Hyperkalemia: Difference between revisions
No edit summary |
|||
| Line 17: | Line 17: | ||
'''Hyperkalemia''' (AE) or '''Hyperkalaemia''' (BE) is an elevated blood level (above 5.0 mmol/L) of the [[electrolyte]] [[potassium]]. The prefix ''hyper-'' means high (contrast with ''hypo-'', meaning low). The middle ''kal'' refers to ''kalium'', which is [[Latin]] for potassium. The end portion of the word, ''-emia'', means "in the blood". Extreme degrees of hyperkalemia are considered a [[medical emergency]] due to the risk of potentially fatal [[arrhythmia]]s. | '''Hyperkalemia''' (AE) or '''Hyperkalaemia''' (BE) is an elevated blood level (above 5.0 mmol/L) of the [[electrolyte]] [[potassium]]. The prefix ''hyper-'' means high (contrast with ''hypo-'', meaning low). The middle ''kal'' refers to ''kalium'', which is [[Latin]] for potassium. The end portion of the word, ''-emia'', means "in the blood". Extreme degrees of hyperkalemia are considered a [[medical emergency]] due to the risk of potentially fatal [[arrhythmia]]s. | ||
==[[Hyperkalemia differential diagnosis | Differential diagnosis]]== | |||
==[[ Hyperkalemia pathophysiology | Pathophysiology ]]== | |||
==[[Hyperkalemia history and symptoms | History and Symptoms ]]== | ==[[Hyperkalemia history and symptoms | History and Symptoms ]]== | ||
| Line 57: | Line 59: | ||
Pseudohyperkalemia is a rise in the amount of potassium that occurs due to excessive leakage of potassium from cells, during or after blood is drawn. It is a laboratory artifact rather than a biological abnormality and can be misleading to doctors.<ref>Sevastos N et al. (2006) Pseudohyperkalemia in serum: the phenomenon and its clinical magnitude. J Lab Clin Med, 147(3):139-44; PMID 16503244.</ref> Pseudohyperkalemia is typically caused by [[hemolysis]] during [[venipuncture]] (by either excessive vacuum of the blood draw or by a syringe needle that is of too fine a gauge); excessive tournequet time or fist clenching during phlebotomy (which presumably leads to efflux of potassium from the muscle cells into the bloodstream).<ref>Don BR et al. (1990) Pseudohyperkalemia caused by fist clenching during phlebotomy. N Engl J Med, 322(18):1290-2; PMID 2325722.</ref>; or by a delay in the processing of the blood specimen. It can also occur in specimens from patients with abnormally high numbers of [[platelet]]s (>1,000,000/mm³), [[leukocyte]]s (> 100 000/mm³), or [[erythrocyte]]s (hematocrit > 55%). People with "leakier" [[cell membrane]]s have been found, whose blood must be separated immediately to avoid pseudohyperkalemia.<ref>Iolascon A et al. (1999) Familial pseudohyperkalemia maps to the same locus as dehydrated hereditary stomatocytosis. Blood, 93(9):3120-3; PMID 10216110.</ref> | Pseudohyperkalemia is a rise in the amount of potassium that occurs due to excessive leakage of potassium from cells, during or after blood is drawn. It is a laboratory artifact rather than a biological abnormality and can be misleading to doctors.<ref>Sevastos N et al. (2006) Pseudohyperkalemia in serum: the phenomenon and its clinical magnitude. J Lab Clin Med, 147(3):139-44; PMID 16503244.</ref> Pseudohyperkalemia is typically caused by [[hemolysis]] during [[venipuncture]] (by either excessive vacuum of the blood draw or by a syringe needle that is of too fine a gauge); excessive tournequet time or fist clenching during phlebotomy (which presumably leads to efflux of potassium from the muscle cells into the bloodstream).<ref>Don BR et al. (1990) Pseudohyperkalemia caused by fist clenching during phlebotomy. N Engl J Med, 322(18):1290-2; PMID 2325722.</ref>; or by a delay in the processing of the blood specimen. It can also occur in specimens from patients with abnormally high numbers of [[platelet]]s (>1,000,000/mm³), [[leukocyte]]s (> 100 000/mm³), or [[erythrocyte]]s (hematocrit > 55%). People with "leakier" [[cell membrane]]s have been found, whose blood must be separated immediately to avoid pseudohyperkalemia.<ref>Iolascon A et al. (1999) Familial pseudohyperkalemia maps to the same locus as dehydrated hereditary stomatocytosis. Blood, 93(9):3120-3; PMID 10216110.</ref> | ||
=== Laboratory Evaluation === | === Laboratory Evaluation === | ||
====Initial==== | ====Initial==== | ||
Revision as of 03:14, 26 November 2011
| Hyperkalemia | |
 | |
|---|---|
| potassium | |
| ICD-10 | E87.5 |
| ICD-9 | 276.7 |
| DiseasesDB | 6242 |
| MeSH | D006947 |
|
Hyperkalemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hyperkalemia On the Web |
|
American Roentgen Ray Society Images of Hyperkalemia |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Priyamvada Singh, M.B.B.S. [2]
Overview
Hyperkalemia (AE) or Hyperkalaemia (BE) is an elevated blood level (above 5.0 mmol/L) of the electrolyte potassium. The prefix hyper- means high (contrast with hypo-, meaning low). The middle kal refers to kalium, which is Latin for potassium. The end portion of the word, -emia, means "in the blood". Extreme degrees of hyperkalemia are considered a medical emergency due to the risk of potentially fatal arrhythmias.
Differential diagnosis
Pathophysiology
History and Symptoms
Diagnosis
In order to gather enough information for diagnosis, the measurement of potassium needs to be repeated, as the elevation can be due to hemolysis in the first sample. Generally, blood tests for renal function (creatinine, blood urea nitrogen), glucose and occasionally creatine kinase and cortisol will be performed. Calculating the trans-tubular potassium gradient can sometimes help in distinguishing the cause of the hyperkalemia.
In many cases, renal ultrasound will be performed, since hyperkalemia is highly suggestive of renal failure.
Also, electrocardiography (EKG/ECG) may be performed to determine if there is a significant risk of cardiac arrhythmias (see ECG/EKG Findings, below).
Causes include:
Ineffective elimination from the body
- Renal insufficiency
- Medication that interferes with urinary excretion:
- ACE inhibitors and angiotensin receptor blockers
- Potassium-sparing diuretics (e.g. amiloride and spironolactone)
- NSAIDs such as ibuprofen, naproxen, or celecoxib
- The calcineurin inhibitor immunosuppressants ciclosporin and tacrolimus
- The antibiotic trimethoprim
- The antiparasitic drug pentamidine
- Mineralocorticoid deficiency or resistance, such as:
- Addison's disease
- Aldosterone deficiency, including reduced levels due to the blood thinner, heparin
- Some forms of congenital adrenal hyperplasia
- Type IV renal tubular acidosis (resistance of renal tubules to aldosterone)
- Gordon's syndrome (“familial hypertension with hyperkalemia”), a rare genetic disorder caused by defective modulators of salt transporters, including the thiazide-sensitive Na-Cl cotransporter.
Excessive release from cells
- Rhabdomyolysis, burns or any cause of rapid tissue necrosis, including tumor lysis syndrome
- Massive blood transfusion or massive hemolysis
- Shifts/transport out of cells caused by acidosis, low insulin levels, beta-blocker therapy, digoxin overdose, or the paralyzing anesthetic succinylcholine
Excessive intake
- Intoxication with salt-substitute, potassium-containing dietary supplements, or potassium-chloride (KCl) infusion. Note that for a person with normal kidney function and nothing interfering with normal elimination (see above), hyperkalemia by potassium intoxication would be seen only with large infusions of KCl or massive doses of oral KCl supplements.
Lethal injection
Hyperkalemia is intentionally brought about in an execution by lethal injection, potassium chloride being the third and last of the three drugs generally administered to cause death, after sodium thiopental has rendered the subject unconscious, then pancuronium bromide has been added to cause respiratory collapse.
Pseudohyperkalemia
Pseudohyperkalemia is a rise in the amount of potassium that occurs due to excessive leakage of potassium from cells, during or after blood is drawn. It is a laboratory artifact rather than a biological abnormality and can be misleading to doctors.[1] Pseudohyperkalemia is typically caused by hemolysis during venipuncture (by either excessive vacuum of the blood draw or by a syringe needle that is of too fine a gauge); excessive tournequet time or fist clenching during phlebotomy (which presumably leads to efflux of potassium from the muscle cells into the bloodstream).[2]; or by a delay in the processing of the blood specimen. It can also occur in specimens from patients with abnormally high numbers of platelets (>1,000,000/mm³), leukocytes (> 100 000/mm³), or erythrocytes (hematocrit > 55%). People with "leakier" cell membranes have been found, whose blood must be separated immediately to avoid pseudohyperkalemia.[3]
Laboratory Evaluation
Initial
- Calcium
- Phosphate
- Magnesium
- Blood urea nitrogen (BUN)/creatinine
Extensive Evaluation
- Cortisol
- Renin
- Aldosterone levels
- Transtubular potassium gradient (by assessing potassium+ secretion)
Electrocardiographic Findings
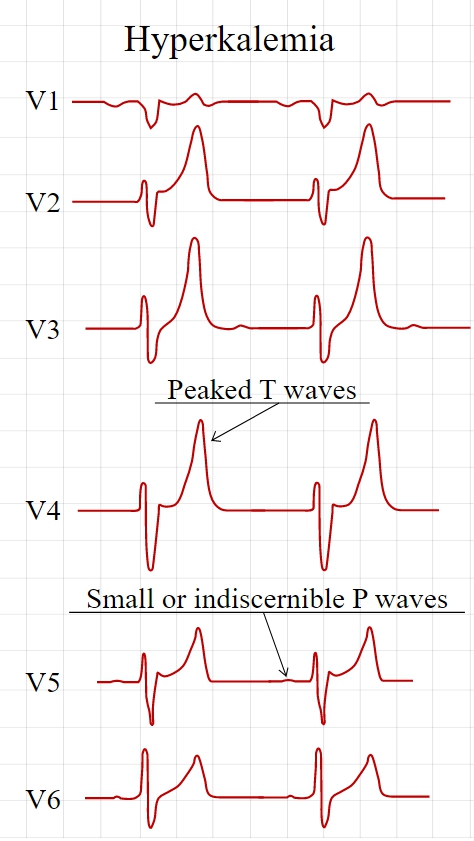
Electrocardiography (ECG) is generally done early to identify any influences on the heart, as hyperkalemia may cause fatal arrhythmias. With moderate hyperkalemia, there is reduction of the size of the P wave and development of tent-shaped T waves. Further hyperkalemia will lead to widening of the QRS complex, that ultimately may become sinusoidal in shape. There appears to be a direct effect of elevated potassium on some of the potassium channels that increases their activity and speeds membrane repolarization. Also, (as noted above), hyperkalemia causes an overall membrane depolarization that inactivates many sodium channels. The faster repolarization of the cardiac action potential causes the tenting of the T waves, and the inactivation of sodium channels causes a sluggish conduction of the electrical wave around the heart, which leads to smaller P waves and widening of the QRS complex.
Spcific findings include the following:
Tall, narrow, and peaked T waves
- Earliest sign of hyperkalemia
- Occurs with K > 5.5 meq/li
- Differential diagnosis of this EKG change includes the T wave changes of bradycardia or stroke. Prominent U waves and QTc prolongation are more consistent with stroke than hyperkalemia.
Intraventricular conduction defect
Decrease of the amplitude of the P wave or an absent P wave
- Decreased P wave amplitude occurs when the K is > 7.0 meq/li
- P waves may be absent when the K is > 8.8 meq/li
- The impulses are still being generated in the SA node and are conducted to the ventricles through specialized atrial fibers without depolarizing the atrial muscle
- Moderate or sever hyperkalemia can cause sinus arrest [4]
ST segment changes simulating current of injury
- Have been labeled the dialyzable current of injury
Cardiac arrhythmias: bradyarrhythmias, tachyarrhythmias, atrioventricular conduction defects
- Occurs with severe hyperkalemia, not mild to moderate hyperkalemia
-
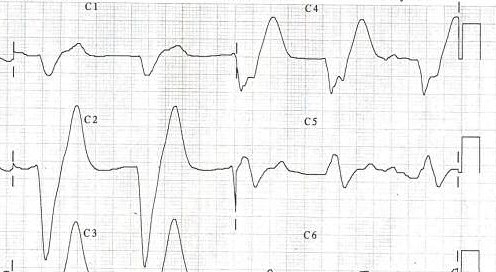
Tall, symmetric, narrow based T waves in a hyperkalemic patient.
-
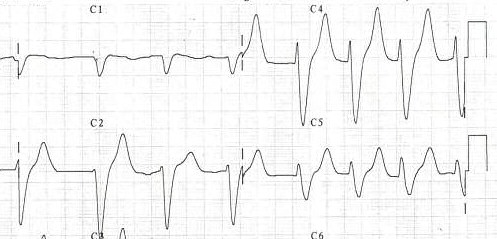
A patient's EKG with hyperkalemia.
-
Same patient's EKG during treatment.
Treatment
When arrhythmias occur, or when potassium levels exceed 6.5 mmol/l, emergency lowering of potassium levels is mandated. Several agents are used to lower K levels. Choice depends on the degree and cause of the hyperkalemia, and other aspects of the patient's condition.
- Calcium supplementation (calcium gluconate 10% (10ml), preferably through a central venous catheter as the calcium may cause phlebitis) does not lower potassium but decreases myocardial excitability, protecting against life threatening arrhythmias.
- Insulin (e.g. intravenous injection of 10-15u of (short acting) insulin (e.g. Actrapid) {along with 50ml of 50% dextrose to prevent hypoglycemia}) will lead to a shift of potassium ions into cells, secondary to increased activity of the sodium-potassium ATPase.
- Bicarbonate therapy (e.g. 1 ampule (45mEq) infused over 5 minutes) is effective in cases of metabolic acidosis. The bicarbonate ion will stimulate an exchange of cellular H+ for Na+, thus leading to stimulation of the sodium-potassium ATPase.
- Salbutamol (albuterol, Ventolin®) is a β2-selective catacholamine that is administered by nebuliser (e.g. 10-20 mg). This drug promotes movement of K into cells, lowering the blood levels.
- Polystyrene sulfonate (Calcium Resonium, Kayexalate) is a binding resin that binds K within the intestine and removes it from the body by defecation. Calcium Resonium (15g three times a day in water) can be given by mouth. Kayexelate can be given by mouth or as an enema. In both cases, the resin absorbs K within the intestine and carries it out of the body by defecation. This medication may cause diarrhea.
- Refractory or severe cases may need dialysis to remove the potassium from the circulation.
- Preventing recurrence of hyperkalemia typically involves reduction of dietary potassium, removal of an offending medication, and/or the addition of a diuretic (such as furosemide (Lasix®) or hydrochlorothiazide).
See also
References
- ↑ Sevastos N et al. (2006) Pseudohyperkalemia in serum: the phenomenon and its clinical magnitude. J Lab Clin Med, 147(3):139-44; PMID 16503244.
- ↑ Don BR et al. (1990) Pseudohyperkalemia caused by fist clenching during phlebotomy. N Engl J Med, 322(18):1290-2; PMID 2325722.
- ↑ Iolascon A et al. (1999) Familial pseudohyperkalemia maps to the same locus as dehydrated hereditary stomatocytosis. Blood, 93(9):3120-3; PMID 10216110.
- ↑ Bonvini RF, Hendiri T, Anwar A (2006). "Sinus arrest and moderate hyperkalemia". Annales De Cardiologie Et D'angéiologie. 55 (3): 161–3. PMID 16792034. Unknown parameter
|month=ignored (help)
Template:Endocrine, nutritional and metabolic pathology