Differentiating psoriasis from other diseases: Difference between revisions
No edit summary |
No edit summary |
||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
Psoriasis must be differentiated from other diseases that cause [[erythematous]], scaly [[Rash erythematous|rash]] such as [[cutaneous T cell lymphoma]]/[[mycosis fungoides]], [[pityriasis rosea]], [[pityriasis rubra pilaris]], [[pityriasis lichenoides chronica]], [[nummular dermatitis]], [[secondary syphilis]], [[Bowen’s disease]], [[exanthematous pustulosis]], [[Lichen planus|hypertrophic lichen planus]], Sneddon–Wilkinson disease, [[Parapsoriasis|small plaque parapsoriasis]], [[intertrigo]], [[Langerhans cell histiocytosis]], [[dyshidrotic dermatitis]], [[tinea manuum]]/pedum/[[Tinea capitis|capitis]] and [[seborrheic dermatitis]]. | Psoriasis must be differentiated from other diseases that cause [[erythematous]], scaly [[Rash erythematous|rash]] such as [[cutaneous T cell lymphoma]]/[[mycosis fungoides]], [[pityriasis rosea]], [[pityriasis rubra pilaris]], [[pityriasis lichenoides chronica]], [[nummular dermatitis]], [[secondary syphilis]], [[Bowen’s disease]], [[exanthematous pustulosis]], [[Lichen planus|hypertrophic lichen planus]], Sneddon–Wilkinson disease, [[Parapsoriasis|small plaque parapsoriasis]], [[intertrigo]], [[Langerhans cell histiocytosis]], [[dyshidrotic dermatitis]], [[tinea manuum]]/pedum/[[Tinea capitis|capitis]], and [[seborrheic dermatitis]]. | ||
==Differentiating psoriasis from other diseases== | ==Differentiating psoriasis from other diseases== | ||
=== Differential diagnosis of psoriasis === | === Differential diagnosis of psoriasis === | ||
*Psoriasis must be differentiated from other diseases causing [[Papulosquamous disorder|papulosquamous]] or [[Erythematous rash|erythematosquamous rash]] especially when the psoriatic [[lesions]] are localized in particular sites as [[Palms of the hands|palms]], [[soles]], [[scalp]], body folds, [[penis]] and [[Nail (anatomy)|nails]]. | *Psoriasis must be differentiated from other diseases causing [[Papulosquamous disorder|papulosquamous]] or [[Erythematous rash|erythematosquamous rash]], especially when the psoriatic [[lesions]] are localized in particular sites as [[Palms of the hands|palms]], [[soles]], [[scalp]], body folds, [[penis]], and [[Nail (anatomy)|nails]]. | ||
*The differential diagnosis of psoriasis includes: | *The differential diagnosis of psoriasis includes: | ||
**[[Cutaneous T cell lymphoma]]/[[mycosis fungoides]] | **[[Cutaneous T cell lymphoma]]/[[mycosis fungoides]] | ||
| Line 37: | Line 37: | ||
| | | | ||
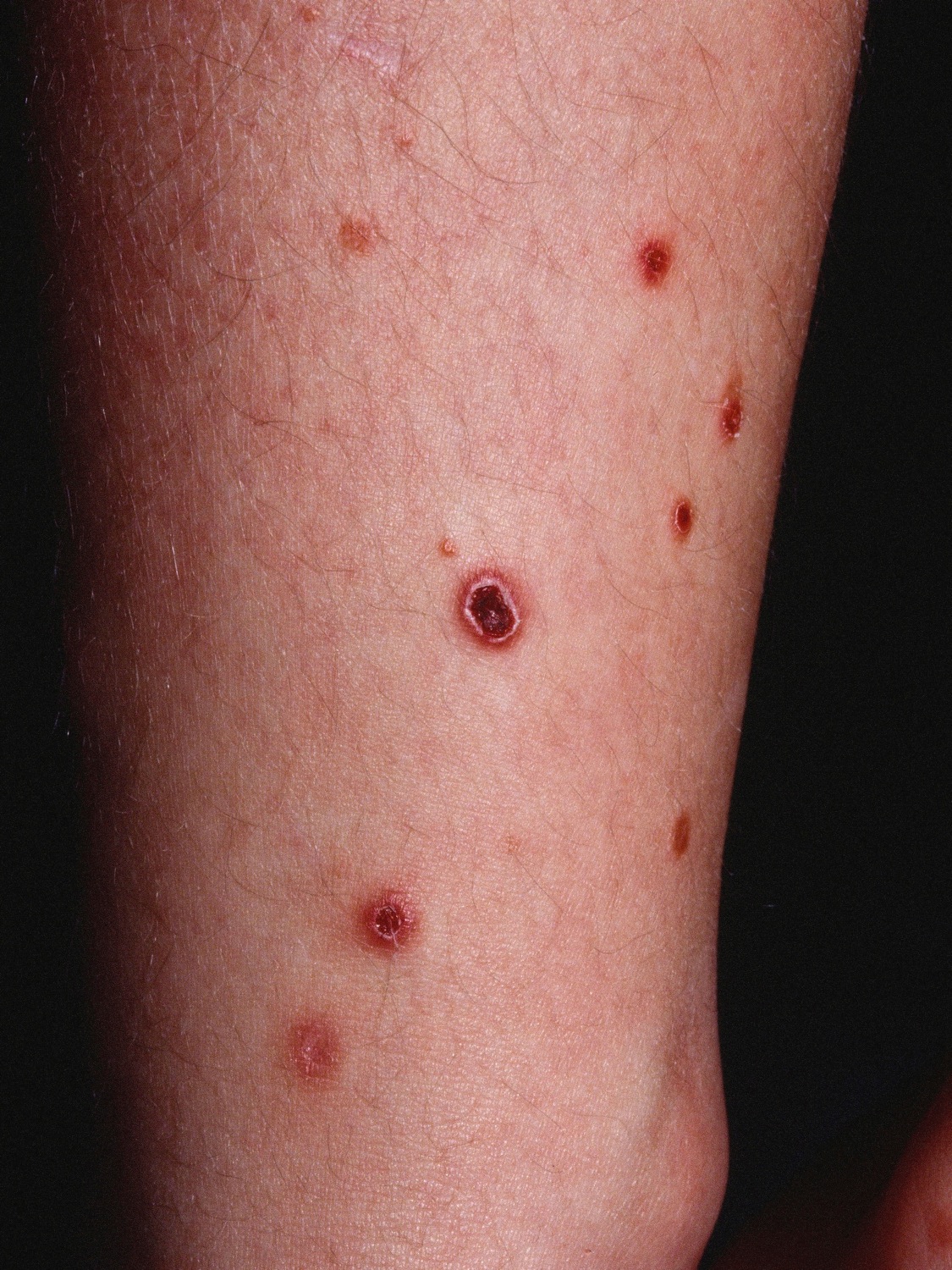
* '''Premycotic phase:''' A scaly, red [[rash]] in areas of the [[body]] that usually are not exposed to the sun. This rash does not cause symptoms and may last for months or years. | * '''Premycotic phase:''' A scaly, red [[rash]] in areas of the [[body]] that usually are not exposed to the sun. This rash does not cause symptoms and may last for months or years. | ||
* '''Patch phase:''' Thin, reddened, [[eczema]] | * '''Patch phase:''' Thin, reddened, [[eczema]]-like rash. | ||
* '''[[Plaque]] phase:''' Small raised [[Bumps on skin|bumps]] ([[Papule|papules]]) or | * '''[[Plaque]] phase:''' Small raised [[Bumps on skin|bumps]] ([[Papule|papules]]) or hardened [[lesions]] on the skin, which may be reddened. | ||
* '''[[Tumor]] phase:''' Tumors form on the [[skin]]. These tumors may develop [[Ulcer|ulcers]]<nowiki/>and the skin may get infected. | * '''[[Tumor]] phase:''' Tumors form on the [[skin]]. These tumors may develop [[Ulcer|ulcers]]<nowiki/> and the skin may get infected. | ||
| | | | ||
* [[Epidermis (skin)|Epidermal]] [[atrophy]] or poikiloderma | * [[Epidermis (skin)|Epidermal]] [[atrophy]] or poikiloderma | ||
* Generalized [[itching]] ([[pruritus]]) | * Generalized [[itching]] ([[pruritus]]) | ||
* [[Pain]] in the affected area of the skin | * [[Pain]] in the affected area of the skin | ||
* [[Insomnia]] | * [[Insomnia]] | ||
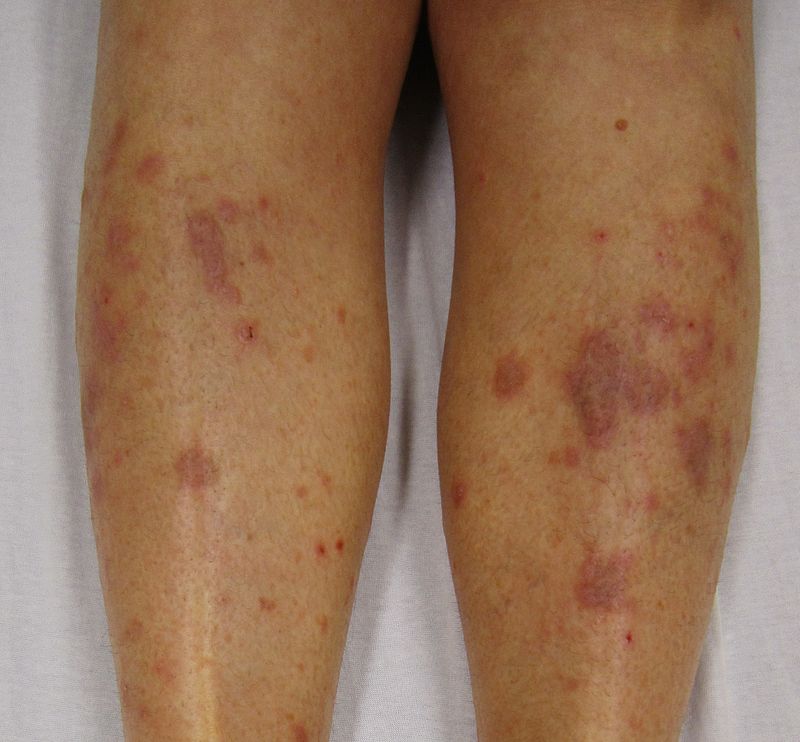
* Red ([[erythematous]]) patches scattered over the [[skin]] of the [[trunk]] and the [[extremities]] | * Red ([[erythematous]]) patches scattered over the [[skin]] of the [[trunk]] and the [[extremities]] | ||
| Line 85: | Line 85: | ||
* Recurrent [[lesions]] are usually less evenly scattered than psoriasis | * Recurrent [[lesions]] are usually less evenly scattered than psoriasis | ||
* Brownish red or orange-brown color | * Brownish red or orange-brown color | ||
* [[Lesions]] are capped by a single detachable opaque mica-like scale | * [[Lesions]] are capped by a single detachable, opaque, mica-like scale | ||
* Often leave [[Hypopigmented area|hypopigmented]] [[Macule|macules]] | * Often leave [[Hypopigmented area|hypopigmented]] [[Macule|macules]] | ||
| | | | ||
| Line 109: | Line 109: | ||
* Often appears after a skin injury, such as a [[burn]], [[abrasion]] (from friction), or [[insect bite]] | * Often appears after a skin injury, such as a [[burn]], [[abrasion]] (from friction), or [[insect bite]] | ||
* Lesions commonly relapse after occasional remission or may persist for long periods | * [[Lesions]] commonly relapse after occasional remission or may persist for long periods | ||
* [[Pruritis]] | * [[Pruritis]] | ||
| | | | ||
| Line 115: | Line 115: | ||
** Dry skin | ** Dry skin | ||
** Emotional stress | ** Emotional stress | ||
** Allergens(rubber chemicals, [[formaldehyde]], [[neomycin]], chrome, [[Mercury (element)|mercury]] and [[nickel]]) | ** Allergens (rubber chemicals, [[formaldehyde]], [[neomycin]], chrome, [[Mercury (element)|mercury]], and [[nickel]]) | ||
** [[Staphylococcus]] infection | ** [[Staphylococcus]] infection | ||
** Seasonal variation | ** Seasonal variation | ||
| Line 126: | Line 126: | ||
|[[Secondary syphilis]]<ref name="urlSTD Facts - Syphilis">{{cite web |url=https://www.cdc.gov/std/syphilis/stdfact-syphilis.htm |title=STD Facts - Syphilis |format= |work= |accessdate=}}</ref> | |[[Secondary syphilis]]<ref name="urlSTD Facts - Syphilis">{{cite web |url=https://www.cdc.gov/std/syphilis/stdfact-syphilis.htm |title=STD Facts - Syphilis |format= |work= |accessdate=}}</ref> | ||
| | | | ||
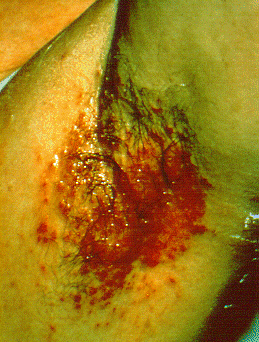
* Round coppery red | * Round, coppery, red colored [[lesions]] on palms and soles | ||
* [[Papule|Papules]] with collarette of scales | * [[Papule|Papules]] with collarette of scales | ||
| | | | ||
| Line 147: | Line 147: | ||
|[[Bowen’s disease]]<ref name="pmid28523295">{{cite journal |vauthors=Neagu TP, Ţigliş M, Botezatu D, Enache V, Cobilinschi CO, Vâlcea-Precup MS, GrinŢescu IM |title=Clinical, histological and therapeutic features of Bowen's disease |journal=Rom J Morphol Embryol |volume=58 |issue=1 |pages=33–40 |year=2017 |pmid=28523295 |doi= |url=}}</ref> | |[[Bowen’s disease]]<ref name="pmid28523295">{{cite journal |vauthors=Neagu TP, Ţigliş M, Botezatu D, Enache V, Cobilinschi CO, Vâlcea-Precup MS, GrinŢescu IM |title=Clinical, histological and therapeutic features of Bowen's disease |journal=Rom J Morphol Embryol |volume=58 |issue=1 |pages=33–40 |year=2017 |pmid=28523295 |doi= |url=}}</ref> | ||
| | | | ||
* [[Erythematous]] | * [[Erythematous]], small, scaly plaque, which enlarges over time in an erratic manner | ||
* Scale is usually yellow or white and it is easily detachable without producing any [[bleeding]] | * Scale is usually yellow or white and it is easily detachable without producing any [[bleeding]] | ||
* Well defined margins | * Well defined margins | ||
| Line 153: | Line 153: | ||
* [[Pruritis]] | * [[Pruritis]] | ||
* [[Pain]] | * [[Pain]] | ||
* Bleeding lesions | * Bleeding [[lesions]] | ||
| | | | ||
* Associated with:<ref name="pmid25201325">{{cite journal |vauthors=Murao K, Yoshioka R, Kubo Y |title=Human papillomavirus infection in Bowen disease: negative p53 expression, not p16(INK4a) overexpression, is correlated with human papillomavirus-associated Bowen disease |journal=J. Dermatol. |volume=41 |issue=10 |pages=878–84 |year=2014 |pmid=25201325 |doi=10.1111/1346-8138.12613 |url=}}</ref> | * Associated with:<ref name="pmid25201325">{{cite journal |vauthors=Murao K, Yoshioka R, Kubo Y |title=Human papillomavirus infection in Bowen disease: negative p53 expression, not p16(INK4a) overexpression, is correlated with human papillomavirus-associated Bowen disease |journal=J. Dermatol. |volume=41 |issue=10 |pages=878–84 |year=2014 |pmid=25201325 |doi=10.1111/1346-8138.12613 |url=}}</ref> | ||
| Line 179: | Line 179: | ||
** Antibiotics ([[Penicillin|penicillins]], [[sulfonamides]], [[tetracyclines]]) | ** Antibiotics ([[Penicillin|penicillins]], [[sulfonamides]], [[tetracyclines]]) | ||
** [[Carbamazepine]] | ** [[Carbamazepine]] | ||
** [[Calcium channel blocker|Calcium channel blockers]]([[Diltiazem]]) | ** [[Calcium channel blocker|Calcium channel blockers]] ([[Diltiazem]]) | ||
** [[Hydroxychloroquine]] | ** [[Hydroxychloroquine]] | ||
| | | | ||
| Line 187: | Line 187: | ||
| | | | ||
* Classically involves shin and ankles and is characterized by [[Hyperkeratosis|hyperkeratotic]] [[Plaque|plaques]] and [[Nodule (medicine)|nodules]] covered by a scale | * Classically involves shin and ankles and is characterized by [[Hyperkeratosis|hyperkeratotic]] [[Plaque|plaques]] and [[Nodule (medicine)|nodules]] covered by a scale | ||
* Lesions may transform into [[Hyperkeratosis|hyperkeratotic]] thickened elevated purplish or reddish [[Plaque|plaques]] and [[nodules]] | * [[Lesions]] may transform into [[Hyperkeratosis|hyperkeratotic]] thickened elevated purplish or reddish [[Plaque|plaques]] and [[nodules]] | ||
| | | | ||
* Chronic [[pruritis]] | * Chronic [[pruritis]] | ||
* Scaling | * Scaling | ||
* May be asymptomatic | * May be [[asymptomatic]] | ||
| | | | ||
* Associated with [[Hepatitis C virus]] infection<ref name="pmid19770446">{{cite journal |vauthors=Shengyuan L, Songpo Y, Wen W, Wenjing T, Haitao Z, Binyou W |title=Hepatitis C virus and lichen planus: a reciprocal association determined by a meta-analysis |journal=Arch Dermatol |volume=145 |issue=9 |pages=1040–7 |year=2009 |pmid=19770446 |doi=10.1001/archdermatol.2009.200 |url=}}</ref> | * Associated with [[Hepatitis C virus]] infection<ref name="pmid19770446">{{cite journal |vauthors=Shengyuan L, Songpo Y, Wen W, Wenjing T, Haitao Z, Binyou W |title=Hepatitis C virus and lichen planus: a reciprocal association determined by a meta-analysis |journal=Arch Dermatol |volume=145 |issue=9 |pages=1040–7 |year=2009 |pmid=19770446 |doi=10.1001/archdermatol.2009.200 |url=}}</ref> | ||
| Line 203: | Line 203: | ||
| | | | ||
* [[Pruritis]] | * [[Pruritis]] | ||
* May be asymptomatic | * May[[ be asymptomatic]] | ||
| | | | ||
* Associated with: | * Associated with: | ||
** [[Monoclonal gammopathy]], usually an IgA paraproteinemia<ref name="pmid3056995">{{cite journal |vauthors=Kasha EE, Epinette WW |title=Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) in association with a monoclonal IgA gammopathy: a report and review of the literature |journal=J. Am. Acad. Dermatol. |volume=19 |issue=5 Pt 1 |pages=854–8 |year=1988 |pmid=3056995 |doi= |url=}}</ref> | ** [[Monoclonal gammopathy]], usually an [[IgA]] paraproteinemia<ref name="pmid3056995">{{cite journal |vauthors=Kasha EE, Epinette WW |title=Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) in association with a monoclonal IgA gammopathy: a report and review of the literature |journal=J. Am. Acad. Dermatol. |volume=19 |issue=5 Pt 1 |pages=854–8 |year=1988 |pmid=3056995 |doi= |url=}}</ref> | ||
** [[Crohn's disease]]<ref name="pmid1357895">{{cite journal |vauthors=Delaporte E, Colombel JF, Nguyen-Mailfer C, Piette F, Cortot A, Bergoend H |title=Subcorneal pustular dermatosis in a patient with Crohn's disease |journal=Acta Derm. Venereol. |volume=72 |issue=4 |pages=301–2 |year=1992 |pmid=1357895 |doi= |url=}}</ref> | ** [[Crohn's disease]]<ref name="pmid1357895">{{cite journal |vauthors=Delaporte E, Colombel JF, Nguyen-Mailfer C, Piette F, Cortot A, Bergoend H |title=Subcorneal pustular dermatosis in a patient with Crohn's disease |journal=Acta Derm. Venereol. |volume=72 |issue=4 |pages=301–2 |year=1992 |pmid=1357895 |doi= |url=}}</ref> | ||
** [[Osteomyelitis]] | ** [[Osteomyelitis]] | ||
| Line 215: | Line 215: | ||
|[[Parapsoriasis|Small plaque parapsoriasis]]<ref name="pmid7026622">{{cite journal |vauthors=Lambert WC, Everett MA |title=The nosology of parapsoriasis |journal=J. Am. Acad. Dermatol. |volume=5 |issue=4 |pages=373–95 |year=1981 |pmid=7026622 |doi= |url=}}</ref> | |[[Parapsoriasis|Small plaque parapsoriasis]]<ref name="pmid7026622">{{cite journal |vauthors=Lambert WC, Everett MA |title=The nosology of parapsoriasis |journal=J. Am. Acad. Dermatol. |volume=5 |issue=4 |pages=373–95 |year=1981 |pmid=7026622 |doi= |url=}}</ref> | ||
| | | | ||
* [[Erythematous]] [[plaques]] which are covered with fine scale | * [[Erythematous]] [[plaques]] which are covered with fine scale | ||
* May present with elongated, finger-like patches symmetrically distributed on the flanks, also known as digitate dermatosis | * May present with elongated, finger-like patches symmetrically distributed on the flanks, also known as digitate dermatosis | ||
| | | | ||
| Line 228: | Line 228: | ||
|[[Intertrigo]]<ref name="pmid16156342">{{cite journal |vauthors=Janniger CK, Schwartz RA, Szepietowski JC, Reich A |title=Intertrigo and common secondary skin infections |journal=Am Fam Physician |volume=72 |issue=5 |pages=833–8 |year=2005 |pmid=16156342 |doi= |url=}}</ref> | |[[Intertrigo]]<ref name="pmid16156342">{{cite journal |vauthors=Janniger CK, Schwartz RA, Szepietowski JC, Reich A |title=Intertrigo and common secondary skin infections |journal=Am Fam Physician |volume=72 |issue=5 |pages=833–8 |year=2005 |pmid=16156342 |doi= |url=}}</ref> | ||
| | | | ||
* Red and fleshy looking lesion in [[skin]] folds | * Red and fleshy looking [[lesion]] in [[skin]] folds | ||
* [[Itching]] | * [[Itching]] | ||
* | * Oozing | ||
* May be sore | * May be sore | ||
| | | | ||
| Line 266: | Line 266: | ||
| | | | ||
* [[Pruritis]] | * [[Pruritis]] | ||
* KOH preparation of the lesions confirms [[fungal infection]] | * [[KOH]] preparation of the [[lesions]] confirms [[fungal infection]] | ||
| | | | ||
* Associated with: | * Associated with: | ||
Revision as of 15:29, 3 August 2017
|
Psoriasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Differentiating psoriasis from other diseases On the Web |
|
American Roentgen Ray Society Images of Differentiating psoriasis from other diseases |
|
Risk calculators and risk factors for Differentiating psoriasis from other diseases |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Syed Hassan A. Kazmi BSc, MD [2]
Overview
Psoriasis must be differentiated from other diseases that cause erythematous, scaly rash such as cutaneous T cell lymphoma/mycosis fungoides, pityriasis rosea, pityriasis rubra pilaris, pityriasis lichenoides chronica, nummular dermatitis, secondary syphilis, Bowen’s disease, exanthematous pustulosis, hypertrophic lichen planus, Sneddon–Wilkinson disease, small plaque parapsoriasis, intertrigo, Langerhans cell histiocytosis, dyshidrotic dermatitis, tinea manuum/pedum/capitis, and seborrheic dermatitis.
Differentiating psoriasis from other diseases
Differential diagnosis of psoriasis
- Psoriasis must be differentiated from other diseases causing papulosquamous or erythematosquamous rash, especially when the psoriatic lesions are localized in particular sites as palms, soles, scalp, body folds, penis, and nails.
- The differential diagnosis of psoriasis includes:
- Cutaneous T cell lymphoma/mycosis fungoides
- Pityriasis rosea
- Pityriasis rubra pilaris
- Pityriasis lichenoides chronica
- Nummular dermatitis
- Secondary syphilis
- Bowen’s disease
- Exanthematous pustulosis
- Hypertrophic lichen planus
- Sneddon–Wilkinson disease
- Small plaque parapsoriasis
- Intertrigo
- Langerhans cell histiocytosis
- Dyshidrotic dermatitis
- Tinea manuum/pedum/capitis
- Seborrheic dermatitis
| Disease | Rash Characteristics | Signs and Symptoms | Associated Conditions | Images |
|---|---|---|---|---|
| Cutaneous T cell lymphoma/Mycosis fungoides[1] |
|
|
||
| Pityriasis rosea[2] |
|
|
||
| Pityriasis lichenoides chronica |
|
|
||
| Nummular dermatitis[5] |
|
|
|
|
| Secondary syphilis[6] |
|
|||
| Bowen’s disease[7] |
|
|
||
| Exanthematous pustulosis[9] |
|
|
||
| Hypertrophic lichen planus[11] |
|
|
|
|
| Sneddon–Wilkinson disease[13] |
|
|||
| Small plaque parapsoriasis[17] |
|
|
|
|
| Intertrigo[19] |
|
|
||
| Langerhans cell histiocytosis[20] |
|
|
|
|
| Tinea manuum/pedum/capitis[24] |
|
|
|
|
| Seborrheic dermatitis |
|
|
Differential diagnosis of psoriatic arthritis
Psoriatic arthritis must be differentiated from other diseases causing oligo/polyarthritis of the peripheral skeleton or arthritis of the axial skeleton, for example:
- Rheumatoid arthritis
- Seronegative arthropathies:
- Ankylosing spondylitis
- Inflammatory bowel disease associated arthritis (enteropathic arthritis)
- Reactive arthritis (Reiter's syndrome)
| Arthritis Type | Clinical Features | Body Distribution | Key Signs | Laboratory Abnormalities | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Psoriasis | Symmetric joint involvement | Asymmetric joint involvement | Enthesopathy | Dactylitis | Nail Dystrophy | Human immunodeficiency virus association | Upper extremity-hands | Lower extremity | Sacroiliac joints | Spine | Osteoporosis | Joint Space | Ankylosis | Periostitis | Soft tissue swelling | ESR | Rheumatoid factor (RF) | HLA-B27 | |
| Psoriatic arthritis | + | + | ++ | + | + | + | + | +++ (DIP/PIP) | +++ | ++ (Unilateral) | ++ | - | ++ (Widening) | ++ | +++ (Fluffy) | ++ | + | - | 30-75% |
| Rheumatoid arthritis | - | ++ | + | - | - | - | - | +++ | +++ | + (Unilateral) | ++(Cervical) | +++ | +++ (Narrowing) | + | + (Linear) | +++ | +++ | +++ | 6-8% |
| Ankylosing spondylitis | - | +++ | - | + | - | - | - | - | + | +++ (Bilateral) | +++ | +++ | ++ (Narrowing) | +++ | +++ (Fluffy) | + | +++ | - | 90% |
| Reactive arthritis (Reiter's syndrome) | - | +++ | - | + | - | - | - | - | +++ | ++ (Unilateral) | + | + | + (Narrowing) | - | +++ (Fluffy) | ++ | ++ | - | 75% |
Key:+ : Infrequently present, ++ : Frequently present, +++ : Always present, - : Absent
References
- ↑ "Mycosis Fungoides and the Sézary Syndrome Treatment (PDQ®)—Patient Version - National Cancer Institute".
- ↑ Mahajan K, Relhan V, Relhan AK, Garg VK (2016). "Pityriasis Rosea: An Update on Etiopathogenesis and Management of Difficult Aspects". Indian J Dermatol. 61 (4): 375–84. doi:10.4103/0019-5154.185699. PMC 4966395. PMID 27512182.
- ↑ Prantsidis A, Rigopoulos D, Papatheodorou G, Menounos P, Gregoriou S, Alexiou-Mousatou I, Katsambas A (2009). "Detection of human herpesvirus 8 in the skin of patients with pityriasis rosea". Acta Derm. Venereol. 89 (6): 604–6. doi:10.2340/00015555-0703. PMID 19997691.
- ↑ Smith KJ, Nelson A, Skelton H, Yeager J, Wagner KF (1997). "Pityriasis lichenoides et varioliformis acuta in HIV-1+ patients: a marker of early stage disease. The Military Medical Consortium for the Advancement of Retroviral Research (MMCARR)". Int. J. Dermatol. 36 (2): 104–9. PMID 9109005.
- ↑ Jiamton S, Tangjaturonrusamee C, Kulthanan K (2013). "Clinical features and aggravating factors in nummular eczema in Thais". Asian Pac. J. Allergy Immunol. 31 (1): 36–42. PMID 23517392.
- ↑ "STD Facts - Syphilis".
- ↑ Neagu TP, Ţigliş M, Botezatu D, Enache V, Cobilinschi CO, Vâlcea-Precup MS, GrinŢescu IM (2017). "Clinical, histological and therapeutic features of Bowen's disease". Rom J Morphol Embryol. 58 (1): 33–40. PMID 28523295.
- ↑ Murao K, Yoshioka R, Kubo Y (2014). "Human papillomavirus infection in Bowen disease: negative p53 expression, not p16(INK4a) overexpression, is correlated with human papillomavirus-associated Bowen disease". J. Dermatol. 41 (10): 878–84. doi:10.1111/1346-8138.12613. PMID 25201325.
- ↑ Szatkowski J, Schwartz RA (2015). "Acute generalized exanthematous pustulosis (AGEP): A review and update". J. Am. Acad. Dermatol. 73 (5): 843–8. doi:10.1016/j.jaad.2015.07.017. PMID 26354880.
- ↑ Schmid S, Kuechler PC, Britschgi M, Steiner UC, Yawalkar N, Limat A, Baltensperger K, Braathen L, Pichler WJ (2002). "Acute generalized exanthematous pustulosis: role of cytotoxic T cells in pustule formation". Am. J. Pathol. 161 (6): 2079–86. doi:10.1016/S0002-9440(10)64486-0. PMC 1850901. PMID 12466124.
- ↑ Ankad BS, Beergouder SL (2016). "Hypertrophic lichen planus versus prurigo nodularis: a dermoscopic perspective". Dermatol Pract Concept. 6 (2): 9–15. doi:10.5826/dpc.0602a03. PMC 4866621. PMID 27222766.
- ↑ Shengyuan L, Songpo Y, Wen W, Wenjing T, Haitao Z, Binyou W (2009). "Hepatitis C virus and lichen planus: a reciprocal association determined by a meta-analysis". Arch Dermatol. 145 (9): 1040–7. doi:10.1001/archdermatol.2009.200. PMID 19770446.
- ↑ Lutz ME, Daoud MS, McEvoy MT, Gibson LE (1998). "Subcorneal pustular dermatosis: a clinical study of ten patients". Cutis. 61 (4): 203–8. PMID 9564592.
- ↑ Kasha EE, Epinette WW (1988). "Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) in association with a monoclonal IgA gammopathy: a report and review of the literature". J. Am. Acad. Dermatol. 19 (5 Pt 1): 854–8. PMID 3056995.
- ↑ Delaporte E, Colombel JF, Nguyen-Mailfer C, Piette F, Cortot A, Bergoend H (1992). "Subcorneal pustular dermatosis in a patient with Crohn's disease". Acta Derm. Venereol. 72 (4): 301–2. PMID 1357895.
- ↑ Sauder MB, Glassman SJ (2013). "Palmoplantar subcorneal pustular dermatosis following adalimumab therapy for rheumatoid arthritis". Int. J. Dermatol. 52 (5): 624–8. doi:10.1111/j.1365-4632.2012.05707.x. PMID 23489057.
- ↑ Lambert WC, Everett MA (1981). "The nosology of parapsoriasis". J. Am. Acad. Dermatol. 5 (4): 373–95. PMID 7026622.
- ↑ Väkevä L, Sarna S, Vaalasti A, Pukkala E, Kariniemi AL, Ranki A (2005). "A retrospective study of the probability of the evolution of parapsoriasis en plaques into mycosis fungoides". Acta Derm. Venereol. 85 (4): 318–23. doi:10.1080/00015550510030087. PMID 16191852.
- ↑ Janniger CK, Schwartz RA, Szepietowski JC, Reich A (2005). "Intertrigo and common secondary skin infections". Am Fam Physician. 72 (5): 833–8. PMID 16156342.
- ↑ Satter EK, High WA (2008). "Langerhans cell histiocytosis: a review of the current recommendations of the Histiocyte Society". Pediatr Dermatol. 25 (3): 291–5. doi:10.1111/j.1525-1470.2008.00669.x. PMID 18577030.
- ↑ Stull MA, Kransdorf MJ, Devaney KO (1992). "Langerhans cell histiocytosis of bone". Radiographics. 12 (4): 801–23. doi:10.1148/radiographics.12.4.1636041. PMID 1636041.
- ↑ Sholl LM, Hornick JL, Pinkus JL, Pinkus GS, Padera RF (2007). "Immunohistochemical analysis of langerin in langerhans cell histiocytosis and pulmonary inflammatory and infectious diseases". Am. J. Surg. Pathol. 31 (6): 947–52. doi:10.1097/01.pas.0000249443.82971.bb. PMID 17527085.
- ↑ Grois N, Pötschger U, Prosch H, Minkov M, Arico M, Braier J, Henter JI, Janka-Schaub G, Ladisch S, Ritter J, Steiner M, Unger E, Gadner H (2006). "Risk factors for diabetes insipidus in langerhans cell histiocytosis". Pediatr Blood Cancer. 46 (2): 228–33. doi:10.1002/pbc.20425. PMID 16047354.
- ↑ Al Hasan M, Fitzgerald SM, Saoudian M, Krishnaswamy G (2004). "Dermatology for the practicing allergist: Tinea pedis and its complications". Clin Mol Allergy. 2 (1): 5. doi:10.1186/1476-7961-2-5. PMC 419368. PMID 15050029.
- ↑ Schwartz RA, Janusz CA, Janniger CK (2006). "Seborrheic dermatitis: an overview". Am Fam Physician. 74 (1): 125–30. PMID 16848386.
- ↑ Misery L, Touboul S, Vinçot C, Dutray S, Rolland-Jacob G, Consoli SG, Farcet Y, Feton-Danou N, Cardinaud F, Callot V, De La Chapelle C, Pomey-Rey D, Consoli SM (2007). "[Stress and seborrheic dermatitis]". Ann Dermatol Venereol (in French). 134 (11): 833–7. PMID 18033062.