Glucagonoma differential diagnosis: Difference between revisions
| Line 3: | Line 3: | ||
{{CMG}}; {{AE}} {{PSD}} {{MAD}} | {{CMG}}; {{AE}} {{PSD}} {{MAD}} | ||
==Overview== | ==Overview== | ||
Glucagonoma must be differentiated from certain skin lesions in which necrolytic migratory erythema can be found such as [[acrodermatitis enteropathica]], [[psoriasis]], [[pellagra]], and [[eczema]]. Glucagonoma should be differentiated from other causes of hyperglycemia include [[infection]], [[diabetes mellitus]], [[Cushing syndrome]], [[renal failure]], [[acute pancreatitis]], severe stress, and prolonged fasting. | Glucagonoma must be differentiated from certain skin lesions in which [[necrolytic migratory erythema]] can be found such as [[acrodermatitis enteropathica]], [[psoriasis]], [[pellagra]], and [[eczema]]. Glucagonoma should be differentiated from other causes of [[hyperglycemia]] include [[infection]], [[diabetes mellitus]], [[Cushing syndrome]], [[renal failure]], [[acute pancreatitis]], severe stress, and prolonged fasting. | ||
==Differentiating Glucagonoma from other Diseases== | ==Differentiating Glucagonoma from other Diseases== | ||
| Line 38: | Line 38: | ||
| | | | ||
* '''Serum glucagon''' | * '''Serum glucagon''' | ||
** Increased plasma glucagon levels (>500 pg/mL) | ** Increased plasma [[glucagon]] levels (>500 pg/mL) | ||
** Concentrations above 1000 pg/mL are diagnostic of glucagonoma | ** Concentrations above 1000 pg/mL are diagnostic of glucagonoma | ||
* CT scan is used to determine: | * [[CT scan]] is used to determine: | ||
**The location of the tumor | **The location of the tumor | ||
**Metastasis (usually liver metastasis) | **Metastasis (usually liver metastasis) | ||
| Line 48: | Line 48: | ||
|- | |- | ||
|[[Pemphigus foliaceus]].<ref name="pmid15993235">{{cite journal| author=Bystryn JC, Rudolph JL| title=Pemphigus. | journal=Lancet | year= 2005 | volume= 366 | issue= 9479 | pages= 61-73 | pmid=15993235 | doi=10.1016/S0140-6736(05)66829-8 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15993235 }}</ref><sup>[[Pemphigus foliaceus#cite note-Bolognia-2|[2]]]</sup><ref name="pmid159414332">{{cite journal| author=Chams-Davatchi C, Valikhani M, Daneshpazhooh M, Esmaili N, Balighi K, Hallaji Z et al.| title=Pemphigus: analysis of 1209 cases. | journal=Int J Dermatol | year= 2005 | volume= 44 | issue= 6 | pages= 470-6 | pmid=15941433 | doi=10.1111/j.1365-4632.2004.02501.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15941433 }}</ref><ref name="pmid21353333">{{cite journal| author=Martin LK, Werth VP, Villaneuva EV, Murrell DF| title=A systematic review of randomized controlled trials for pemphigus vulgaris and pemphigus foliaceus. | journal=J Am Acad Dermatol | year= 2011 | volume= 64 | issue= 5 | pages= 903-8 | pmid=21353333 | doi=10.1016/j.jaad.2010.04.039 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21353333 }}</ref> | |[[Pemphigus foliaceus]].<ref name="pmid15993235">{{cite journal| author=Bystryn JC, Rudolph JL| title=Pemphigus. | journal=Lancet | year= 2005 | volume= 366 | issue= 9479 | pages= 61-73 | pmid=15993235 | doi=10.1016/S0140-6736(05)66829-8 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15993235 }}</ref><sup>[[Pemphigus foliaceus#cite note-Bolognia-2|[2]]]</sup><ref name="pmid159414332">{{cite journal| author=Chams-Davatchi C, Valikhani M, Daneshpazhooh M, Esmaili N, Balighi K, Hallaji Z et al.| title=Pemphigus: analysis of 1209 cases. | journal=Int J Dermatol | year= 2005 | volume= 44 | issue= 6 | pages= 470-6 | pmid=15941433 | doi=10.1111/j.1365-4632.2004.02501.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15941433 }}</ref><ref name="pmid21353333">{{cite journal| author=Martin LK, Werth VP, Villaneuva EV, Murrell DF| title=A systematic review of randomized controlled trials for pemphigus vulgaris and pemphigus foliaceus. | journal=J Am Acad Dermatol | year= 2011 | volume= 64 | issue= 5 | pages= 903-8 | pmid=21353333 | doi=10.1016/j.jaad.2010.04.039 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21353333 }}</ref> | ||
|Autoimmune blistering disease of the skin with characteristic lesions that are scaly, crusted erosions, often on an erythematous base.<sup>[[Pemphigus foliaceus#cite note-Fitz2-1|[1]]]</sup> | |[[Autoimmunity|Autoimmune]] blistering [[disease]] of the skin with characteristic lesions that are [[Scaly leg|scaly]], crusted erosions, often on an [[Erythematous rash|erythematous base]].<sup>[[Pemphigus foliaceus#cite note-Fitz2-1|[1]]]</sup> | ||
Mucosal involvement is absent even with widespread disease | [[Mucosal]] involvement is absent even with widespread [[disease]] | ||
| | | | ||
* Cutaneous lesion that usually develops in a seborrheic distribution | * Cutaneous lesion that usually develops in a [[Seborrheic eczema|seborrheic]] distribution | ||
* The scalp, face, and trunk are common sites of involvement | * The [[scalp]], [[face]], and [[trunk]] are common sites of involvement | ||
* Skin lesions may remain localized or may coalesce to cover large areas of skin | * [[Skin lesions]] may remain localized or may [[Coalescence (chemistry)|coalesce]] to cover large areas of [[skin]] | ||
* Pain or burning sensations frequently accompany the cutaneous lesions | * Pain or burning sensations frequently accompany the cutaneous lesions | ||
* Systemic symptoms are usually absent | * Systemic symptoms are usually absent | ||
| | | | ||
* The skin lesions usually consist of small, scattered superficial blisters | * The skin lesions usually consist of small, scattered superficial [[blisters]] | ||
** Lesions rapidly evolve into scaly, crusted erosions | ** Lesions rapidly evolve into scaly, crusted erosions | ||
** Positive Nikolsky sign | ** Positive [[Nikolsky's sign|Nikolsky sign]] | ||
* Occasionally, pemphigus foliaceus progresses to involve the entire skin surface as an exfoliative erythroderma | * Occasionally, [[pemphigus foliaceus]] progresses to involve the entire skin surface as an [[Exfoliative skin disease|exfoliative erythroderma]] | ||
|Autoimmune [[IgG]] build up in the [[Epidermis (skin)|epidermis]], then nearly almost all of the antibodies are aimed against [[desmoglein 1]] | |Autoimmune [[IgG]] build up in the [[Epidermis (skin)|epidermis]], then nearly almost all of the [[antibodies]] are aimed against [[desmoglein 1]] | ||
|[[File:Pemphigus foliaceus08.jpg|center|250px|thumb|<small>Courtesy:http://www.atlasdermatologico.com.br/index.jsf</small>]] | |[[File:Pemphigus foliaceus08.jpg|center|250px|thumb|<small>Courtesy:http://www.atlasdermatologico.com.br/index.jsf</small>]] | ||
|- | |- | ||
|[[Psoriasis|Pustular psoriasis]]<sup>[[Psoriasis history and symptoms#cite note-pmid1390163-2|[2]]]</sup><sup>[[Psoriasis history and symptoms#cite note-pmid24790463-3|[3]]]</sup> | |[[Psoriasis|Pustular psoriasis]]<sup>[[Psoriasis history and symptoms#cite note-pmid1390163-2|[2]]]</sup><sup>[[Psoriasis history and symptoms#cite note-pmid24790463-3|[3]]]</sup> | ||
| | | | ||
* Positive family history of psoriasis | * Positive family history of [[psoriasis]] | ||
*Frequent association with [[histocompatibility]] [[antigen]] (HLA)- Cw6 | *Frequent association with [[histocompatibility]] [[antigen]] (HLA)- Cw6 | ||
* A history of a long-term [[erythematous]] scaly area with [[ocular]] and [[joint]] involvement | * A history of a long-term [[erythematous]] scaly area with [[ocular]] and [[joint]] involvement | ||
* Past medical history of the patient may | * Past medical history of the patient may include: | ||
**[[Viral]] or [[bacterial]] infection | **[[Viral]] or [[bacterial]] infection | ||
** [[Diabetes mellitus| | ** [[Diabetes mellitus|Diabetes]] | ||
** [[Hypertension]] | ** [[Hypertension]] | ||
** [[Chronic kidney disease]] | ** [[Chronic kidney disease]] | ||
**[[Obesity]] | **[[Obesity]] | ||
| | | | ||
* [[Pain]](unpleasant, superficial, sensitive, itchy, hot or burning) | * [[Pain]](unpleasant, superficial, sensitive, [[itchy]], hot or burning) | ||
* [[Pruritus]] | * [[Pruritus]] | ||
* High [[fever]] | * High [[fever]] | ||
* Dystrophic nails | * [[Dystrophic calcification|Dystrophic]] nails | ||
* Recent presentation of [[arthralgia]] | * Recent presentation of [[arthralgia]] | ||
| | | | ||
| Line 90: | Line 90: | ||
* Scaling [[Papule|papules]] and [[Plaque|plaques]] | * Scaling [[Papule|papules]] and [[Plaque|plaques]] | ||
* [[Koebner phenomenon]]: appearance of new psoriatic lesions at the site of skin injury | * [[Koebner phenomenon]]: appearance of new psoriatic lesions at the site of skin injury | ||
* [[Woronoff|Woronoff’s ring]]: ring of peripheral blanching skin around a | * [[Woronoff|Woronoff’s ring]]: ring of peripheral blanching skin around a [[psoriatic]] [[plaque]] | ||
* Auspitz’s sign: | * [[Auspitz's sign|Auspitz’s sign]]: | ||
** Small [[bleeding]] points are seen upon disruption of a psoriatic scale | ** Small [[bleeding]] points are seen upon disruption of a [[psoriatic]] scale | ||
| | | | ||
* '''Skin biopsy''' | * '''Skin biopsy''' | ||
| Line 104: | Line 104: | ||
**[[Edema]] of [[dermal]] [[papillae]] | **[[Edema]] of [[dermal]] [[papillae]] | ||
**[[Basal cell layer]] is expanded | **[[Basal cell layer]] is expanded | ||
* Leukocytosis | * [[Leukocytosis]] | ||
|[[File:Pus.png|center|250px|thumb|<small>Courtesy:http://www.atlasdermatologico.com.br/index.jsf</small>]] | |[[File:Pus.png|center|250px|thumb|<small>Courtesy:http://www.atlasdermatologico.com.br/index.jsf</small>]] | ||
|- | |- | ||
| Line 111: | Line 111: | ||
* An [[autosomal]] [[recessive]] disorder characterized by: | * An [[autosomal]] [[recessive]] disorder characterized by: | ||
**Periorificial and acral [[dermatitis]], [[alopecia]], and [[diarrhea]] | **Periorificial and acral [[dermatitis]], [[alopecia]], and [[diarrhea]] | ||
* The genetic base is a [[mutation]] of [[SLC39A4]] which encodes a [[transmembrane protein]] that serves as a zinc uptake protein | * The genetic base is a [[mutation]] of [[SLC39A4]] which encodes a [[transmembrane protein]] that serves as a [[zinc]] uptake protein | ||
| | | | ||
* Symptoms appear in infants after breast milk weaning | * Symptoms appear in infants after breast milk weaning | ||
| Line 117: | Line 117: | ||
* [[Diarrhea]] | * [[Diarrhea]] | ||
| | | | ||
* [[Erythematous]] | * [[Erythematous]]<nowiki/>patches/plaques of dry and [[Scale|scaly]] skin | ||
* The lesions may appear [[Eczematous Scaling|eczematous]] or may evolve into [[Crust|crusted]] [[vesicles]], [[Bulla|bullae]] or [[pustules]] | * The lesions may appear [[Eczematous Scaling|eczematous]] or may evolve into [[Crust|crusted]] [[vesicles]], [[Bulla|bullae]] or [[pustules]] | ||
| Line 136: | Line 136: | ||
|[[Pellagra]]<ref name="pmid12777163">{{cite journal| author=Prousky JE| title=Pellagra may be a rare secondary complication of anorexia nervosa: a systematic review of the literature. | journal=Altern Med Rev | year= 2003 | volume= 8 | issue= 2 | pages= 180-5 | pmid=12777163 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12777163 }}</ref><ref name="pmid21128910">{{cite journal| author=Wan P, Moat S, Anstey A| title=Pellagra: a review with emphasis on photosensitivity. | journal=Br J Dermatol | year= 2011 | volume= 164 | issue= 6 | pages= 1188-200 | pmid=21128910 | doi=10.1111/j.1365-2133.2010.10163.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21128910 }}</ref> | |[[Pellagra]]<ref name="pmid12777163">{{cite journal| author=Prousky JE| title=Pellagra may be a rare secondary complication of anorexia nervosa: a systematic review of the literature. | journal=Altern Med Rev | year= 2003 | volume= 8 | issue= 2 | pages= 180-5 | pmid=12777163 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12777163 }}</ref><ref name="pmid21128910">{{cite journal| author=Wan P, Moat S, Anstey A| title=Pellagra: a review with emphasis on photosensitivity. | journal=Br J Dermatol | year= 2011 | volume= 164 | issue= 6 | pages= 1188-200 | pmid=21128910 | doi=10.1111/j.1365-2133.2010.10163.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21128910 }}</ref> | ||
| | | | ||
* | * Niacin deficiency disease characterized by | ||
**[[Photosensitivity| | **[[Photosensitivity|Photosensitivity]] | ||
**Pigmented [[dermatitis]] | **Pigmented [[dermatitis]] | ||
** [[Diarrhea]] | ** [[Diarrhea]] | ||
** [[Dementia]]. | ** [[Dementia]]. | ||
* Hisotry of: | * Hisotry of: | ||
**[[Alcoholic| | **[[Alcoholic|Alcoholics]] | ||
** [[Bariatric surgery]] | ** [[Bariatric surgery]] | ||
** [[Anorexia nervosa]] | ** [[Anorexia nervosa]] | ||
| Line 155: | Line 155: | ||
* [[Diarrhea]] | * [[Diarrhea]] | ||
* [[Dementia]] | * [[Dementia]] | ||
|Symmetric | |Symmetric [[Hyperpigmentation|hyperpigmented]] [[rash]], similar in color and distribution to a sunburn, which is present in the exposed areas of skin | ||
|[[Niacin]] status can be assessed by measuring urinary [[N-methylnicotinamide]] or by measuring the erythrocyte [[NAD|NAD/]][[NADP]] ratio | |[[Niacin]] status can be assessed by measuring urinary [[N-methylnicotinamide]] or by measuring the erythrocyte [[NAD|NAD/]][[NADP]] ratio | ||
|[[File:Pellagra24.jpg|center|250px|thumb|<small>Courtesy:http://www.atlasdermatologico.com.br/index.jsf</small>]] | |[[File:Pellagra24.jpg|center|250px|thumb|<small>Courtesy:http://www.atlasdermatologico.com.br/index.jsf</small>]] | ||
| Line 161: | Line 161: | ||
|[[eczema|Chronic eczema]] ([[atopic dermatitis]]) | |[[eczema|Chronic eczema]] ([[atopic dermatitis]]) | ||
| | | | ||
* Chronic pruritic inflammatory skin disease | * Chronic [[Pruritic disorders|pruritic]] inflammatory skin disease | ||
*Occurs most frequently in children but also affects adults | *Occurs most frequently in children but also affects adults | ||
* Family history of: | * Family history of: | ||
| Line 168: | Line 168: | ||
**[[Asthma]] | **[[Asthma]] | ||
**[[Allergic rhinitis]]) | **[[Allergic rhinitis]]) | ||
* History of [[dermatitis]] involving the skin creases | * History of [[dermatitis]] involving the [[Skin crease|skin creases]] | ||
* Personal or family history of [[asthma]] or [[hay fever]] | * Personal or family history of [[asthma]] or [[hay fever]] | ||
| | | | ||
* Symptoms beginning in a child before the age of 2 years or, in children <4 years | * Symptoms beginning in a child before the age of 2 years or, in children <4 years | ||
* Dermatitis affecting the cheeks or dorsal aspect of extremities | * [[Dermatitis]] affecting the cheeks or dorsal aspect of extremities | ||
* Dry skin and severe [[pruritus]] that is associated with cutaneous [[ | * Dry skin and severe [[pruritus]] that is associated with [[cutaneous]] [[hyperactivity]] to various environmental stimuli | ||
* Exposure to: | * Exposure to: | ||
**Food and inhalant allergens | **Food and inhalant allergens | ||
**Irritants | **[[Irritants]] | ||
**Infection | **[[Infection]] | ||
| | | | ||
* Visible [[dermatitis]] involving flexural surfaces | * Visible [[dermatitis]] involving flexural surfaces | ||
| Line 185: | Line 185: | ||
* Raised [[IgE]] or an [[eosinophilia]] | * Raised [[IgE]] or an [[eosinophilia]] | ||
* [[RAST test|Radioallergosorbent Test]]: | * [[RAST test|Radioallergosorbent Test]]: | ||
**Blood is mixed separately with many different allergens and the antibody levels measured | **[[Blood]] is mixed separately with many different [[allergens]] and the [[antibody]] levels measured | ||
* [[Skin biopsy]]: | * [[Skin biopsy]]: | ||
** A procedure that removes a small piece of the affected skin and sent for [[microscopic examination]] in a pathology laboratory | ** A procedure that removes a small piece of the affected skin and sent for [[microscopic examination]] in a pathology laboratory | ||
| Line 200: | Line 200: | ||
* [[Diabetes insipidus]] | * [[Diabetes insipidus]] | ||
* Transient hyperglycemia | * Transient hyperglycemia | ||
* Steroid therapy | * [[Steroid]] therapy | ||
* [[Renal tubular acidosis|Renal tubular acidosis type-1]] | * [[Renal tubular acidosis|Renal tubular acidosis type-1]] | ||
* [[Glucagonoma]] | * [[Glucagonoma]] | ||
| Line 209: | Line 209: | ||
{| style="border: 0px; font-size: 90%; margin: 3px;" align="center" | {| style="border: 0px; font-size: 90%; margin: 3px;" align="center" | ||
! rowspan="2 | ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | ||
! colspan="5 | ! colspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |History and symptoms | ||
! colspan="8 | ! colspan="8" style="background:#4479BA; color: #FFFFFF;" align="center" |Laboratory findings | ||
! rowspan="2 | ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Additional findings | ||
|- | |- | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Polyuria | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Polydipsia | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Polyphagia | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss | |||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Weight gain | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Serum glucose | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Urinary Glucose | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Urine PH | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Serum Sodium | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Urinary Glucose | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" |24 hrs cortisol level | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" |C-peptide level | ||
! | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Serum glucagon | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Diabetes mellitus type 1|Type 1 Diabetes mellitus]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Diabetes mellitus type 1|Type 1 Diabetes mellitus]] | ||
Revision as of 15:26, 20 November 2017
|
Glucagonoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Glucagonoma differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Glucagonoma differential diagnosis |
|
Risk calculators and risk factors for Glucagonoma differential diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Parminder Dhingra, M.D. [2] Mohammed Abdelwahed M.D[3]
Overview
Glucagonoma must be differentiated from certain skin lesions in which necrolytic migratory erythema can be found such as acrodermatitis enteropathica, psoriasis, pellagra, and eczema. Glucagonoma should be differentiated from other causes of hyperglycemia include infection, diabetes mellitus, Cushing syndrome, renal failure, acute pancreatitis, severe stress, and prolonged fasting.
Differentiating Glucagonoma from other Diseases
Glucagonoma must be differentiated from certain skin lesions in which necrolytic migratory erythema can be found such as:[1]
| Disease | Clinical Picture | Investigations | Pictures | ||
|---|---|---|---|---|---|
| History | Symptoms | Signs | |||
| Glucagonoma[2][3][4][5] | A family history of multiple endocrine neoplasia type 1 |
|
|
|
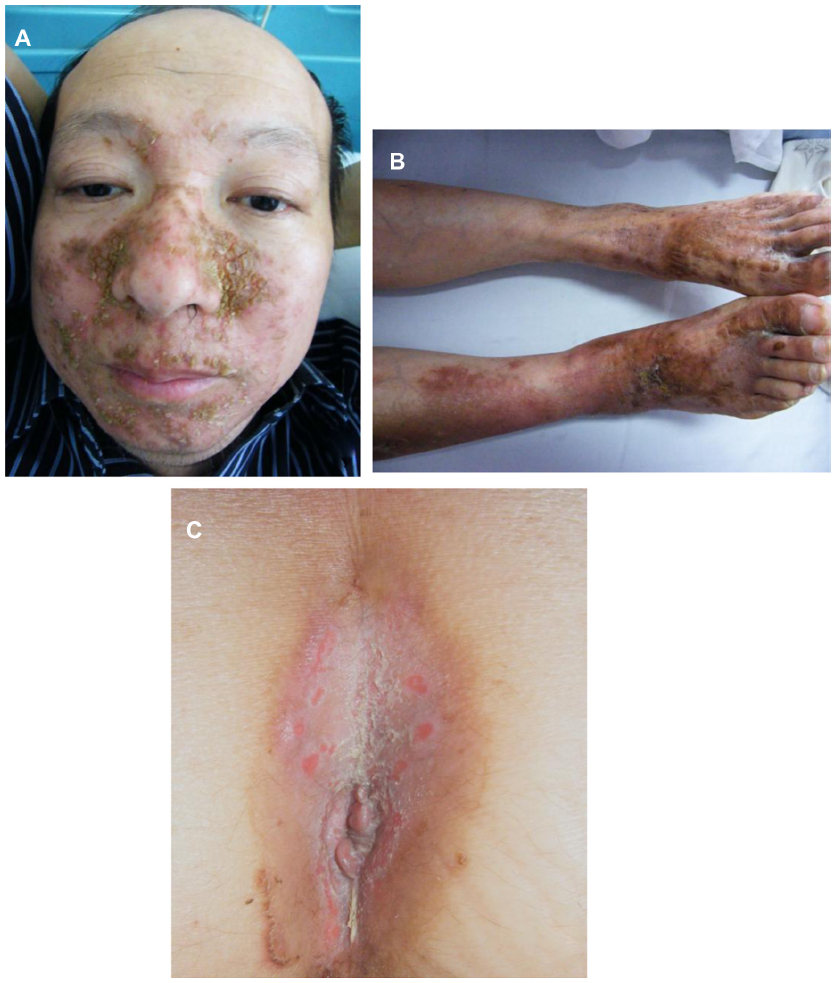 |
| Pemphigus foliaceus.[6][2][7][8] | Autoimmune blistering disease of the skin with characteristic lesions that are scaly, crusted erosions, often on an erythematous base.[1] |
|
|
Autoimmune IgG build up in the epidermis, then nearly almost all of the antibodies are aimed against desmoglein 1 |  |
| Pustular psoriasis[2][3] |
|
|
|
|
 |
| Acrodermatitis enteropathica[9][10][11] |
|
|
|
|
 |
| Pellagra[12][13] |
|
Symmetric hyperpigmented rash, similar in color and distribution to a sunburn, which is present in the exposed areas of skin | Niacin status can be assessed by measuring urinary N-methylnicotinamide or by measuring the erythrocyte NAD/NADP ratio |  | |
| Chronic eczema (atopic dermatitis) |
|
|
|
|
 |
Differentiating glucagonoma from other causes of hyperglycemia:
Glucagonoma can be differentiated from other causes of hyperglycemia which include:[14][15][16]
- Type 2 DM
- MODY-DM
- Psychogenic polydipsia
- Diabetes insipidus
- Transient hyperglycemia
- Steroid therapy
- Renal tubular acidosis type-1
- Glucagonoma
- Cushing's syndrome
- Hypothyroidism
- Wolfram syndrome
- Alstrom syndrome
| Disease | History and symptoms | Laboratory findings | Additional findings | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Polyuria | Polydipsia | Polyphagia | Weight loss | Weight gain | Serum glucose | Urinary Glucose | Urine PH | Serum Sodium | Urinary Glucose | 24 hrs cortisol level | C-peptide level | Serum glucagon | ||
| Type 1 Diabetes mellitus | ✔ | ✔ | ✔ | ✔ | - | ↑ | ↑ | Normal | Normal | N/↑ | Normal | ↓ | Normal | Auto antibodies present (Anti GAD-65 and anti insulin anti bodies) |
| Type 2 Diabetes mellitus | ✔ | ✔ | ✔ | ✔ | - | ↑ | ↑ | Normal | Normal | ↑ | Normal | Normal | ↑ | Acanthosis nigricans |
| MODY | ✔ | ✔ | ✔ | - | ✔ | ↑ | ↑ | Normal | Normal | ↑ | Normal | Normal | N | - |
| Psychogenic polydipsia | ✔ | ✔ | - | - | - | Normal | Normal | Normal | ↓ | Normal | Normal | Normal | Normal | - |
| Diabetes insipidus | ✔ | ✔ | - | - | - | Normal | Normal | Normal | ↑ | Normal | Normal | Normal | Normal | - |
| Transient hyperglycemia | - | - | - | - | - | ↑ | ↑ | Normal | Normal | ↑ | Normal | Normal | N/↑ | In hospitalized patients especially in ICU and CCU |
| Steroid therapy | ✔ | - | - | - | ✔ | ↑ | ↑ | Normal | Normal | ↑ | ↑ | N/↑ | N/↑ | Acanthosis nigricans, |
| RTA 1 | - | - | - | ✔ | - | Normal | Normal | ↑ | Normal | ↑ | Normal | Normal | Normal | Hypokalemia, nephrolithiasis |
| Glucagonoma | - | - | - | - | - | ↑ | Normal | Normal | Normal | - | Normal | Normal | ↑ | Necrolytic migratory erythema |
| Cushing syndrome | - | - | - | - | ✔ | ↑ | - | Normal | ↓ | N/↑ | ↑ | Normal | Normal | Moon face, obesity, buffalo hump, easy bruisibility |
References
- ↑ Fang S, Li S, Cai T (2014). "Glucagonoma syndrome: a case report with focus on skin disorders". Onco Targets Ther. 7: 1449–53. doi:10.2147/OTT.S66285. PMC 4140234. PMID 25152626.
- ↑ Wilkinson DS (1973). "Necrolytic migratory erythema with carcinoma of the pancreas". Trans St Johns Hosp Dermatol Soc. 59 (2): 244–50. PMID 4793623.
- ↑ Wermers RA, Fatourechi V, Wynne AG, Kvols LK, Lloyd RV (1996). "The glucagonoma syndrome. Clinical and pathologic features in 21 patients". Medicine (Baltimore). 75 (2): 53–63. PMID 8606627.
- ↑ Zhang M, Xu X, Shen Y, Hu ZH, Wu LM, Zheng SS (2004). "Clinical experience in diagnosis and treatment of glucagonoma syndrome". HBPD INT. 3 (3): 473–5. PMID 15313692.
- ↑ Kindmark H, Sundin A, Granberg D, Dunder K, Skogseid B, Janson ET, Welin S, Oberg K, Eriksson B (2007). "Endocrine pancreatic tumors with glucagon hypersecretion: a retrospective study of 23 cases during 20 years". Med. Oncol. 24 (3): 330–7. PMID 17873310.
- ↑ Bystryn JC, Rudolph JL (2005). "Pemphigus". Lancet. 366 (9479): 61–73. doi:10.1016/S0140-6736(05)66829-8. PMID 15993235.
- ↑ Chams-Davatchi C, Valikhani M, Daneshpazhooh M, Esmaili N, Balighi K, Hallaji Z; et al. (2005). "Pemphigus: analysis of 1209 cases". Int J Dermatol. 44 (6): 470–6. doi:10.1111/j.1365-4632.2004.02501.x. PMID 15941433.
- ↑ Martin LK, Werth VP, Villaneuva EV, Murrell DF (2011). "A systematic review of randomized controlled trials for pemphigus vulgaris and pemphigus foliaceus". J Am Acad Dermatol. 64 (5): 903–8. doi:10.1016/j.jaad.2010.04.039. PMID 21353333.
- ↑ Prasad AS, Cossack ZT (1984). "Zinc supplementation and growth in sickle cell disease". Ann Intern Med. 100 (3): 367–71. PMID 6696358.
- ↑ Meftah S, Prasad AS, Lee DY, Brewer GJ (1991). "Ecto 5' nucleotidase (5'NT) as a sensitive indicator of human zinc deficiency". J Lab Clin Med. 118 (4): 309–16. PMID 1940572.
- ↑ Kiliç I, Ozalp I, Coŝkun T, Tokatli A, Emre S, Saldamli I; et al. (1998). "The effect of zinc-supplemented bread consumption on school children with asymptomatic zinc deficiency". J Pediatr Gastroenterol Nutr. 26 (2): 167–71. PMID 9481631.
- ↑ Prousky JE (2003). "Pellagra may be a rare secondary complication of anorexia nervosa: a systematic review of the literature". Altern Med Rev. 8 (2): 180–5. PMID 12777163.
- ↑ Wan P, Moat S, Anstey A (2011). "Pellagra: a review with emphasis on photosensitivity". Br J Dermatol. 164 (6): 1188–200. doi:10.1111/j.1365-2133.2010.10163.x. PMID 21128910.
- ↑ Barrett TG (2007). "Differential diagnosis of type 1 diabetes: which genetic syndromes need to be considered?". Pediatr Diabetes. 8 Suppl 6: 15–23. doi:10.1111/j.1399-5448.2007.00278.x. PMID 17727381.
- ↑ Type 1 Diabetes mellitus "Dennis Kasper, Anthony Fauci, Stephen Hauser, Dan Longo, J. Larry Jameson, Joseph Loscalzo"Harrison's Principles of Internal Medicine, 19e Accessed on December 27th,2016
- ↑ "namrata".