans systematisata, malignant angioendotheliomatosis | |||
==[[Intravascular large B-cell lymphoma | == Overview == | ||
[[Intravascular large B-cell lymphoma]] is a very rare subtype of [[diffuse large B-cell lymphoma]] (DLBCL). It is also considered a distinct type of [[non-Hodgkin lymphoma]] (NHL) in the World Health Organization ([[WHO]]) classification system. Intravascular large B-cell lymphoma affects small blood vessels. It is a rare and aggressive variant of intravascular proliferation of clonal [[lymphocytes]] with little to no [[parenchymal]] involvement. Based on the clinical presentation, intravascular large B-cell lymphoma may be classified into either Western variant or Asian variant. On [[microscopic]] [[histopathological]] analysis, [[diffuse]] infiltrate of large atypical cells with irregular nuclear contours, vesicular chromatin, and occasional prominent [[nucleoli]] are characteristic findings of intravascular large b-cell lymphoma. The incidence of intravascular [[large B-cell lymphoma]] increases with age; the median age at diagnosis is 67 years. Intravascular large B-cell [[lymphoma]] affects men and women equally. People with this type of [[lymphoma]] often have a poor prognosis. Symptoms of the intravascular large B-cell lymphoma include [[fever]], [[weight loss]], [[night sweats]], chest pain, abdominal pain, bone pain, and painless swellings in the neck, axilla, groin, thorax, and abdomen. [[Lymph node]] biopsy is diagnostic of intravascular large B-cell lymphoma. [[CT]], [[MRI]], and [[PET]] scan may be helpful in the diagnosis of intravascular large B-cell lymphoma. The predominant therapy for intravascular large B-cell lymphoma is [[chemotherapy]]. Adjunctive [[radiotherapy]] may be required. | |||
== | ==Classification== | ||
Based on the clinical presentation, intravascular large B-cell lymphoma may be classified into either Western variant or Asian variant. | |||
{| style="border: 0px; font-size: 90%; margin: 3px;" align=center | |||
|+ '''Intravascular large B-cell lymphoma classification''' | |||
! style="background: #4479BA;; color:#FFF;" | Name | |||
! style="background: #4479BA;; color:#FFF;" | Description | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Western variant | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* Western variant characterized by symptoms related to the main organ involved, predominantly neurological or cutaneous | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Asian variant | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* Asian variant in which the patients present with multi-organ failure, [[hepatosplenomegaly]], [[pancytopenia]], and hemophagocytic syndrome. | |||
* This is an aggressive lymphoma which responds poorly to [[chemotherapy]]. | |||
* The poor prognosis reflects in part frequent delays in diagnosis because of a lack of detectable tumor masses. | |||
|} | |||
==[[Intravascular large B-cell lymphoma pathophysiology| | == Pathophysiology== | ||
Intravascular large B-cell lymphoma is characterized by a massive intravascular proliferation of atypical mononuclear cells which lodged in the lumina of small or intermediate vessels in many organs. The neoplastic lymphoid cells are large with prominent [[nucleoli]] and frequent mitotic figures. Fibrin [[thrombi]], [[haemorrhage]] and [[necrosis]] may be seen<ref name="pmid28461685">{{cite journal |vauthors=di Fonzo H, Contardo D, Carrozza D, Finocchietto P, Rojano Crisson A, Cabral C, de Los Angeles Juarez M |title=Intravascular Large B Cell Lymphoma Presenting as Fever of Unknown Origin and Diagnosed by Random Skin Biopsies: A Case Report and Literature Review |journal=Am J Case Rep |volume=18 |issue= |pages=482–486 |date=May 2017 |pmid=28461685 |pmc=5421743 |doi=10.12659/ajcr.903816 |url=}}</ref>. | |||
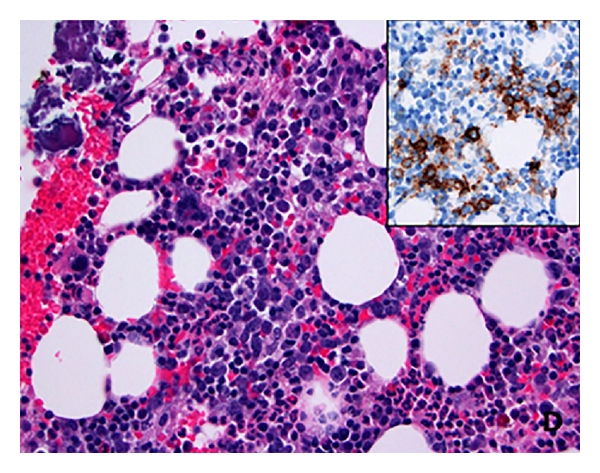
===Microscopic Pathology=== | |||
On microscopic [[histopathological]] analysis, diffuse infiltrate of large atypical cells with irregular nuclear contours, vesicular chromatin, and occasional prominent nucleoli are characteristic findings of intravascular large b-cell lymphoma. | |||
[[File:Intravascular lymphoma - very high mag.jpg|left|thumb|Micrograph showing an intravascular large B-cell lymphoma in a blood vessel of the brain. H&E stain.]] | |||
[[File:Intravascular large B-cell lymphoma pathophysiology image 4.jpg|center|thumb|Micrograph showing an intravascular large B-cell lymphoma.]] | |||
== | ==Causes== | ||
There are no established causes for intravascular large B-cell lymphoma. | |||
== | ==Differentiating Intravascular Large B-Cell Lymphoma from other Diseases== | ||
Intravascular large B-cell lymphoma must be differentiated from other lymphomas with the help of clincal, morphological, immunophenotypic and genetic data as the treatment of all these conditions are different from each other.<ref name="pmid18094718">{{cite journal |vauthors=Matutes E, Oscier D, Montalban C, Berger F, Callet-Bauchu E, Dogan A, Felman P, Franco V, Iannitto E, Mollejo M, Papadaki T, Remstein ED, Salar A, Solé F, Stamatopoulos K, Thieblemont C, Traverse-Glehen A, Wotherspoon A, Coiffier B, Piris MA |title=Splenic marginal zone lymphoma proposals for a revision of diagnostic, staging and therapeutic criteria |journal=Leukemia |volume=22 |issue=3 |pages=487–95 |date=March 2008 |pmid=18094718 |doi=10.1038/sj.leu.2405068 |url=}}</ref><ref name="pmid20479288">{{cite journal |vauthors=Salido M, Baró C, Oscier D, Stamatopoulos K, Dierlamm J, Matutes E, Traverse-Glehen A, Berger F, Felman P, Thieblemont C, Gesk S, Athanasiadou A, Davis Z, Gardiner A, Milla F, Ferrer A, Mollejo M, Calasanz MJ, Florensa L, Espinet B, Luño E, Wlodarska I, Verhoef G, García-Granero M, Salar A, Papadaki T, Serrano S, Piris MA, Solé F |title=Cytogenetic aberrations and their prognostic value in a series of 330 splenic marginal zone B-cell lymphomas: a multicenter study of the Splenic B-Cell Lymphoma Group |journal=Blood |volume=116 |issue=9 |pages=1479–88 |date=September 2010 |pmid=20479288 |doi=10.1182/blood-2010-02-267476 |url=}}</ref><ref name="pmid22891276">{{cite journal |vauthors=Kiel MJ, Velusamy T, Betz BL, Zhao L, Weigelin HG, Chiang MY, Huebner-Chan DR, Bailey NG, Yang DT, Bhagat G, Miranda RN, Bahler DW, Medeiros LJ, Lim MS, Elenitoba-Johnson KS |title=Whole-genome sequencing identifies recurrent somatic NOTCH2 mutations in splenic marginal zone lymphoma |journal=J. Exp. Med. |volume=209 |issue=9 |pages=1553–65 |date=August 2012 |pmid=22891276 |pmc=3428949 |doi=10.1084/jem.20120910 |url=}}</ref><ref name="pmid22891273">{{cite journal |vauthors=Rossi D, Trifonov V, Fangazio M, Bruscaggin A, Rasi S, Spina V, Monti S, Vaisitti T, Arruga F, Famà R, Ciardullo C, Greco M, Cresta S, Piranda D, Holmes A, Fabbri G, Messina M, Rinaldi A, Wang J, Agostinelli C, Piccaluga PP, Lucioni M, Tabbò F, Serra R, Franceschetti S, Deambrogi C, Daniele G, Gattei V, Marasca R, Facchetti F, Arcaini L, Inghirami G, Bertoni F, Pileri SA, Deaglio S, Foà R, Dalla-Favera R, Pasqualucci L, Rabadan R, Gaidano G |title=The coding genome of splenic marginal zone lymphoma: activation of NOTCH2 and other pathways regulating marginal zone development |journal=J. Exp. Med. |volume=209 |issue=9 |pages=1537–51 |date=August 2012 |pmid=22891273 |pmc=3428941 |doi=10.1084/jem.20120904 |url=}}</ref><ref name="pmid21663470">{{cite journal |vauthors=Tiacci E, Trifonov V, Schiavoni G, Holmes A, Kern W, Martelli MP, Pucciarini A, Bigerna B, Pacini R, Wells VA, Sportoletti P, Pettirossi V, Mannucci R, Elliott O, Liso A, Ambrosetti A, Pulsoni A, Forconi F, Trentin L, Semenzato G, Inghirami G, Capponi M, Di Raimondo F, Patti C, Arcaini L, Musto P, Pileri S, Haferlach C, Schnittger S, Pizzolo G, Foà R, Farinelli L, Haferlach T, Pasqualucci L, Rabadan R, Falini B |title=BRAF mutations in hairy-cell leukemia |journal=N. Engl. J. Med. |volume=364 |issue=24 |pages=2305–15 |date=June 2011 |pmid=21663470 |doi=10.1056/NEJMoa1014209 |url=}}</ref><ref name="pmid24241536">{{cite journal |vauthors=Waterfall JJ, Arons E, Walker RL, Pineda M, Roth L, Killian JK, Abaan OD, Davis SR, Kreitman RJ, Meltzer PS |title=High prevalence of MAP2K1 mutations in variant and IGHV4-34-expressing hairy-cell leukemias |journal=Nat. Genet. |volume=46 |issue=1 |pages=8–10 |date=January 2014 |pmid=24241536 |pmc=3905739 |doi=10.1038/ng.2828 |url=}}</ref><ref name="pmid18042795">{{cite journal |vauthors=Traverse-Glehen A, Baseggio L, Bauchu EC, Morel D, Gazzo S, Ffrench M, Verney A, Rolland D, Thieblemont C, Magaud JP, Salles G, Coiffier B, Berger F, Felman P |title=Splenic red pulp lymphoma with numerous basophilic villous lymphocytes: a distinct clinicopathologic and molecular entity? |journal=Blood |volume=111 |issue=4 |pages=2253–60 |date=February 2008 |pmid=18042795 |doi=10.1182/blood-2007-07-098848 |url=}}</ref><ref name="pmid22301699">{{cite journal |vauthors=Braggio E, Dogan A, Keats JJ, Chng WJ, Huang G, Matthews JM, Maurer MJ, Law ME, Bosler DS, Barrett M, Lossos IS, Witzig TE, Fonseca R |title=Genomic analysis of marginal zone and lymphoplasmacytic lymphomas identified common and disease-specific abnormalities |journal=Mod. Pathol. |volume=25 |issue=5 |pages=651–60 |date=May 2012 |pmid=22301699 |pmc=3341516 |doi=10.1038/modpathol.2011.213 |url=}}</ref><ref name="pmid23611359">{{cite journal |vauthors=Traverse-Glehen A, Bachy E, Baseggio L, Callet-Bauchu E, Gazzo S, Verney A, Hayette S, Jallades L, Ffrench M, Salles G, Coiffier B, Felman P, Berger F |title=Immunoarchitectural patterns in splenic marginal zone lymphoma: correlations with chromosomal aberrations, IGHV mutations, and survival. A study of 76 cases |journal=Histopathology |volume=62 |issue=6 |pages=876–93 |date=May 2013 |pmid=23611359 |doi=10.1111/his.12092 |url=}}</ref><ref name="pmid22210875">{{cite journal |vauthors=Xi L, Arons E, Navarro W, Calvo KR, Stetler-Stevenson M, Raffeld M, Kreitman RJ |title=Both variant and IGHV4-34-expressing hairy cell leukemia lack the BRAF V600E mutation |journal=Blood |volume=119 |issue=14 |pages=3330–2 |date=April 2012 |pmid=22210875 |pmc=3321859 |doi=10.1182/blood-2011-09-379339 |url=}}</ref><ref name="pmid8123845">{{cite journal |vauthors=Matutes E, Morilla R, Owusu-Ankomah K, Houlihan A, Catovsky D |title=The immunophenotype of splenic lymphoma with villous lymphocytes and its relevance to the differential diagnosis with other B-cell disorders |journal=Blood |volume=83 |issue=6 |pages=1558–62 |date=March 1994 |pmid=8123845 |doi= |url=}}</ref><ref name="pmid21917686">{{cite journal |vauthors=Venkataraman G, Aguhar C, Kreitman RJ, Yuan CM, Stetler-Stevenson M |title=Characteristic CD103 and CD123 expression pattern defines hairy cell leukemia: usefulness of CD123 and CD103 in the diagnosis of mature B-cell lymphoproliferative disorders |journal=Am. J. Clin. Pathol. |volume=136 |issue=4 |pages=625–30 |date=October 2011 |pmid=21917686 |doi=10.1309/AJCPKUM9J4IXCWEU |url=}}</ref><ref name="pmid23073320">{{cite journal |vauthors=Ponzoni M, Kanellis G, Pouliou E, Baliakas P, Scarfò L, Ferreri AJ, Doglioni C, Bikos V, Dagklis A, Anagnostopoulos A, Ghia P, Stamatopoulos K, Papadaki T |title=Bone marrow histopathology in the diagnostic evaluation of splenic marginal-zone and splenic diffuse red pulp small B-cell lymphoma: a reliable substitute for spleen histopathology? |journal=Am. J. Surg. Pathol. |volume=36 |issue=11 |pages=1609–18 |date=November 2012 |pmid=23073320 |doi=10.1097/PAS.0b013e318271243d |url=}}</ref><ref name="pmid15183626">{{cite journal |vauthors=Falini B, Tiacci E, Liso A, Basso K, Sabattini E, Pacini R, Foa R, Pulsoni A, Dalla Favera R, Pileri S |title=Simple diagnostic assay for hairy cell leukaemia by immunocytochemical detection of annexin A1 (ANXA1) |journal=Lancet |volume=363 |issue=9424 |pages=1869–70 |date=June 2004 |pmid=15183626 |doi=10.1016/S0140-6736(04)16356-3 |url=}}</ref><ref name="pmid20220064">{{cite journal |vauthors=Kanellis G, Mollejo M, Montes-Moreno S, Rodriguez-Pinilla SM, Cigudosa JC, Algara P, Montalban C, Matutes E, Wotherspoon A, Piris MA |title=Splenic diffuse red pulp small B-cell lymphoma: revision of a series of cases reveals characteristic clinico-pathological features |journal=Haematologica |volume=95 |issue=7 |pages=1122–9 |date=July 2010 |pmid=20220064 |doi=10.3324/haematol.2009.013714 |url=}}</ref><ref name="pmid24366360">{{cite journal |vauthors=Hunter ZR, Xu L, Yang G, Zhou Y, Liu X, Cao Y, Manning RJ, Tripsas C, Patterson CJ, Sheehy P, Treon SP |title=The genomic landscape of Waldenstrom macroglobulinemia is characterized by highly recurring MYD88 and WHIM-like CXCR4 mutations, and small somatic deletions associated with B-cell lymphomagenesis |journal=Blood |volume=123 |issue=11 |pages=1637–46 |date=March 2014 |pmid=24366360 |doi=10.1182/blood-2013-09-525808 |url=}}</ref><ref name="pmid15767800">{{cite journal |vauthors=Went PT, Zimpfer A, Pehrs AC, Sabattini E, Pileri SA, Maurer R, Terracciano L, Tzankov A, Sauter G, Dirnhofer S |title=High specificity of combined TRAP and DBA.44 expression for hairy cell leukemia |journal=Am. J. Surg. Pathol. |volume=29 |issue=4 |pages=474–8 |date=April 2005 |pmid=15767800 |doi= |url=}}</ref><ref name="pmid19287458">{{cite journal |vauthors=Morice WG, Chen D, Kurtin PJ, Hanson CA, McPhail ED |title=Novel immunophenotypic features of marrow lymphoplasmacytic lymphoma and correlation with Waldenström's macroglobulinemia |journal=Mod. Pathol. |volume=22 |issue=6 |pages=807–16 |date=June 2009 |pmid=19287458 |doi=10.1038/modpathol.2009.34 |url=}}</ref><ref name="pmid25268192">{{cite journal |vauthors=Behdad A, Bailey NG |title=Diagnosis of splenic B-cell lymphomas in the bone marrow: a review of histopathologic, immunophenotypic, and genetic findings |journal=Arch. Pathol. Lab. Med. |volume=138 |issue=10 |pages=1295–301 |date=October 2014 |pmid=25268192 |doi=10.5858/arpa.2014-0291-CC |url=}}</ref><ref name="pmid23347903">{{cite journal |vauthors=Shao H, Calvo KR, Grönborg M, Tembhare PR, Kreitman RJ, Stetler-Stevenson M, Yuan CM |title=Distinguishing hairy cell leukemia variant from hairy cell leukemia: development and validation of diagnostic criteria |journal=Leuk. Res. |volume=37 |issue=4 |pages=401–409 |date=April 2013 |pmid=23347903 |pmc=5575750 |doi=10.1016/j.leukres.2012.11.021 |url=}}</ref><ref name="pmid25114404">{{cite journal |vauthors=Konkay K, Uppin MS, Uppin SG, Raghunadha Rao D, Geetha Ch, Paul TR |title=Hairy cell leukemia: clinicopathological and immunophenotypic study |journal=Indian J Hematol Blood Transfus |volume=30 |issue=3 |pages=180–6 |date=September 2014 |pmid=25114404 |pmc=4115087 |doi=10.1007/s12288-013-0231-x |url=}}</ref><ref name="pmid25818826">{{cite journal |vauthors=Rudolf-Oliveira RC, Pirolli MM, de Souza FS, Michels J, Santos-Silva MC |title=Hairy cell leukemia variant: the importance of differential diagnosis |journal=Rev Bras Hematol Hemoter |volume=37 |issue=2 |pages=132–5 |date=2015 |pmid=25818826 |pmc=4382572 |doi=10.1016/j.bjhh.2015.01.003 |url=}}</ref><ref name="pmid19880776">{{cite journal |vauthors=Pileri SA, Falini B |title=Mantle cell lymphoma |journal=Haematologica |volume=94 |issue=11 |pages=1488–92 |date=November 2009 |pmid=19880776 |pmc=2770958 |doi=10.3324/haematol.2009.013359 |url=}}</ref><ref name="pmid22541613">{{cite journal |vauthors=Traverse-Glehen A, Baseggio L, Salles G, Coiffier B, Felman P, Berger F |title=Splenic diffuse red pulp small-B cell lymphoma: toward the emergence of a new lymphoma entity |journal=Discov Med |volume=13 |issue=71 |pages=253–65 |date=April 2012 |pmid=22541613 |doi= |url=}}</ref><ref name="pmid22499304">{{cite journal |vauthors=Rahman K, Subramanian PG, Kadam PA, Gadage V, Galani K, Mittal N, Ghogale S, Badrinath Y, Ansari R, Kushte S, Nair R, Sengar M, Menon H, Gujral S |title=Morphological spectrum of leukemic mantle cell lymphoma |journal=Indian J Pathol Microbiol |volume=55 |issue=1 |pages=66–71 |date=2012 |pmid=22499304 |doi=10.4103/0377-4929.94860 |url=}}</ref><ref name="pmid15762289">{{cite journal |vauthors=Cessna MH, Hartung L, Tripp S, Perkins SL, Bahler DW |title=Hairy cell leukemia variant: fact or fiction |journal=Am. J. Clin. Pathol. |volume=123 |issue=1 |pages=132–8 |date=January 2005 |pmid=15762289 |doi= |url=}}</ref><ref name="pmid25818826">{{cite journal |vauthors=Rudolf-Oliveira RC, Pirolli MM, de Souza FS, Michels J, Santos-Silva MC |title=Hairy cell leukemia variant: the importance of differential diagnosis |journal=Rev Bras Hematol Hemoter |volume=37 |issue=2 |pages=132–5 |date=2015 |pmid=25818826 |pmc=4382572 |doi=10.1016/j.bjhh.2015.01.003 |url=}}</ref><ref name="pmid11789727">{{cite journal |vauthors=Kansal R, Singleton TP, Ross CW, Finn WG, Padmore RF, Schnitzer B |title=Follicular hodgkin lymphoma: a histopathologic study |journal=Am. J. Clin. Pathol. |volume=117 |issue=1 |pages=29–35 |date=January 2002 |pmid=11789727 |doi=10.1309/M7YV-V8V2-A5VA-J1Y4 |url=}}</ref><ref name="pmid29748447">{{cite journal |vauthors=Autore F, Strati P, Laurenti L, Ferrajoli A |title=Morphological, immunophenotypic, and genetic features of chronic lymphocytic leukemia with trisomy 12: a comprehensive review |journal=Haematologica |volume=103 |issue=6 |pages=931–938 |date=June 2018 |pmid=29748447 |pmc=6058775 |doi=10.3324/haematol.2017.186684 |url=}}</ref> | |||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 1000px" | |||
| valign="top" | | |||
|+ | |||
! style="background: #4479BA; width: 600px;" | {{fontcolor|#FFF|'''Differential Diagnosis'''}} | |||
! style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF|'''Cytogenetics'''}} | |||
! style="background: #4479BA; width: 500px;" | {{fontcolor|#FFF|'''Morphological Features'''}} | |||
! style="background: #4479BA; width: 500px;" | {{fontcolor|#FFF|'''Immunophenotype'''}} | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | |||
'''Splenic marginal zone lymphoma''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Deletion 7q, [[trisomy]] 3, [[trisomy]] 12, [[trisomy]] 18, | |||
* Genes mutation [[NOTCH2]], NFkB pathway genes (BIRC3, [[TNFAIP3]], [[MAP3K14]], IKBKB, [[MYD88]] L265P) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Micronodular pattern of [[lymphocytic]] infiltration of the [[white pulp]] | |||
* Expanded [[mantle]] and [[marginal zone]] component with [[biphasic]] distribution of neoplastic cells | |||
* [[Diffuse]] or [[patchy]] [[red pulp]] involvement penetrating sinuses and cords | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[CD20]]+, [[CD79a]]+[[IgM]]+ | |||
* [[CD11c]]+, [[IgD]]+, DBA44+ in more than 50% of the cases | |||
* [[CD5]]+, [[CD25]]+, [[CD103]]+, [[IgG]]+ in less than 50% of the cases | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | |||
'''Splenic diffuse red pulp lymphoma''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Uncommon: 7q deletion, [[trisomy]] 18, 17p deletion ( [[TP53]]) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* No [[micronodular pattern]] | |||
* [[Effacement]] of [[white pulp]] | |||
* Obliteration of splenic architecture by neoplastic cells | |||
* [[Red pulp]] involvement with infiltration of both cord and sinuses | |||
* Extensive [[intra-sinusoidal]] involvement in the [[bone marrow]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[CD11c]]+,[[CD20]]+, [[CD79a]]+ DBA44+ | |||
* [[IgM]]+, [[IgD]]+, [[IgG]]+ in more than 50% of the cases | |||
* [[CD5]]+, [[CD103]]+, [[CD123]]+ in less than 50% of the cases | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | |||
'''Hairy cell leukemia variant''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Common: Deletion 17p ( [[TP53]]), | |||
* Uncommon: 5q gain, deletion 7q | |||
* Gene mutation: [[MAP2K1]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* More commonly [[sinusoidal]] or [[diffuse]] infiltration of the [[bone marrow]] | |||
* [[Peripheral blood]] picture predominant with [[prolymhocytes]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[CD11c]]+, [[ CD20]]+, [[CD79a]]+, [[CD103]]+, DBA44+ | |||
* [[IgG]]+ in more than 50% of the cases | |||
* [[IgD]]+, [[IgM]]+ in less than 50% of the cases | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | |||
'''Hairy cell leukemia''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Uncommon: 5q gain, 7q deletion | |||
* gene mutation: [[BRAF V600E]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Uniform involvement of [[red pulp]] | |||
* [[white pulp]] reduced in size | |||
* [[patchy]] [[infiltration]] of the [[bone marrow]] by [[hairy cells]]. | |||
* increase [[reticulin]] fiber replacing normal [[hematopoietic]] cells resulting in '''Dry tap''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[CD11c]]+, [[CD20]]+, [[CD79a]]+, [[CD25]]+, [[CD103]]+, [[CD123]]+, [[Annexin A1]]+, [[IgM]]+, [[IgD]]+, [[IgG]]+ | |||
* [[CD10]]+ in less than 50% of the cases | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | |||
'''Lymphoplasmacytic lymphoma''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Common: 6q deletion, | |||
* Uncommon: 13q deletion, 7q deletion | |||
* Gene mutation: [[MYD88]] L265P | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Homogeneous]] [[white pulp]] [[infiltration]] without visible [[marginal zone]] and monocytoid cells | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[CD11]]+,[[ CD20]]+, [[CD79a]]+ [[IgM]]+ | |||
* [[CD25]]+ in more than 50% of the cases | |||
* [[CD5]]+ in less than 50% of the cases | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | |||
'''Chronic lymphocytic leukemia''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Chromosomal deletion]] 6q, 7q, 13q, 17p | |||
* [[Trisomy]] 13 less frequently | |||
* Gene mutation: [[TP53]],[[SF3B1]], [[BIRC3]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Small mature [[neoplastic]] [[lymphoid]] cells | |||
* [[Bone marrow]] infiltration pattern may [[diffuse]], [[interstitial]], [[nodular]] | |||
* Intrasinusoidal pattern rarely observed | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[IgM]]+, [[IgD]]+, [[CD5]]+, [[CD23]]+, [[CD43]]+, [[CD79a]]+, [[LEF1]]+ | |||
* [[CD20]]+, DBA44+ in less than 50% | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | |||
'''Follicular lymphoma''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* t(14;18) [[translocation]] | |||
* Gene mutation: BCL2 | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Follicles]] in the [[white pulp]] consisting of centroblasts and centrocytes | |||
* [[Diffuse]] [[red pulp]] [[infiltration]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[IgM]]+, [[IgD]]+, [[CD20]]+, [[CD79a]]+, [[BCL6]]+ | |||
* [[CD10]]+ in more than 50% | |||
* [[CD23]]+ in less than 50% | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | |||
'''Mantle cell lymphoma''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* t(11;14) [[translocation]] | |||
* [[Gene mutation]]: [[CCND1]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Small neoplastic cells similar to centrocytes | |||
* [[Bone marrow]] [[infiltration]] pattern may be [[interstitial]], [[diffuse]] or [[nodular]] | |||
* Intrasinusoidal pattern rarely observed | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[IgM]]+, [[IgD]]+, [[CD5]]+, [[CD20]]+, [[CD43]]+, [[CD79a]]+, [[BCL1]]+, [[SOX11]]+ | |||
* [[BCL6]]+ and LEF1+ in less than 50% for the cases | |||
|} | |||
== | == Epidemiology and Demographics == | ||
===Age=== | |||
The incidence of intravascular large B-cell lymphoma increases with age; the median age at diagnosis is 67 years.<ref name="seer.cancer.gov">Intravascular large B-cell lymphoma. Surveillance, Epidemiology, and End Results Program. http://seer.cancer.gov/seertools/hemelymph/51f6cf5ae3e27c3994bd54a7/. Accessed on March 09, 2016 </ref> | |||
===Gender=== | |||
Intravascular large B-cell lymphoma affects men and women equally.<ref name="seer.cancer.gov">Intravascular large B-cell lymphoma. Surveillance, Epidemiology, and End Results Program. http://seer.cancer.gov/seertools/hemelymph/51f6cf5ae3e27c3994bd54a7/. Accessed on March 09, 2016 </ref> | |||
== Risk Factors == | |||
There are no established risk factors for intravascular large B-cell lymphoma. | |||
== | == Natural History, Complications and Prognosis== | ||
* Intravascular large B-cell lymphoma usually affects the small blood vessels in many organs, including: [[central nervous system]], kidneys, lungs, and skin. However, almost any site can be affected. | |||
* People with intravascular large B-cell lymphoma have a variety of symptoms. The symptoms will depend on the tissue or organ affected when the [[blood vessels]] become occluded. This type of [[lymphoma]] is often difficult to diagnose because the symptoms can be so varied. | |||
* Intravascular large B-cell lymphoma is a fast-growing (aggressive) [[lymphoma]]. | |||
* People with this type of [[lymphoma]] often have a poor prognosis. | |||
* People with this type of [[lymphoma]] can also develop a very serious condition where certain parts of the [[immune system]] are activated (hemophagocytic syndrome).<ref name="seer.cancer.gov">Intravascular large B-cell lymphoma. Surveillance, Epidemiology, and End Results Program. http://seer.cancer.gov/seertools/hemelymph/51f6cf5ae3e27c3994bd54a7/. Accessed on March 09, 2016 </ref> | |||
*[[Hemophagocytic syndrome]] causes: | |||
:*[[Fever]] | |||
:* Enlarged liver and spleen ([[hepatosplenomegaly]]) | |||
:* A lower number of [[red blood cells]], [[white blood cells]] and [[platelets]] in the blood ([[pancytopenia]]) | |||
== Diagnosis == | |||
===Staging=== | |||
Staging for Intravascular large B-cell lymphoma is provided in the following table:<ref>{{Cite journal| doi = 10.1200/JCO.2013.54.8800| issn = 1527-7755| volume = 32| issue = 27| pages = 3059–3068| last1 = Cheson| first1 = Bruce D.| last2 = Fisher| first2 = Richard I.| last3 = Barrington| first3 = Sally F.| last4 = Cavalli| first4 = Franco| last5 = Schwartz| first5 = Lawrence H.| last6 = Zucca| first6 = Emanuele| last7 = Lister| first7 = T. Andrew| last8 = Alliance, Australasian Leukaemia and Lymphoma Group| last9 = Eastern Cooperative Oncology Group| last10 = European Mantle Cell Lymphoma Consortium| last11 = Italian Lymphoma Foundation| last12 = European Organisation for Research| last13 = Treatment of Cancer/Dutch Hemato-Oncology Group| last14 = Grupo Español de Médula Ósea| last15 = German High-Grade Lymphoma Study Group| last16 = German Hodgkin's Study Group| last17 = Japanese Lymphorra Study Group| last18 = Lymphoma Study Association| last19 = NCIC Clinical Trials Group| last20 = Nordic Lymphoma Study Group| last21 = Southwest Oncology Group| last22 = United Kingdom National Cancer Research Institute| title = Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification| journal = Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology| date = 2014-09-20| pmid = 25113753}}</ref> | |||
== | {| style="border: 0px; font-size: 90%; margin: 3px;" align=center | ||
[[Intravascular large B-cell lymphoma | |+ '''Revised staging system for primary nodal lymphomas (Lugano classification)''' | ||
! style="background: #4479BA; color:#FFF;" | Stage | |||
! style="background: #4479BA; color:#FFF;" | Involvement | |||
! style="background: #4479BA; color:#FFF;" | Extranodal (E) status | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" colspan=3 | '''Limited''' | |||
|- | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Stage I | |||
| style="padding: 5px 5px; background: #F5F5F5;" | One node or a group of adjacent nodes | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Single extranodal lesions without nodal involvement | |||
|- | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Stage II | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Two or more nodal groups on the same side of the diaphragm | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Stage I or II by nodal extent with limited contiguous extranodal involvement | |||
|- | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Stage II bulky | |||
| style="padding: 5px 5px; background: #F5F5F5;" | II as above with "bulky" disease | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Not applicable | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" colspan=3 | '''Advanced''' | |||
|- | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Stage III | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Nodes on both sides of the diaphragm; nodes above the diaphragm with spleen involvement | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Not applicable | |||
|- | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Stage IV | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Additional noncontiguous extralymphatic involvement | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Not applicable | |||
|} | |||
=== Symptoms === | |||
People with intravascular large B-cell lymphoma have a variety of symptoms. The symptoms will depend on the tissue or organ affected when the [[blood vessels]] become occluded. This type of [[lymphoma]] is often difficult to diagnose because the symptoms can be so varied. | |||
Most common symptoms of the intravascular large B-cell lymphoma include:<ref name="seer.cancer.gov">Intravascular large B-cell lymphoma. Surveillance, Epidemiology, and End Results Program. http://seer.cancer.gov/seertools/hemelymph/51f6cf5ae3e27c3994bd54a7/. Accessed on March 09, 2016 </ref> | |||
* [[Fever]] | |||
* [[Weight loss]] | |||
* [[Night sweats]] | |||
* Painless swellings in the neck, axilla, groin, thorax, and abdomen | |||
* Pain in the chest, abdomen, or bones | |||
=== Physical Examination === | |||
====Vitals==== | |||
* [[Fever]] is often present | |||
====Skin==== | |||
* Skin rash | |||
====HEENT==== | |||
* [[Lymphadenopathy|Cervical lymphadenopathy]] | |||
====Thorax==== | |||
* Thoracic masses suggestive of [[Lymphadenopathy|central lymphadenopathy]] | |||
====Abdomen==== | |||
* [[Abdominal mass]]es suggestive of [[Lymphadenopathy|central lymphadenopathy]] | |||
* [[Hepatosplenomegaly]] | |||
====Extremities==== | |||
* [[Lymphadenopathy|Peripheral lymphadenopathy]] | |||
{| style="border: 0px; font-size: 90%; margin: 3px;" align=center | |||
|+ '''Intravascular large B-cell lymphoma clinical features based on organ involvement''' | |||
! style="background: #4479BA;; color:#FFF;" | Organ Involved | |||
! style="background: #4479BA;; color:#FFF;" | Clinical features | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Central nervous system | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* Focal sensory or motor deficits, generalized weakness, altered sensorium, rapidly progressive [[dementia]]<ref name="pmid28726030">{{cite journal |vauthors=Brett FM, Chen D, Loftus T, Langan Y, Looby S, Hutchinson S |title=Intravascular large B-cell lymphoma presenting clinically as rapidly progressive dementia |journal=Ir J Med Sci |volume=187 |issue=2 |pages=319–322 |date=May 2018 |pmid=28726030 |doi=10.1007/s11845-017-1653-5 |url=}}</ref>, [[seizures]], [[hemiparesis]], [[dysarthria]], [[ataxia]], [[vertigo]], and transient visual loss<ref name="pmid27546361">{{cite journal |vauthors=Kubisova K, Martanovic P, Sisovsky V, Tomleinova Z, Steno A, Janega P, Rychly B, Babal P |title=Dominant neurologic symptomatology in intravascular large B-cell lymphoma |journal=Bratisl Lek Listy |volume=117 |issue=6 |pages=308–11 |date=2016 |pmid=27546361 |doi= |url=}}</ref> | |||
|- | |||
| style="text-align: center; padding: 5px 5px; background: #F5F5F5;" | Cutaneous Involvement | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* Maculopapular eruptions, [[nodules]], [[plaques]], tumors, hyperpigmented patches, palpable [[purpura]], ulcers, and infiltrative “peau d’orange” | |||
|} | |||
===Laboratory Findings === | |||
Laboratory tests for intravascular large B-cell lymphoma include:<ref name="seer.cancer.gov">Intravascular large B-cell lymphoma. Surveillance, Epidemiology, and End Results Program. http://seer.cancer.gov/seertools/hemelymph/51f6cf5ae3e27c3994bd54a7/. Accessed on March 09, 2016 </ref> | |||
* [[Complete blood count]] (CBC): [[pancytopenia]] | |||
* Blood chemistry studies: | |||
* Cytogenetic analysis | |||
* [[Flow cytometry]] | |||
* [[Immunohistochemistry]] | |||
* [[Immunophenotyping]] | |||
====Biopsy==== | |||
Lymph node biopsy is diagnostic of intravascular large B-cell lymphoma. | |||
==== Other Imaging Findings ==== | |||
[[CT]], [[MRI]], and [[PET]] scan may be helpful in the diagnosis of intravascular large B-cell lymphoma. | |||
== | ==Treatment== | ||
* [[ | ===Medical Therapy=== | ||
* [[ | {| style="border: 0px; font-size: 90%; margin: 3px;" align=center | ||
|+ '''Treatment of intravascular large B-cell lymphoma<ref name="canadiancancer">Intravascular large B-cell lymphoma. Canadian Cancer Society. http://www.cancer.ca/en/cancer-information/cancer-type/non-hodgkin-lymphoma/non-hodgkin-lymphoma/types-of-nhl/intravascular-large-b-cell-lymphoma/?region=nb. Accessed on March 9, 2016 </ref>''' | |||
! style="background: #4479BA; color:#FFF;" | Therapy<ref name="pmid19717091">{{cite journal |vauthors=Shimada K, Kinoshita T, Naoe T, Nakamura S |title=Presentation and management of intravascular large B-cell lymphoma |journal=Lancet Oncol. |volume=10 |issue=9 |pages=895–902 |date=September 2009 |pmid=19717091 |doi=10.1016/S1470-2045(09)70140-8 |url=}}</ref> | |||
! style="background: #4479BA; color:#FFF;" | Description | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" | [[Chemotherapy]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* Combination therapy : | |||
:* CHOP – [[Cyclophosphamide]] {{and}} [[Doxorubicin]] {{and}} [[Vincristine]] {{and}} [[Prednisone]] | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" | [[Radiation therapy]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* [[External beam radiation therapy]] may be used. | |||
|} | |||
==References== | ==References== | ||
{{ | {{Reflist|2}} | ||
== | [[Category:Disease]] | ||
* [ | [[Category:Oncology]] | ||
==Related Chapters== | |||
* [[Richter's transformation]] | |||
* [[T-cell lymphoma]] | |||
| Line 64: | Line 299: | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | |||
[[Category:Medicine]] | |||
[[Category:Hematology]] | |||
[[Category:Immunology]] | |||
Latest revision as of 14:53, 18 October 2019
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sowminya Arikapudi, M.B,B.S. [2] Syed Musadiq Ali M.B.B.S.[3]
Synonyms and keywords: Intravascular lymphomatosis, angiotropic large cell lymphoma, angio-endotheliotropic (intravascular) lymphoma, angioendotheliomatosis proliferans systematisata, malignant angioendotheliomatosis
Overview
Intravascular large B-cell lymphoma is a very rare subtype of diffuse large B-cell lymphoma (DLBCL). It is also considered a distinct type of non-Hodgkin lymphoma (NHL) in the World Health Organization (WHO) classification system. Intravascular large B-cell lymphoma affects small blood vessels. It is a rare and aggressive variant of intravascular proliferation of clonal lymphocytes with little to no parenchymal involvement. Based on the clinical presentation, intravascular large B-cell lymphoma may be classified into either Western variant or Asian variant. On microscopic histopathological analysis, diffuse infiltrate of large atypical cells with irregular nuclear contours, vesicular chromatin, and occasional prominent nucleoli are characteristic findings of intravascular large b-cell lymphoma. The incidence of intravascular large B-cell lymphoma increases with age; the median age at diagnosis is 67 years. Intravascular large B-cell lymphoma affects men and women equally. People with this type of lymphoma often have a poor prognosis. Symptoms of the intravascular large B-cell lymphoma include fever, weight loss, night sweats, chest pain, abdominal pain, bone pain, and painless swellings in the neck, axilla, groin, thorax, and abdomen. Lymph node biopsy is diagnostic of intravascular large B-cell lymphoma. CT, MRI, and PET scan may be helpful in the diagnosis of intravascular large B-cell lymphoma. The predominant therapy for intravascular large B-cell lymphoma is chemotherapy. Adjunctive radiotherapy may be required.
Classification
Based on the clinical presentation, intravascular large B-cell lymphoma may be classified into either Western variant or Asian variant.
| Name | Description |
|---|---|
| Western variant |
|
| Asian variant |
|
Pathophysiology
Intravascular large B-cell lymphoma is characterized by a massive intravascular proliferation of atypical mononuclear cells which lodged in the lumina of small or intermediate vessels in many organs. The neoplastic lymphoid cells are large with prominent nucleoli and frequent mitotic figures. Fibrin thrombi, haemorrhage and necrosis may be seen[1].
Microscopic Pathology
On microscopic histopathological analysis, diffuse infiltrate of large atypical cells with irregular nuclear contours, vesicular chromatin, and occasional prominent nucleoli are characteristic findings of intravascular large b-cell lymphoma.

Causes
There are no established causes for intravascular large B-cell lymphoma.
Differentiating Intravascular Large B-Cell Lymphoma from other Diseases
Intravascular large B-cell lymphoma must be differentiated from other lymphomas with the help of clincal, morphological, immunophenotypic and genetic data as the treatment of all these conditions are different from each other.[2][3][4][5][6][7][8][9][10][11][12][13][14][15][16][17][18][19][20][21][22][23][24][25][26][27][23][28][29]
| Differential Diagnosis | Cytogenetics | Morphological Features | Immunophenotype |
|---|---|---|---|
|
Splenic marginal zone lymphoma |
|
||
|
Splenic diffuse red pulp lymphoma |
|
||
|
Hairy cell leukemia variant |
|
||
|
Hairy cell leukemia |
|
|
|
|
Lymphoplasmacytic lymphoma |
|
|
|
|
Chronic lymphocytic leukemia |
|
|
|
|
Follicular lymphoma |
|
|
|
|
Mantle cell lymphoma |
|
|
Epidemiology and Demographics
Age
The incidence of intravascular large B-cell lymphoma increases with age; the median age at diagnosis is 67 years.[30]
Gender
Intravascular large B-cell lymphoma affects men and women equally.[30]
Risk Factors
There are no established risk factors for intravascular large B-cell lymphoma.
Natural History, Complications and Prognosis
- Intravascular large B-cell lymphoma usually affects the small blood vessels in many organs, including: central nervous system, kidneys, lungs, and skin. However, almost any site can be affected.
- People with intravascular large B-cell lymphoma have a variety of symptoms. The symptoms will depend on the tissue or organ affected when the blood vessels become occluded. This type of lymphoma is often difficult to diagnose because the symptoms can be so varied.
- Intravascular large B-cell lymphoma is a fast-growing (aggressive) lymphoma.
- People with this type of lymphoma often have a poor prognosis.
- People with this type of lymphoma can also develop a very serious condition where certain parts of the immune system are activated (hemophagocytic syndrome).[30]
- Hemophagocytic syndrome causes:
- Fever
- Enlarged liver and spleen (hepatosplenomegaly)
- A lower number of red blood cells, white blood cells and platelets in the blood (pancytopenia)
Diagnosis
Staging
Staging for Intravascular large B-cell lymphoma is provided in the following table:[31]
| Stage | Involvement | Extranodal (E) status |
|---|---|---|
| Limited | ||
| Stage I | One node or a group of adjacent nodes | Single extranodal lesions without nodal involvement |
| Stage II | Two or more nodal groups on the same side of the diaphragm | Stage I or II by nodal extent with limited contiguous extranodal involvement |
| Stage II bulky | II as above with "bulky" disease | Not applicable |
| Advanced | ||
| Stage III | Nodes on both sides of the diaphragm; nodes above the diaphragm with spleen involvement | Not applicable |
| Stage IV | Additional noncontiguous extralymphatic involvement | Not applicable |
Symptoms
People with intravascular large B-cell lymphoma have a variety of symptoms. The symptoms will depend on the tissue or organ affected when the blood vessels become occluded. This type of lymphoma is often difficult to diagnose because the symptoms can be so varied. Most common symptoms of the intravascular large B-cell lymphoma include:[30]
- Fever
- Weight loss
- Night sweats
- Painless swellings in the neck, axilla, groin, thorax, and abdomen
- Pain in the chest, abdomen, or bones
Physical Examination
Vitals
- Fever is often present
Skin
- Skin rash
HEENT
Thorax
- Thoracic masses suggestive of central lymphadenopathy
Abdomen
- Abdominal masses suggestive of central lymphadenopathy
- Hepatosplenomegaly
Extremities
| Organ Involved | Clinical features |
|---|---|
| Central nervous system |
|
| Cutaneous Involvement |
Laboratory Findings
Laboratory tests for intravascular large B-cell lymphoma include:[30]
- Complete blood count (CBC): pancytopenia
- Blood chemistry studies:
- Cytogenetic analysis
- Flow cytometry
- Immunohistochemistry
- Immunophenotyping
Biopsy
Lymph node biopsy is diagnostic of intravascular large B-cell lymphoma.
Other Imaging Findings
CT, MRI, and PET scan may be helpful in the diagnosis of intravascular large B-cell lymphoma.
Treatment
Medical Therapy
| Therapy[35] | Description |
|---|---|
| Chemotherapy |
|
| Radiation therapy |
|
References
- ↑ di Fonzo H, Contardo D, Carrozza D, Finocchietto P, Rojano Crisson A, Cabral C, de Los Angeles Juarez M (May 2017). "Intravascular Large B Cell Lymphoma Presenting as Fever of Unknown Origin and Diagnosed by Random Skin Biopsies: A Case Report and Literature Review". Am J Case Rep. 18: 482–486. doi:10.12659/ajcr.903816. PMC 5421743. PMID 28461685.
- ↑ Matutes E, Oscier D, Montalban C, Berger F, Callet-Bauchu E, Dogan A, Felman P, Franco V, Iannitto E, Mollejo M, Papadaki T, Remstein ED, Salar A, Solé F, Stamatopoulos K, Thieblemont C, Traverse-Glehen A, Wotherspoon A, Coiffier B, Piris MA (March 2008). "Splenic marginal zone lymphoma proposals for a revision of diagnostic, staging and therapeutic criteria". Leukemia. 22 (3): 487–95. doi:10.1038/sj.leu.2405068. PMID 18094718.
- ↑ Salido M, Baró C, Oscier D, Stamatopoulos K, Dierlamm J, Matutes E, Traverse-Glehen A, Berger F, Felman P, Thieblemont C, Gesk S, Athanasiadou A, Davis Z, Gardiner A, Milla F, Ferrer A, Mollejo M, Calasanz MJ, Florensa L, Espinet B, Luño E, Wlodarska I, Verhoef G, García-Granero M, Salar A, Papadaki T, Serrano S, Piris MA, Solé F (September 2010). "Cytogenetic aberrations and their prognostic value in a series of 330 splenic marginal zone B-cell lymphomas: a multicenter study of the Splenic B-Cell Lymphoma Group". Blood. 116 (9): 1479–88. doi:10.1182/blood-2010-02-267476. PMID 20479288.
- ↑ Kiel MJ, Velusamy T, Betz BL, Zhao L, Weigelin HG, Chiang MY, Huebner-Chan DR, Bailey NG, Yang DT, Bhagat G, Miranda RN, Bahler DW, Medeiros LJ, Lim MS, Elenitoba-Johnson KS (August 2012). "Whole-genome sequencing identifies recurrent somatic NOTCH2 mutations in splenic marginal zone lymphoma". J. Exp. Med. 209 (9): 1553–65. doi:10.1084/jem.20120910. PMC 3428949. PMID 22891276.
- ↑ Rossi D, Trifonov V, Fangazio M, Bruscaggin A, Rasi S, Spina V, Monti S, Vaisitti T, Arruga F, Famà R, Ciardullo C, Greco M, Cresta S, Piranda D, Holmes A, Fabbri G, Messina M, Rinaldi A, Wang J, Agostinelli C, Piccaluga PP, Lucioni M, Tabbò F, Serra R, Franceschetti S, Deambrogi C, Daniele G, Gattei V, Marasca R, Facchetti F, Arcaini L, Inghirami G, Bertoni F, Pileri SA, Deaglio S, Foà R, Dalla-Favera R, Pasqualucci L, Rabadan R, Gaidano G (August 2012). "The coding genome of splenic marginal zone lymphoma: activation of NOTCH2 and other pathways regulating marginal zone development". J. Exp. Med. 209 (9): 1537–51. doi:10.1084/jem.20120904. PMC 3428941. PMID 22891273.
- ↑ Tiacci E, Trifonov V, Schiavoni G, Holmes A, Kern W, Martelli MP, Pucciarini A, Bigerna B, Pacini R, Wells VA, Sportoletti P, Pettirossi V, Mannucci R, Elliott O, Liso A, Ambrosetti A, Pulsoni A, Forconi F, Trentin L, Semenzato G, Inghirami G, Capponi M, Di Raimondo F, Patti C, Arcaini L, Musto P, Pileri S, Haferlach C, Schnittger S, Pizzolo G, Foà R, Farinelli L, Haferlach T, Pasqualucci L, Rabadan R, Falini B (June 2011). "BRAF mutations in hairy-cell leukemia". N. Engl. J. Med. 364 (24): 2305–15. doi:10.1056/NEJMoa1014209. PMID 21663470.
- ↑ Waterfall JJ, Arons E, Walker RL, Pineda M, Roth L, Killian JK, Abaan OD, Davis SR, Kreitman RJ, Meltzer PS (January 2014). "High prevalence of MAP2K1 mutations in variant and IGHV4-34-expressing hairy-cell leukemias". Nat. Genet. 46 (1): 8–10. doi:10.1038/ng.2828. PMC 3905739. PMID 24241536.
- ↑ Traverse-Glehen A, Baseggio L, Bauchu EC, Morel D, Gazzo S, Ffrench M, Verney A, Rolland D, Thieblemont C, Magaud JP, Salles G, Coiffier B, Berger F, Felman P (February 2008). "Splenic red pulp lymphoma with numerous basophilic villous lymphocytes: a distinct clinicopathologic and molecular entity?". Blood. 111 (4): 2253–60. doi:10.1182/blood-2007-07-098848. PMID 18042795.
- ↑ Braggio E, Dogan A, Keats JJ, Chng WJ, Huang G, Matthews JM, Maurer MJ, Law ME, Bosler DS, Barrett M, Lossos IS, Witzig TE, Fonseca R (May 2012). "Genomic analysis of marginal zone and lymphoplasmacytic lymphomas identified common and disease-specific abnormalities". Mod. Pathol. 25 (5): 651–60. doi:10.1038/modpathol.2011.213. PMC 3341516. PMID 22301699.
- ↑ Traverse-Glehen A, Bachy E, Baseggio L, Callet-Bauchu E, Gazzo S, Verney A, Hayette S, Jallades L, Ffrench M, Salles G, Coiffier B, Felman P, Berger F (May 2013). "Immunoarchitectural patterns in splenic marginal zone lymphoma: correlations with chromosomal aberrations, IGHV mutations, and survival. A study of 76 cases". Histopathology. 62 (6): 876–93. doi:10.1111/his.12092. PMID 23611359.
- ↑ Xi L, Arons E, Navarro W, Calvo KR, Stetler-Stevenson M, Raffeld M, Kreitman RJ (April 2012). "Both variant and IGHV4-34-expressing hairy cell leukemia lack the BRAF V600E mutation". Blood. 119 (14): 3330–2. doi:10.1182/blood-2011-09-379339. PMC 3321859. PMID 22210875.
- ↑ Matutes E, Morilla R, Owusu-Ankomah K, Houlihan A, Catovsky D (March 1994). "The immunophenotype of splenic lymphoma with villous lymphocytes and its relevance to the differential diagnosis with other B-cell disorders". Blood. 83 (6): 1558–62. PMID 8123845.
- ↑ Venkataraman G, Aguhar C, Kreitman RJ, Yuan CM, Stetler-Stevenson M (October 2011). "Characteristic CD103 and CD123 expression pattern defines hairy cell leukemia: usefulness of CD123 and CD103 in the diagnosis of mature B-cell lymphoproliferative disorders". Am. J. Clin. Pathol. 136 (4): 625–30. doi:10.1309/AJCPKUM9J4IXCWEU. PMID 21917686.
- ↑ Ponzoni M, Kanellis G, Pouliou E, Baliakas P, Scarfò L, Ferreri AJ, Doglioni C, Bikos V, Dagklis A, Anagnostopoulos A, Ghia P, Stamatopoulos K, Papadaki T (November 2012). "Bone marrow histopathology in the diagnostic evaluation of splenic marginal-zone and splenic diffuse red pulp small B-cell lymphoma: a reliable substitute for spleen histopathology?". Am. J. Surg. Pathol. 36 (11): 1609–18. doi:10.1097/PAS.0b013e318271243d. PMID 23073320.
- ↑ Falini B, Tiacci E, Liso A, Basso K, Sabattini E, Pacini R, Foa R, Pulsoni A, Dalla Favera R, Pileri S (June 2004). "Simple diagnostic assay for hairy cell leukaemia by immunocytochemical detection of annexin A1 (ANXA1)". Lancet. 363 (9424): 1869–70. doi:10.1016/S0140-6736(04)16356-3. PMID 15183626.
- ↑ Kanellis G, Mollejo M, Montes-Moreno S, Rodriguez-Pinilla SM, Cigudosa JC, Algara P, Montalban C, Matutes E, Wotherspoon A, Piris MA (July 2010). "Splenic diffuse red pulp small B-cell lymphoma: revision of a series of cases reveals characteristic clinico-pathological features". Haematologica. 95 (7): 1122–9. doi:10.3324/haematol.2009.013714. PMID 20220064.
- ↑ Hunter ZR, Xu L, Yang G, Zhou Y, Liu X, Cao Y, Manning RJ, Tripsas C, Patterson CJ, Sheehy P, Treon SP (March 2014). "The genomic landscape of Waldenstrom macroglobulinemia is characterized by highly recurring MYD88 and WHIM-like CXCR4 mutations, and small somatic deletions associated with B-cell lymphomagenesis". Blood. 123 (11): 1637–46. doi:10.1182/blood-2013-09-525808. PMID 24366360.
- ↑ Went PT, Zimpfer A, Pehrs AC, Sabattini E, Pileri SA, Maurer R, Terracciano L, Tzankov A, Sauter G, Dirnhofer S (April 2005). "High specificity of combined TRAP and DBA.44 expression for hairy cell leukemia". Am. J. Surg. Pathol. 29 (4): 474–8. PMID 15767800.
- ↑ Morice WG, Chen D, Kurtin PJ, Hanson CA, McPhail ED (June 2009). "Novel immunophenotypic features of marrow lymphoplasmacytic lymphoma and correlation with Waldenström's macroglobulinemia". Mod. Pathol. 22 (6): 807–16. doi:10.1038/modpathol.2009.34. PMID 19287458.
- ↑ Behdad A, Bailey NG (October 2014). "Diagnosis of splenic B-cell lymphomas in the bone marrow: a review of histopathologic, immunophenotypic, and genetic findings". Arch. Pathol. Lab. Med. 138 (10): 1295–301. doi:10.5858/arpa.2014-0291-CC. PMID 25268192.
- ↑ Shao H, Calvo KR, Grönborg M, Tembhare PR, Kreitman RJ, Stetler-Stevenson M, Yuan CM (April 2013). "Distinguishing hairy cell leukemia variant from hairy cell leukemia: development and validation of diagnostic criteria". Leuk. Res. 37 (4): 401–409. doi:10.1016/j.leukres.2012.11.021. PMC 5575750. PMID 23347903.
- ↑ Konkay K, Uppin MS, Uppin SG, Raghunadha Rao D, Geetha C, Paul TR (September 2014). "Hairy cell leukemia: clinicopathological and immunophenotypic study". Indian J Hematol Blood Transfus. 30 (3): 180–6. doi:10.1007/s12288-013-0231-x. PMC 4115087. PMID 25114404. Vancouver style error: initials (help)
- ↑ 23.0 23.1 Rudolf-Oliveira RC, Pirolli MM, de Souza FS, Michels J, Santos-Silva MC (2015). "Hairy cell leukemia variant: the importance of differential diagnosis". Rev Bras Hematol Hemoter. 37 (2): 132–5. doi:10.1016/j.bjhh.2015.01.003. PMC 4382572. PMID 25818826.
- ↑ Pileri SA, Falini B (November 2009). "Mantle cell lymphoma". Haematologica. 94 (11): 1488–92. doi:10.3324/haematol.2009.013359. PMC 2770958. PMID 19880776.
- ↑ Traverse-Glehen A, Baseggio L, Salles G, Coiffier B, Felman P, Berger F (April 2012). "Splenic diffuse red pulp small-B cell lymphoma: toward the emergence of a new lymphoma entity". Discov Med. 13 (71): 253–65. PMID 22541613.
- ↑ Rahman K, Subramanian PG, Kadam PA, Gadage V, Galani K, Mittal N, Ghogale S, Badrinath Y, Ansari R, Kushte S, Nair R, Sengar M, Menon H, Gujral S (2012). "Morphological spectrum of leukemic mantle cell lymphoma". Indian J Pathol Microbiol. 55 (1): 66–71. doi:10.4103/0377-4929.94860. PMID 22499304.
- ↑ Cessna MH, Hartung L, Tripp S, Perkins SL, Bahler DW (January 2005). "Hairy cell leukemia variant: fact or fiction". Am. J. Clin. Pathol. 123 (1): 132–8. PMID 15762289.
- ↑ Kansal R, Singleton TP, Ross CW, Finn WG, Padmore RF, Schnitzer B (January 2002). "Follicular hodgkin lymphoma: a histopathologic study". Am. J. Clin. Pathol. 117 (1): 29–35. doi:10.1309/M7YV-V8V2-A5VA-J1Y4. PMID 11789727.
- ↑ Autore F, Strati P, Laurenti L, Ferrajoli A (June 2018). "Morphological, immunophenotypic, and genetic features of chronic lymphocytic leukemia with trisomy 12: a comprehensive review". Haematologica. 103 (6): 931–938. doi:10.3324/haematol.2017.186684. PMC 6058775. PMID 29748447.
- ↑ 30.0 30.1 30.2 30.3 30.4 Intravascular large B-cell lymphoma. Surveillance, Epidemiology, and End Results Program. http://seer.cancer.gov/seertools/hemelymph/51f6cf5ae3e27c3994bd54a7/. Accessed on March 09, 2016
- ↑ Cheson, Bruce D.; Fisher, Richard I.; Barrington, Sally F.; Cavalli, Franco; Schwartz, Lawrence H.; Zucca, Emanuele; Lister, T. Andrew; Alliance, Australasian Leukaemia and Lymphoma Group; Eastern Cooperative Oncology Group; European Mantle Cell Lymphoma Consortium; Italian Lymphoma Foundation; European Organisation for Research; Treatment of Cancer/Dutch Hemato-Oncology Group; Grupo Español de Médula Ósea; German High-Grade Lymphoma Study Group; German Hodgkin's Study Group; Japanese Lymphorra Study Group; Lymphoma Study Association; NCIC Clinical Trials Group; Nordic Lymphoma Study Group; Southwest Oncology Group; United Kingdom National Cancer Research Institute (2014-09-20). "Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification". Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 32 (27): 3059–3068. doi:10.1200/JCO.2013.54.8800. ISSN 1527-7755. PMID 25113753.
- ↑ Brett FM, Chen D, Loftus T, Langan Y, Looby S, Hutchinson S (May 2018). "Intravascular large B-cell lymphoma presenting clinically as rapidly progressive dementia". Ir J Med Sci. 187 (2): 319–322. doi:10.1007/s11845-017-1653-5. PMID 28726030.
- ↑ Kubisova K, Martanovic P, Sisovsky V, Tomleinova Z, Steno A, Janega P, Rychly B, Babal P (2016). "Dominant neurologic symptomatology in intravascular large B-cell lymphoma". Bratisl Lek Listy. 117 (6): 308–11. PMID 27546361.
- ↑ Intravascular large B-cell lymphoma. Canadian Cancer Society. http://www.cancer.ca/en/cancer-information/cancer-type/non-hodgkin-lymphoma/non-hodgkin-lymphoma/types-of-nhl/intravascular-large-b-cell-lymphoma/?region=nb. Accessed on March 9, 2016
- ↑ Shimada K, Kinoshita T, Naoe T, Nakamura S (September 2009). "Presentation and management of intravascular large B-cell lymphoma". Lancet Oncol. 10 (9): 895–902. doi:10.1016/S1470-2045(09)70140-8. PMID 19717091.
Related Chapters