Differentiating psoriasis from other diseases: Difference between revisions
No edit summary |
|||
| (26 intermediate revisions by 5 users not shown) | |||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
Psoriasis must be differentiated from other diseases that cause [[erythematous]], scaly [[Rash erythematous|rash]] such as [[cutaneous T cell lymphoma]]/[[mycosis fungoides]], [[pityriasis rosea]], [[pityriasis rubra pilaris]], [[pityriasis lichenoides chronica]], [[nummular dermatitis]], [[secondary syphilis]], [[Bowen’s disease]], [[exanthematous pustulosis]], [[Lichen planus|hypertrophic lichen planus]], Sneddon–Wilkinson disease, [[Parapsoriasis|small plaque parapsoriasis]], [[intertrigo]], [[Langerhans cell histiocytosis]], [[dyshidrotic dermatitis]], [[tinea manuum]]/pedum/[[Tinea capitis|capitis]] and [[seborrheic dermatitis]]. | Psoriasis must be differentiated from other diseases that cause an [[erythematous]], scaly [[Rash erythematous|rash]] such as [[cutaneous T cell lymphoma]]/[[mycosis fungoides]], [[pityriasis rosea]], [[pityriasis rubra pilaris]], [[pityriasis lichenoides chronica]], [[nummular dermatitis]], [[secondary syphilis]], [[Bowen’s disease]], [[exanthematous pustulosis]], [[Lichen planus|hypertrophic lichen planus]], Sneddon–Wilkinson disease, [[Parapsoriasis|small plaque parapsoriasis]], [[intertrigo]], [[Langerhans cell histiocytosis]], [[dyshidrotic dermatitis]], [[tinea manuum]]/pedum/[[Tinea capitis|capitis]], and [[seborrheic dermatitis]]. | ||
==Differentiating | ==Differentiating psoriasis from other diseases== | ||
=== Differential diagnosis of psoriasis === | === Differential diagnosis of psoriasis === | ||
*Psoriasis must be differentiated from other diseases | *Psoriasis must be differentiated from other diseases that cause [[Papulosquamous disorder|papulosquamous]] or [[Erythematous rash|erythematosquamous rash]], especially when the psoriatic [[lesions]] are localized in such sites as the [[Palms of the hands|palms]], [[soles]], [[scalp]], body folds, [[penis]], and [[Nail (anatomy)|nails]]. The differential diagnosis of psoriasis includes: | ||
{| class="wikitable" | {| class="wikitable" | ||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Disease | ! align="center" style="background:#4479BA; color: #FFFFFF;" + |Disease | ||
| Line 34: | Line 17: | ||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Images | ! align="center" style="background:#4479BA; color: #FFFFFF;" + |Images | ||
|- | |- | ||
|[[Cutaneous T cell lymphoma]]/[[Mycosis fungoides]]<ref name="urlMycosis Fungoides and the Sézary Syndrome Treatment (PDQ®)—Patient Version - National Cancer Institute">{{cite web |url=https://www.cancer.gov/types/lymphoma/patient/mycosis-fungoides-treatment-pdq |title=Mycosis Fungoides and the Sézary Syndrome Treatment (PDQ®)—Patient Version - National Cancer Institute |format= |work= |accessdate=}}</ref> | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Cutaneous T cell lymphoma]]/[[Mycosis fungoides]]<ref name="urlMycosis Fungoides and the Sézary Syndrome Treatment (PDQ®)—Patient Version - National Cancer Institute">{{cite web |url=https://www.cancer.gov/types/lymphoma/patient/mycosis-fungoides-treatment-pdq |title=Mycosis Fungoides and the Sézary Syndrome Treatment (PDQ®)—Patient Version - National Cancer Institute |format= |work= |accessdate=}}</ref> | ||
| | | | ||
* '''Premycotic phase:''' A scaly, red [[rash]] in areas of the [[body]] that usually are not exposed to the sun. This rash does not cause symptoms and may last for months or years. | * '''Premycotic phase:''' A scaly, red [[rash]] in areas of the [[body]] that usually are not exposed to the sun. This rash does not cause symptoms and may last for months or years. | ||
* '''Patch phase:''' Thin, | * '''Patch phase:''' Thin, [[erythematous]], [[eczema]]-like rash. | ||
* '''[[Plaque]] phase:''' Small raised [[Bumps on skin|bumps]] ([[Papule|papules]]) or | * '''[[Plaque]] phase:''' Small raised [[Bumps on skin|bumps]] ([[Papule|papules]]) or hardened [[lesions]] on the skin, which may be [[erythematous]]. | ||
* '''[[Tumor]] phase:''' Tumors form on the [[skin]]. | * '''[[Tumor]] phase:''' Tumors form on the [[skin]]. [[Infection]] secondary to [[Ulcer|ulcers]]. | ||
| | | | ||
* [[Epidermis (skin)|Epidermal]] [[atrophy]] or poikiloderma | * [[Epidermis (skin)|Epidermal]] [[atrophy]] or poikiloderma | ||
* Generalized [[itching]] ([[pruritus]]) | * Generalized [[itching]] ([[pruritus]]) | ||
* [[Pain]] in the affected area of the skin | * [[Pain]] in the affected area of the skin | ||
* [[Insomnia]] | * [[Insomnia]] | ||
* Red ([[erythematous]]) patches scattered over the [[skin]] of the [[trunk]] and the [[extremities]] | * Red ([[erythematous]]) patches scattered over the [[skin]] of the [[trunk]] and the [[extremities]] | ||
* Tumor-like lobulated outgrowths form on the skin in the latter | * Tumor-like lobulated outgrowths form on the skin in the latter phase of the disease | ||
* [[Weight loss]] | * [[Weight loss]] | ||
* [[Lymphadenopathy]] | * [[Lymphadenopathy]] | ||
* [[Malaise]] and [[fatigue]] | * [[Malaise]] and [[fatigue]] | ||
* [[Anemia]] | * [[Anemia]] | ||
* May progress to [[Sezary syndrome]] ( | * May progress to [[Sezary syndrome]] (skin involvement plus hematogenous dissemination) | ||
| | | | ||
* [[Sezary syndrome]] | * [[Sezary syndrome]] | ||
| | | | ||
[[Image:Mycosis_fungoides.JPG|200px]] | [[Image:Mycosis_fungoides.JPG|200px|courtesy of wikipedia.org]] | ||
|- | |- | ||
|[[Pityriasis rosea]]<ref name="pmid27512182">{{cite journal |vauthors=Mahajan K, Relhan V, Relhan AK, Garg VK |title=Pityriasis Rosea: An Update on Etiopathogenesis and Management of Difficult Aspects |journal=Indian J Dermatol |volume=61 |issue=4 |pages=375–84 |year=2016 |pmid=27512182 |pmc=4966395 |doi=10.4103/0019-5154.185699 |url=}}</ref> | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Pityriasis rosea]]<ref name="pmid27512182">{{cite journal |vauthors=Mahajan K, Relhan V, Relhan AK, Garg VK |title=Pityriasis Rosea: An Update on Etiopathogenesis and Management of Difficult Aspects |journal=Indian J Dermatol |volume=61 |issue=4 |pages=375–84 |year=2016 |pmid=27512182 |pmc=4966395 |doi=10.4103/0019-5154.185699 |url=}}</ref> | ||
| | | | ||
* Pink or salmon in | * Pink or salmon in color, which may be scaly; referred to as "herald patch" | ||
* Oval | * Oval shape | ||
* Long axis oriented along the cleavage lines | * Long axis oriented along the cleavage lines | ||
* Distributed on the [[trunk]] and [[proximal extremities]] | * Distributed on the [[trunk]] and [[proximal extremities]] | ||
* Squamous marginal collarette and a “fir-tree” or “Christmas tree” distribution on | * Squamous marginal collarette and a “fir-tree” or “Christmas tree” distribution on posterior trunk | ||
* | * Secondary to [[viral infection]]<nowiki/>s | ||
* Resolves spontaneously after 6-8 weeks | * Resolves spontaneously after 6-8 weeks | ||
| | | | ||
| Line 79: | Line 62: | ||
** [[HHV-8]] | ** [[HHV-8]] | ||
| | | | ||
[[Image:Pityriasisrosea.png|200px]] | [[Image:Pityriasisrosea.png|200px|courtesy of https://commons.wikimedia.org]] | ||
|- | |- | ||
|[[Pityriasis lichenoides chronica]] | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Pityriasis lichenoides chronica]] | ||
| | | | ||
* Recurrent [[lesions]] are usually less evenly scattered than psoriasis | * Recurrent [[lesions]] are usually less evenly scattered than in cases of psoriasis | ||
* Brownish red or orange-brown color | * Brownish red or orange-brown in color | ||
* [[Lesions]] are capped by a single detachable opaque mica-like scale | * [[Lesions]] are capped by a single detachable, opaque, mica-like scale | ||
* Often leave [[Hypopigmented area|hypopigmented]] [[Macule|macules]] | * Often leave [[Hypopigmented area|hypopigmented]] [[Macule|macules]] | ||
| | | | ||
| Line 91: | Line 74: | ||
* [[Malaise]] | * [[Malaise]] | ||
* [[Myalgias]] | * [[Myalgias]] | ||
* | * [[Paraesthesia]] | ||
* [[Pruritis]] | * [[Pruritis|Pruritus]] | ||
| | | | ||
* Infection by any of the following:<ref name="pmid9109005">{{cite journal |vauthors=Smith KJ, Nelson A, Skelton H, Yeager J, Wagner KF |title=Pityriasis lichenoides et varioliformis acuta in HIV-1+ patients: a marker of early stage disease. The Military Medical Consortium for the Advancement of Retroviral Research (MMCARR) |journal=Int. J. Dermatol. |volume=36 |issue=2 |pages=104–9 |year=1997 |pmid=9109005 |doi= |url=}}</ref> | * Infection by any of the following:<ref name="pmid9109005">{{cite journal |vauthors=Smith KJ, Nelson A, Skelton H, Yeager J, Wagner KF |title=Pityriasis lichenoides et varioliformis acuta in HIV-1+ patients: a marker of early stage disease. The Military Medical Consortium for the Advancement of Retroviral Research (MMCARR) |journal=Int. J. Dermatol. |volume=36 |issue=2 |pages=104–9 |year=1997 |pmid=9109005 |doi= |url=}}</ref> | ||
| Line 99: | Line 82: | ||
** [[Human Immunodeficiency Virus (HIV)|Human immunodeficiency virus]] (HIV) | ** [[Human Immunodeficiency Virus (HIV)|Human immunodeficiency virus]] (HIV) | ||
| | | | ||
[[Image:PLEVA2.jpg|200px|courtesy http://www.regionalderm.com]] | [[Image:PLEVA2.jpg|200px|courtesy of http://www.regionalderm.com]] | ||
|- | |- | ||
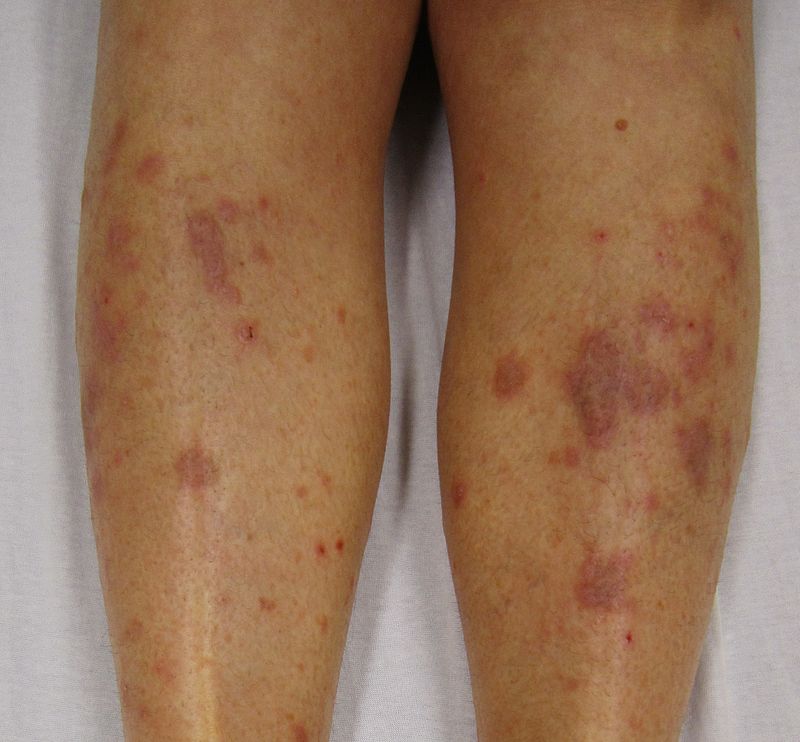
|[[Nummular dermatitis]]<ref name="pmid23517392">{{cite journal |vauthors=Jiamton S, Tangjaturonrusamee C, Kulthanan K |title=Clinical features and aggravating factors in nummular eczema in Thais |journal=Asian Pac. J. Allergy Immunol. |volume=31 |issue=1 |pages=36–42 |year=2013 |pmid=23517392 |doi= |url=}}</ref> | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Nummular dermatitis]]<ref name="pmid23517392">{{cite journal |vauthors=Jiamton S, Tangjaturonrusamee C, Kulthanan K |title=Clinical features and aggravating factors in nummular eczema in Thais |journal=Asian Pac. J. Allergy Immunol. |volume=31 |issue=1 |pages=36–42 |year=2013 |pmid=23517392 |doi= |url=}}</ref> | ||
| | | | ||
* Multiple coin-shaped [[Eczematous Scaling|eczematous]] [[lesions]] | * Multiple coin-shaped [[Eczematous Scaling|eczematous]] [[lesions]] | ||
| Line 109: | Line 92: | ||
* Often appears after a skin injury, such as a [[burn]], [[abrasion]] (from friction), or [[insect bite]] | * Often appears after a skin injury, such as a [[burn]], [[abrasion]] (from friction), or [[insect bite]] | ||
* Lesions commonly relapse after occasional remission or may persist for long periods | * [[Lesions]] commonly relapse after occasional remission or may persist for long periods | ||
* [[Pruritis]] | * [[Pruritis|Pruritus]] | ||
| | | | ||
* Associated with: | * Associated with: | ||
** Dry skin | ** Dry skin | ||
** Emotional stress | ** Emotional stress | ||
** Allergens(rubber chemicals, [[formaldehyde]], [[neomycin]], chrome, [[Mercury (element)|mercury]] and [[nickel]]) | ** [[Allergens]] (rubber chemicals, [[formaldehyde]], [[neomycin]], chrome, [[Mercury (element)|mercury]], and [[nickel]]) | ||
** [[Staphylococcus]] infection | ** [[Staphylococcus]] infection | ||
** Seasonal variation | ** Seasonal variation | ||
| Line 122: | Line 105: | ||
** [[Atopy]] | ** [[Atopy]] | ||
| | | | ||
[[Image: | [[Image:Nummular dermatitis dry.jpg|200px|courtesy of your-doctor.net dermatology atlas]] | ||
|- | |- | ||
|[[Secondary syphilis]]<ref name="urlSTD Facts - Syphilis">{{cite web |url=https://www.cdc.gov/std/syphilis/stdfact-syphilis.htm |title=STD Facts - Syphilis |format= |work= |accessdate=}}</ref> | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Secondary syphilis]]<ref name="urlSTD Facts - Syphilis">{{cite web |url=https://www.cdc.gov/std/syphilis/stdfact-syphilis.htm |title=STD Facts - Syphilis |format= |work= |accessdate=}}</ref> | ||
| | | | ||
* Round coppery red | * Round, coppery, red colored [[lesions]] on palms and soles | ||
* [[Papule|Papules]] with collarette of scales | * [[Papule|Papules]] with collarette of scales | ||
| | | | ||
| Line 133: | Line 116: | ||
* [[Sore throat]] | * [[Sore throat]] | ||
* [[Hair loss|Patchy hair loss]] | * [[Hair loss|Patchy hair loss]] | ||
* [[Headaches]] | * [[Headaches|Headache]] | ||
* [[Weight loss]] | * [[Weight loss]] | ||
* [[Myalgia]] | * [[Myalgia]] | ||
| Line 143: | Line 126: | ||
** Positive [[Venereal disease research laboratory (VDRL) test|VDRL]] test | ** Positive [[Venereal disease research laboratory (VDRL) test|VDRL]] test | ||
| | | | ||
[[Image:Secondary_Syphilis.jpg|200px]] | [[Image:Secondary_Syphilis.jpg|200px|courtesy of wikipedia.org]] | ||
|- | |- | ||
|[[Bowen’s disease]]<ref name="pmid28523295">{{cite journal |vauthors=Neagu TP, Ţigliş M, Botezatu D, Enache V, Cobilinschi CO, Vâlcea-Precup MS, GrinŢescu IM |title=Clinical, histological and therapeutic features of Bowen's disease |journal=Rom J Morphol Embryol |volume=58 |issue=1 |pages=33–40 |year=2017 |pmid=28523295 |doi= |url=}}</ref> | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Bowen’s disease]]<ref name="pmid28523295">{{cite journal |vauthors=Neagu TP, Ţigliş M, Botezatu D, Enache V, Cobilinschi CO, Vâlcea-Precup MS, GrinŢescu IM |title=Clinical, histological and therapeutic features of Bowen's disease |journal=Rom J Morphol Embryol |volume=58 |issue=1 |pages=33–40 |year=2017 |pmid=28523295 |doi= |url=}}</ref> | ||
| | | | ||
* [[Erythematous]] | * [[Erythematous]], small, scaly plaque, which enlarges erratically over time | ||
* Scale is usually yellow or white and it is easily detachable without | * Scale is usually yellow or white and it is easily detachable without any [[bleeding]] | ||
* Well defined margins | * Well-defined margins | ||
| | | | ||
* [[Pruritis]] | * [[Pruritis|Pruritus]] | ||
* [[Pain]] | * [[Pain]] | ||
* Bleeding lesions | * Bleeding [[lesions]] | ||
| | | | ||
* Associated with:<ref name="pmid25201325">{{cite journal |vauthors=Murao K, Yoshioka R, Kubo Y |title=Human papillomavirus infection in Bowen disease: negative p53 expression, not p16(INK4a) overexpression, is correlated with human papillomavirus-associated Bowen disease |journal=J. Dermatol. |volume=41 |issue=10 |pages=878–84 |year=2014 |pmid=25201325 |doi=10.1111/1346-8138.12613 |url=}}</ref> | * Associated with:<ref name="pmid25201325">{{cite journal |vauthors=Murao K, Yoshioka R, Kubo Y |title=Human papillomavirus infection in Bowen disease: negative p53 expression, not p16(INK4a) overexpression, is correlated with human papillomavirus-associated Bowen disease |journal=J. Dermatol. |volume=41 |issue=10 |pages=878–84 |year=2014 |pmid=25201325 |doi=10.1111/1346-8138.12613 |url=}}</ref> | ||
| Line 166: | Line 149: | ||
** [[Sjögren's syndrome|Sjögren’s syndrome]] | ** [[Sjögren's syndrome|Sjögren’s syndrome]] | ||
| | | | ||
[[Image:Bowen.jpg|200px]] | [[Image:Bowen.jpg|200px|courtesy of wikipedia.org]] | ||
|- | |- | ||
|[[Exanthematous pustulosis]]<ref name="pmid26354880">{{cite journal |vauthors=Szatkowski J, Schwartz RA |title=Acute generalized exanthematous pustulosis (AGEP): A review and update |journal=J. Am. Acad. Dermatol. |volume=73 |issue=5 |pages=843–8 |year=2015 |pmid=26354880 |doi=10.1016/j.jaad.2015.07.017 |url=}}</ref> | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Exanthematous pustulosis]]<ref name="pmid26354880">{{cite journal |vauthors=Szatkowski J, Schwartz RA |title=Acute generalized exanthematous pustulosis (AGEP): A review and update |journal=J. Am. Acad. Dermatol. |volume=73 |issue=5 |pages=843–8 |year=2015 |pmid=26354880 |doi=10.1016/j.jaad.2015.07.017 |url=}}</ref> | ||
| | | | ||
* Numerous small, primarily non-follicular, sterile [[pustules]], arising within large areas of [[Edema|edematous]] [[erythema]] | * Numerous small, primarily non-follicular, sterile [[pustules]], arising within large areas of [[Edema|edematous]] [[erythema]] | ||
| Line 177: | Line 160: | ||
| | | | ||
* Associated with:<ref name="pmid12466124">{{cite journal |vauthors=Schmid S, Kuechler PC, Britschgi M, Steiner UC, Yawalkar N, Limat A, Baltensperger K, Braathen L, Pichler WJ |title=Acute generalized exanthematous pustulosis: role of cytotoxic T cells in pustule formation |journal=Am. J. Pathol. |volume=161 |issue=6 |pages=2079–86 |year=2002 |pmid=12466124 |pmc=1850901 |doi=10.1016/S0002-9440(10)64486-0 |url=}}</ref> | * Associated with:<ref name="pmid12466124">{{cite journal |vauthors=Schmid S, Kuechler PC, Britschgi M, Steiner UC, Yawalkar N, Limat A, Baltensperger K, Braathen L, Pichler WJ |title=Acute generalized exanthematous pustulosis: role of cytotoxic T cells in pustule formation |journal=Am. J. Pathol. |volume=161 |issue=6 |pages=2079–86 |year=2002 |pmid=12466124 |pmc=1850901 |doi=10.1016/S0002-9440(10)64486-0 |url=}}</ref> | ||
** Antibiotics ([[Penicillin|penicillins]], [[sulfonamides]], [[tetracyclines]]) | ** [[Antibiotics]] ([[Penicillin|penicillins]], [[sulfonamides]], [[tetracyclines]]) | ||
** [[Carbamazepine]] | ** [[Carbamazepine]] | ||
** [[Calcium channel blocker|Calcium channel blockers]]([[Diltiazem]]) | ** [[Calcium channel blocker|Calcium channel blockers]] ([[Diltiazem]]) | ||
** [[Hydroxychloroquine]] | ** [[Hydroxychloroquine]] | ||
| | | | ||
[[Image:Acute_generalized_exanthematous_pustulosis.jpg|200px]] | [[Image:Acute_generalized_exanthematous_pustulosis.jpg|200px|commons.wikimedia.org]] | ||
|- | |- | ||
|[[Lichen planus|Hypertrophic lichen planus]]<ref name="pmid27222766">{{cite journal |vauthors=Ankad BS, Beergouder SL |title=Hypertrophic lichen planus versus prurigo nodularis: a dermoscopic perspective |journal=Dermatol Pract Concept |volume=6 |issue=2 |pages=9–15 |year=2016 |pmid=27222766 |pmc=4866621 |doi=10.5826/dpc.0602a03 |url=}}</ref> | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Lichen planus|Hypertrophic lichen planus]]<ref name="pmid27222766">{{cite journal |vauthors=Ankad BS, Beergouder SL |title=Hypertrophic lichen planus versus prurigo nodularis: a dermoscopic perspective |journal=Dermatol Pract Concept |volume=6 |issue=2 |pages=9–15 |year=2016 |pmid=27222766 |pmc=4866621 |doi=10.5826/dpc.0602a03 |url=}}</ref> | ||
| | | | ||
* Classically involves shin and ankles and is characterized by [[Hyperkeratosis|hyperkeratotic]] [[Plaque|plaques]] and [[Nodule (medicine)|nodules]] covered by a scale | * Classically involves shin and ankles and is characterized by [[Hyperkeratosis|hyperkeratotic]] [[Plaque|plaques]] and [[Nodule (medicine)|nodules]] covered by a scale | ||
* Lesions may transform into [[Hyperkeratosis|hyperkeratotic]] thickened elevated purplish or reddish [[Plaque|plaques]] and [[nodules]] | * [[Lesions]] may transform into [[Hyperkeratosis|hyperkeratotic]] thickened, elevated, purplish or reddish [[Plaque|plaques]] and [[nodules]] | ||
| | | | ||
* Chronic [[pruritis]] | * Chronic [[pruritis|pruritus]] | ||
* Scaling | * Scaling | ||
* May be asymptomatic | * May be [[asymptomatic]] | ||
| | | | ||
* Associated with [[Hepatitis C virus]] infection<ref name="pmid19770446">{{cite journal |vauthors=Shengyuan L, Songpo Y, Wen W, Wenjing T, Haitao Z, Binyou W |title=Hepatitis C virus and lichen planus: a reciprocal association determined by a meta-analysis |journal=Arch Dermatol |volume=145 |issue=9 |pages=1040–7 |year=2009 |pmid=19770446 |doi=10.1001/archdermatol.2009.200 |url=}}</ref> | * Associated with [[Hepatitis C virus]] infection<ref name="pmid19770446">{{cite journal |vauthors=Shengyuan L, Songpo Y, Wen W, Wenjing T, Haitao Z, Binyou W |title=Hepatitis C virus and lichen planus: a reciprocal association determined by a meta-analysis |journal=Arch Dermatol |volume=145 |issue=9 |pages=1040–7 |year=2009 |pmid=19770446 |doi=10.1001/archdermatol.2009.200 |url=}}</ref> | ||
| | | | ||
[[Image:Lichen_planus2.JPG|200px]] | [[Image:Lichen_planus2.JPG|200px|courtesy of wikipedia.org]] | ||
|- | |- | ||
|Sneddon–Wilkinson disease<ref name="pmid9564592">{{cite journal |vauthors=Lutz ME, Daoud MS, McEvoy MT, Gibson LE |title=Subcorneal pustular dermatosis: a clinical study of ten patients |journal=Cutis |volume=61 |issue=4 |pages=203–8 |year=1998 |pmid=9564592 |doi= |url=}}</ref> | | style="background: #DCDCDC; padding: 5px; text-align: center;" |Sneddon–Wilkinson disease<ref name="pmid9564592">{{cite journal |vauthors=Lutz ME, Daoud MS, McEvoy MT, Gibson LE |title=Subcorneal pustular dermatosis: a clinical study of ten patients |journal=Cutis |volume=61 |issue=4 |pages=203–8 |year=1998 |pmid=9564592 |doi= |url=}}</ref> | ||
| | | | ||
* [[Flaccid]] [[pustules]] that are often generalized and have a tendency to involve the flexural areas | * [[Flaccid]] [[pustules]] that are often generalized and have a tendency to involve the flexural areas | ||
* | * Annular configuration | ||
| | | | ||
* [[Pruritis]] | * [[Pruritis|Pruritus]] | ||
* May be asymptomatic | * May be asymptomatic | ||
| | | | ||
* Associated with: | * Associated with: | ||
** [[Monoclonal gammopathy]], usually an IgA paraproteinemia<ref name="pmid3056995">{{cite journal |vauthors=Kasha EE, Epinette WW |title=Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) in association with a monoclonal IgA gammopathy: a report and review of the literature |journal=J. Am. Acad. Dermatol. |volume=19 |issue=5 Pt 1 |pages=854–8 |year=1988 |pmid=3056995 |doi= |url=}}</ref> | ** [[Monoclonal gammopathy]], usually an [[IgA]] paraproteinemia<ref name="pmid3056995">{{cite journal |vauthors=Kasha EE, Epinette WW |title=Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) in association with a monoclonal IgA gammopathy: a report and review of the literature |journal=J. Am. Acad. Dermatol. |volume=19 |issue=5 Pt 1 |pages=854–8 |year=1988 |pmid=3056995 |doi= |url=}}</ref> | ||
** [[Crohn's disease]]<ref name="pmid1357895">{{cite journal |vauthors=Delaporte E, Colombel JF, Nguyen-Mailfer C, Piette F, Cortot A, Bergoend H |title=Subcorneal pustular dermatosis in a patient with Crohn's disease |journal=Acta Derm. Venereol. |volume=72 |issue=4 |pages=301–2 |year=1992 |pmid=1357895 |doi= |url=}}</ref> | ** [[Crohn's disease]]<ref name="pmid1357895">{{cite journal |vauthors=Delaporte E, Colombel JF, Nguyen-Mailfer C, Piette F, Cortot A, Bergoend H |title=Subcorneal pustular dermatosis in a patient with Crohn's disease |journal=Acta Derm. Venereol. |volume=72 |issue=4 |pages=301–2 |year=1992 |pmid=1357895 |doi= |url=}}</ref> | ||
** [[Osteomyelitis]] | ** [[Osteomyelitis]] | ||
** [[Adalimumab]]<ref name="pmid23489057">{{cite journal |vauthors=Sauder MB, Glassman SJ |title=Palmoplantar subcorneal pustular dermatosis following adalimumab therapy for rheumatoid arthritis |journal=Int. J. Dermatol. |volume=52 |issue=5 |pages=624–8 |year=2013 |pmid=23489057 |doi=10.1111/j.1365-4632.2012.05707.x |url=}}</ref> | ** [[Adalimumab]]<ref name="pmid23489057">{{cite journal |vauthors=Sauder MB, Glassman SJ |title=Palmoplantar subcorneal pustular dermatosis following adalimumab therapy for rheumatoid arthritis |journal=Int. J. Dermatol. |volume=52 |issue=5 |pages=624–8 |year=2013 |pmid=23489057 |doi=10.1111/j.1365-4632.2012.05707.x |url=}}</ref> | ||
| | | | ||
[[Image: | [[Image:Sneddon wilkinson disease 03.jpeg|200px|courtesy http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=427]] | ||
|- | |- | ||
|[[Parapsoriasis|Small plaque parapsoriasis]]<ref name="pmid7026622">{{cite journal |vauthors=Lambert WC, Everett MA |title=The nosology of parapsoriasis |journal=J. Am. Acad. Dermatol. |volume=5 |issue=4 |pages=373–95 |year=1981 |pmid=7026622 |doi= |url=}}</ref> | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Parapsoriasis|Small plaque parapsoriasis]]<ref name="pmid7026622">{{cite journal |vauthors=Lambert WC, Everett MA |title=The nosology of parapsoriasis |journal=J. Am. Acad. Dermatol. |volume=5 |issue=4 |pages=373–95 |year=1981 |pmid=7026622 |doi= |url=}}</ref> | ||
| | | | ||
* [[Erythematous]] [[plaques]] | * [[Erythematous]] [[plaques]] with fine scaly surface | ||
* May present with elongated, finger-like patches | * May present with elongated, finger-like patches | ||
* Symmetrical distribution on the flanks | |||
* Known as digitate dermatosis | |||
| | | | ||
* [[Lesions]] may be [[asymptomatic]] | * [[Lesions]] may be [[asymptomatic]] | ||
| Line 226: | Line 211: | ||
[[Image:Small_plaque_parapsoriasis.jpg|200px|courtesy http://www.regionalderm.com]] | [[Image:Small_plaque_parapsoriasis.jpg|200px|courtesy http://www.regionalderm.com]] | ||
|- | |- | ||
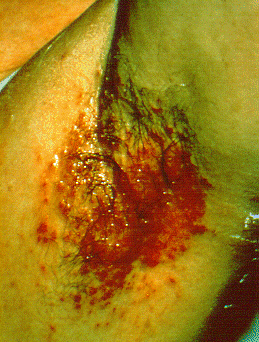
|[[Intertrigo]]<ref name="pmid16156342">{{cite journal |vauthors=Janniger CK, Schwartz RA, Szepietowski JC, Reich A |title=Intertrigo and common secondary skin infections |journal=Am Fam Physician |volume=72 |issue=5 |pages=833–8 |year=2005 |pmid=16156342 |doi= |url=}}</ref> | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Intertrigo]]<ref name="pmid16156342">{{cite journal |vauthors=Janniger CK, Schwartz RA, Szepietowski JC, Reich A |title=Intertrigo and common secondary skin infections |journal=Am Fam Physician |volume=72 |issue=5 |pages=833–8 |year=2005 |pmid=16156342 |doi= |url=}}</ref> | ||
| | | | ||
* Red and fleshy looking lesion in [[skin]] folds | * Red and fleshy looking [[lesion]] in [[skin]] folds | ||
* [[Itching]] | * [[Itching]] | ||
* | * Oozing | ||
* May be sore | * May be sore | ||
| | | | ||
* [[Pruritis]] | * [[Pruritis|Pruritus]] | ||
* Musty odor | * Musty odor | ||
| | | | ||
| Line 242: | Line 227: | ||
** [[Obesity]] | ** [[Obesity]] | ||
| | | | ||
[[Image:Axillary_intertrigo.png|200px]] | [[Image:Axillary_intertrigo.png|200px|courtesy of cdc.gov]] | ||
|- | |- | ||
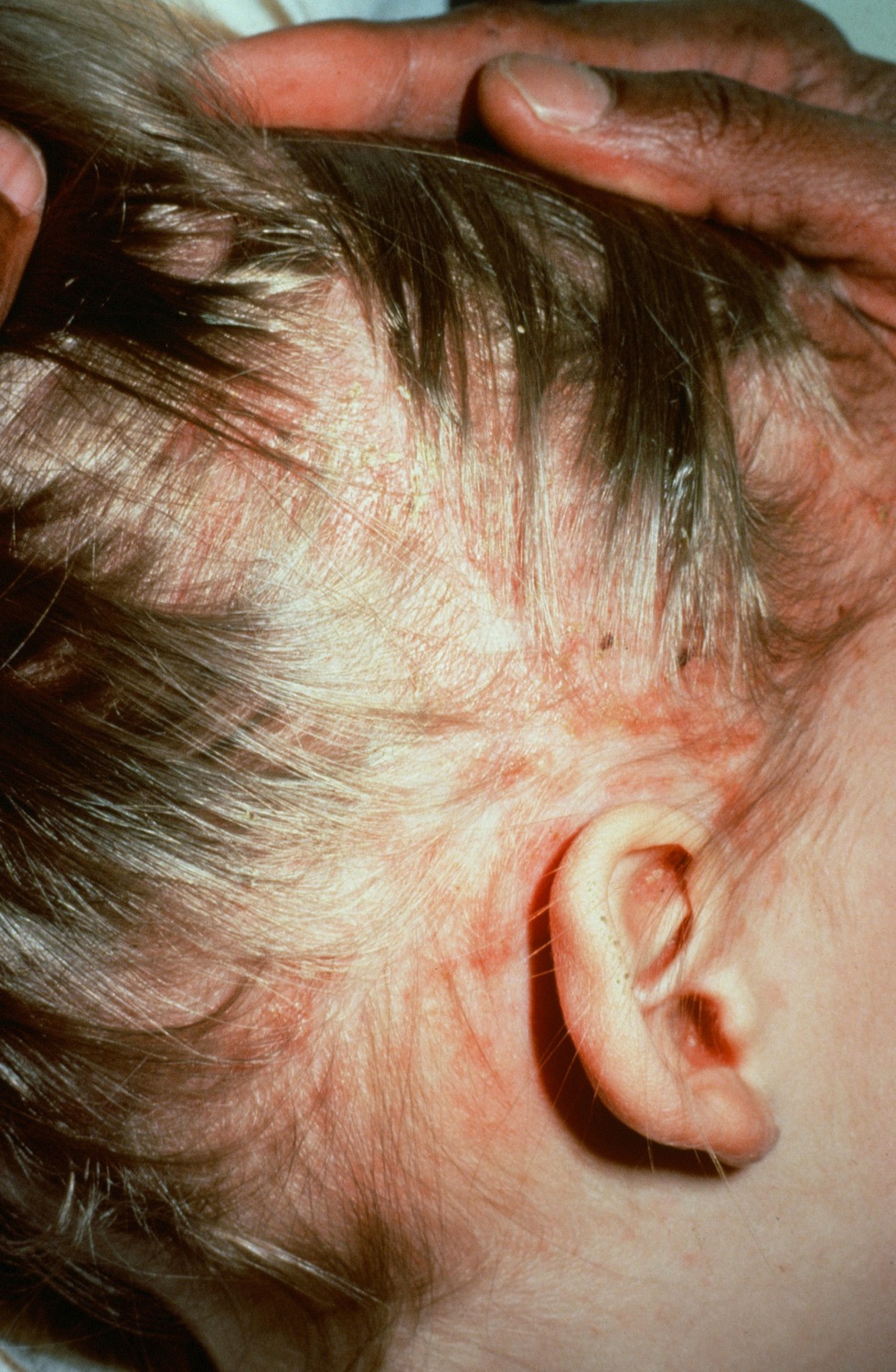
|[[Langerhans cell histiocytosis]]<ref name="pmid18577030">{{cite journal |vauthors=Satter EK, High WA |title=Langerhans cell histiocytosis: a review of the current recommendations of the Histiocyte Society |journal=Pediatr Dermatol |volume=25 |issue=3 |pages=291–5 |year=2008 |pmid=18577030 |doi=10.1111/j.1525-1470.2008.00669.x |url=}}</ref> | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Langerhans cell histiocytosis]]<ref name="pmid18577030">{{cite journal |vauthors=Satter EK, High WA |title=Langerhans cell histiocytosis: a review of the current recommendations of the Histiocyte Society |journal=Pediatr Dermatol |volume=25 |issue=3 |pages=291–5 |year=2008 |pmid=18577030 |doi=10.1111/j.1525-1470.2008.00669.x |url=}}</ref> | ||
| | | | ||
* Scaling and crusting of | * Scaling and crusting of [[scalp]] | ||
| | | | ||
* Pathological fractures<ref name="pmid1636041">{{cite journal |vauthors=Stull MA, Kransdorf MJ, Devaney KO |title=Langerhans cell histiocytosis of bone |journal=Radiographics |volume=12 |issue=4 |pages=801–23 |year=1992 |pmid=1636041 |doi=10.1148/radiographics.12.4.1636041 |url=}}</ref> | * Pathological fractures<ref name="pmid1636041">{{cite journal |vauthors=Stull MA, Kransdorf MJ, Devaney KO |title=Langerhans cell histiocytosis of bone |journal=Radiographics |volume=12 |issue=4 |pages=801–23 |year=1992 |pmid=1636041 |doi=10.1148/radiographics.12.4.1636041 |url=}}</ref> | ||
| Line 258: | Line 243: | ||
** [[Pancytopenia]] | ** [[Pancytopenia]] | ||
| | | | ||
[[Image:Langerhan_cell_histiocytosis.jpg|200px|courtesy http://www.regionalderm.com ]] | [[Image:Langerhan_cell_histiocytosis.jpg|200px|courtesy http://www.regionalderm.com]] | ||
|- | |- | ||
|[[Tinea manuum]]/pedum/capitis<ref name="pmid15050029">{{cite journal |vauthors=Al Hasan M, Fitzgerald SM, Saoudian M, Krishnaswamy G |title=Dermatology for the practicing allergist: Tinea pedis and its complications |journal=Clin Mol Allergy |volume=2 |issue=1 |pages=5 |year=2004 |pmid=15050029 |pmc=419368 |doi=10.1186/1476-7961-2-5 |url=}}</ref> | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Tinea manuum]]/pedum/capitis<ref name="pmid15050029">{{cite journal |vauthors=Al Hasan M, Fitzgerald SM, Saoudian M, Krishnaswamy G |title=Dermatology for the practicing allergist: Tinea pedis and its complications |journal=Clin Mol Allergy |volume=2 |issue=1 |pages=5 |year=2004 |pmid=15050029 |pmc=419368 |doi=10.1186/1476-7961-2-5 |url=}}</ref> | ||
| | | | ||
* Scaling, flaking, and sometimes blistering of the affected areas | * Scaling, flaking, and sometimes blistering of the affected areas | ||
* Hair loss with a black dot on scalp in case of [[tinea capitis]] | * Hair loss with a black dot on scalp in case of [[tinea capitis]] | ||
| | | | ||
* [[Pruritis]] | * [[Pruritis|Pruritus]] | ||
* KOH preparation of the lesions confirms [[fungal infection]] | * [[KOH]] preparation of the [[lesions]] confirms [[fungal infection]] | ||
| | | | ||
* Associated with: | * Associated with: | ||
| Line 274: | Line 259: | ||
** May lead to [[asthma]] exacerbation | ** May lead to [[asthma]] exacerbation | ||
| | | | ||
[[Image:Tinea_pedis.jpg|200px]] | [[Image:Tinea_pedis.jpg|200px|courtesy regionalderm.com]] | ||
|- | |- | ||
|[[Seborrheic dermatitis]] | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Seborrheic dermatitis]] | ||
| | | | ||
* [[Papulosquamous]], scaly, flaky, [[itchy]], and red [[rash]] found particularly at [[sebaceous gland]]-rich areas of the body | * [[Papulosquamous]], scaly, flaky, [[itchy]], and red [[rash]] found particularly at [[sebaceous gland]]-rich areas of the body | ||
| | | | ||
* [[Pruritus]] | |||
| | | | ||
* Associated with:<ref name="pmid16848386">{{cite journal |vauthors=Schwartz RA, Janusz CA, Janniger CK |title=Seborrheic dermatitis: an overview |journal=Am Fam Physician |volume=74 |issue=1 |pages=125–30 |year=2006 |pmid=16848386 |doi= |url=}}</ref> | * Associated with:<ref name="pmid16848386">{{cite journal |vauthors=Schwartz RA, Janusz CA, Janniger CK |title=Seborrheic dermatitis: an overview |journal=Am Fam Physician |volume=74 |issue=1 |pages=125–30 |year=2006 |pmid=16848386 |doi= |url=}}</ref> | ||
| Line 291: | Line 277: | ||
** [[Biotin]] deficiency | ** [[Biotin]] deficiency | ||
| | | | ||
[[Image:Seborrhoeic_dermatitisnew.jpg|200px]] | [[Image:Seborrhoeic_dermatitisnew.jpg|200px|courtesy of wikipedia.com]] | ||
|} | |} | ||
=== Differential diagnosis of psoriatic arthritis === | === Differential diagnosis of psoriatic arthritis === | ||
Psoriatic arthritis must be differentiated from other diseases causing | Psoriatic arthritis must be differentiated from other diseases causing [[Oligoarthritis|oligo]]/[[polyarthritis]] or [[arthritis]] of the [[axial skeleton]], including: | ||
<small> | |||
{| class="wikitable" | {| class="wikitable" | ||
! | ! align="center" style="background:#4479BA; color: #FFFFFF;" + |Arthritis Type | ||
! colspan="7" align="center" style="background:#4479BA; color: #FFFFFF;" ! + |Clinical Features | |||
! colspan="4" align="center" style="background:#4479BA; color: #FFFFFF;" ! + |Body Distribution | |||
! colspan="4" align="center" style="background:#4479BA; color: #FFFFFF;" ! + |Key Signs | |||
! colspan="4" align="center" style="background:#4479BA; color: #FFFFFF;" ! + |Laboratory Abnormalities | |||
! colspan="7" |Clinical Features | |||
! colspan="4" |Body Distribution | |||
! colspan="4" |Key Signs | |||
! colspan=" | |||
|- | |- | ||
| | | | ||
|'''Psoriasis''' | |'''History of Psoriasis''' | ||
|'''Symmetric joint involvement''' | |'''Symmetric [[joint]] involvement''' | ||
|'''Asymmetric joint involvement''' | |'''Asymmetric [[joint]] involvement''' | ||
|[[Enthesopathy|'''Enthesopathy''']] | |[[Enthesopathy|'''Enthesopathy''']] | ||
|'''Dactylitis''' | |'''[[Dactylitis]]''' | ||
|'''Nail Dystrophy''' | |'''[[Nail (anatomy)|Nail]] [[Dystrophy]]''' | ||
|'''Human immunodeficiency virus association''' | |'''[[Human Immunodeficiency Virus (HIV)|Human immunodeficiency virus]] association''' | ||
|'''Upper extremity-hands''' | |'''[[Upper extremity]]-hands''' | ||
|'''Lower extremity''' | |'''[[Lower extremity]]''' | ||
|'''Sacroiliac joints''' | |'''[[Sacroiliac joint|Sacroiliac joints]]''' | ||
|'''Spine''' | |'''[[Spine]]''' | ||
|''' | |'''[[Osteopenia]]''' | ||
|'''Joint Space''' | |'''[[Joint]] Space''' | ||
|'''Ankylosis''' | |'''[[Ankylosis]]''' | ||
|'''Periostitis''' | |'''[[Periostitis]]''' | ||
|'''Soft tissue swelling''' | |'''[[Soft tissue]] swelling''' | ||
|'''ESR''' | |'''[[ESR]]''' | ||
|'''Rheumatoid factor (RF)''' | |'''[[Rheumatoid factor]] ([[Rheumatoid factor|RF]])''' | ||
|'''HLA-B27''' | |'''[[HLA-B27]]''' | ||
|- | |- | ||
|Psoriatic arthritis | |'''[[Psoriatic arthritis]]''' | ||
| + | | + | ||
| + | | + | ||
| Line 371: | Line 319: | ||
| + | | + | ||
| + | | + | ||
| +++ (DIP/PIP) | | +++ ([[Distal interphalangeal joints|DIP]]/[[Proximal interphalangeal joints|PIP]]) | ||
| +++ | | +++ | ||
| ++ (Unilateral) | | ++ (Unilateral) | ||
| Line 384: | Line 332: | ||
|30-75% | |30-75% | ||
|- | |- | ||
|Rheumatoid arthritis | |'''[[Rheumatoid arthritis]]''' | ||
| - | | - | ||
| ++ | | ++ | ||
| Line 392: | Line 340: | ||
| - | | - | ||
| - | | - | ||
| +++ (MCP/wrist) | | +++ | ||
([[MCP joints|MCP]]/[[wrist]]) | |||
| +++ | | +++ | ||
| + (Unilateral) | | + (Unilateral) | ||
| ++(Cervical) | | ++([[Cervical spine|Cervical]]) | ||
| +++ | | +++ | ||
| +++ (Narrowing) | | +++ (Narrowing) | ||
| Line 405: | Line 354: | ||
|6-8% | |6-8% | ||
|- | |- | ||
|Ankylosing spondylitis | |'''[[Ankylosing spondylitis]]''' | ||
| - | | - | ||
| +++ | | +++ | ||
| Line 413: | Line 362: | ||
| - | | - | ||
| - | | - | ||
| | | + | ||
| + | | + | ||
| +++ (Bilateral) | | +++ (Bilateral) | ||
| Line 426: | Line 375: | ||
|90% | |90% | ||
|- | |- | ||
|Reactive arthritis (Reiter's syndrome) | |'''[[Reactive arthritis]] ([[Reiter's syndrome]])''' | ||
| - | | - | ||
| +++ | | +++ | ||
| - | | - | ||
| + | |||
| + | | + | ||
| - | | - | ||
| - | | - | ||
| | | ++ | ||
| +++ | | +++ | ||
| ++ (Unilateral) | | ++ (Unilateral) | ||
| Line 447: | Line 396: | ||
|75% | |75% | ||
|} | |} | ||
Key:+ : Infrequently present, ++ : Frequently present, +++ : Always present, - : Absent | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
Latest revision as of 02:24, 14 August 2017
|
Psoriasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Differentiating psoriasis from other diseases On the Web |
|
American Roentgen Ray Society Images of Differentiating psoriasis from other diseases |
|
Risk calculators and risk factors for Differentiating psoriasis from other diseases |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Syed Hassan A. Kazmi BSc, MD [2]
Overview
Psoriasis must be differentiated from other diseases that cause an erythematous, scaly rash such as cutaneous T cell lymphoma/mycosis fungoides, pityriasis rosea, pityriasis rubra pilaris, pityriasis lichenoides chronica, nummular dermatitis, secondary syphilis, Bowen’s disease, exanthematous pustulosis, hypertrophic lichen planus, Sneddon–Wilkinson disease, small plaque parapsoriasis, intertrigo, Langerhans cell histiocytosis, dyshidrotic dermatitis, tinea manuum/pedum/capitis, and seborrheic dermatitis.
Differentiating psoriasis from other diseases
Differential diagnosis of psoriasis
- Psoriasis must be differentiated from other diseases that cause papulosquamous or erythematosquamous rash, especially when the psoriatic lesions are localized in such sites as the palms, soles, scalp, body folds, penis, and nails. The differential diagnosis of psoriasis includes:
| Disease | Rash Characteristics | Signs and Symptoms | Associated Conditions | Images |
|---|---|---|---|---|
| Cutaneous T cell lymphoma/Mycosis fungoides[1] |
|
|
||
| Pityriasis rosea[2] |
|
|
||
| Pityriasis lichenoides chronica |
|
|
||
| Nummular dermatitis[5] |
|
|
|
|
| Secondary syphilis[6] |
|
|||
| Bowen’s disease[7] |
|
|
||
| Exanthematous pustulosis[9] |
|
|
||
| Hypertrophic lichen planus[11] |
|
|
|
|
| Sneddon–Wilkinson disease[13] |
|
|
||
| Small plaque parapsoriasis[17] |
|
|
|
|
| Intertrigo[19] |
|
|
||
| Langerhans cell histiocytosis[20] |
|
|
|
|
| Tinea manuum/pedum/capitis[24] |
|
|
|
|
| Seborrheic dermatitis |
|
|
Differential diagnosis of psoriatic arthritis
Psoriatic arthritis must be differentiated from other diseases causing oligo/polyarthritis or arthritis of the axial skeleton, including:
| Arthritis Type | Clinical Features | Body Distribution | Key Signs | Laboratory Abnormalities | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| History of Psoriasis | Symmetric joint involvement | Asymmetric joint involvement | Enthesopathy | Dactylitis | Nail Dystrophy | Human immunodeficiency virus association | Upper extremity-hands | Lower extremity | Sacroiliac joints | Spine | Osteopenia | Joint Space | Ankylosis | Periostitis | Soft tissue swelling | ESR | Rheumatoid factor (RF) | HLA-B27 | |
| Psoriatic arthritis | + | + | ++ | + | + | + | + | +++ (DIP/PIP) | +++ | ++ (Unilateral) | ++ | - | ++ (Widening) | ++ | +++ (Fluffy) | ++ | + | - | 30-75% |
| Rheumatoid arthritis | - | ++ | + | - | - | - | - | +++ | +++ | + (Unilateral) | ++(Cervical) | +++ | +++ (Narrowing) | + | + (Linear) | +++ | +++ | +++ | 6-8% |
| Ankylosing spondylitis | - | +++ | - | + | - | - | - | + | + | +++ (Bilateral) | +++ | +++ | ++ (Narrowing) | +++ | +++ (Fluffy) | + | +++ | - | 90% |
| Reactive arthritis (Reiter's syndrome) | - | +++ | - | + | + | - | - | ++ | +++ | ++ (Unilateral) | + | + | + (Narrowing) | - | +++ (Fluffy) | ++ | ++ | - | 75% |
Key:+ : Infrequently present, ++ : Frequently present, +++ : Always present, - : Absent
References
- ↑ "Mycosis Fungoides and the Sézary Syndrome Treatment (PDQ®)—Patient Version - National Cancer Institute".
- ↑ Mahajan K, Relhan V, Relhan AK, Garg VK (2016). "Pityriasis Rosea: An Update on Etiopathogenesis and Management of Difficult Aspects". Indian J Dermatol. 61 (4): 375–84. doi:10.4103/0019-5154.185699. PMC 4966395. PMID 27512182.
- ↑ Prantsidis A, Rigopoulos D, Papatheodorou G, Menounos P, Gregoriou S, Alexiou-Mousatou I, Katsambas A (2009). "Detection of human herpesvirus 8 in the skin of patients with pityriasis rosea". Acta Derm. Venereol. 89 (6): 604–6. doi:10.2340/00015555-0703. PMID 19997691.
- ↑ Smith KJ, Nelson A, Skelton H, Yeager J, Wagner KF (1997). "Pityriasis lichenoides et varioliformis acuta in HIV-1+ patients: a marker of early stage disease. The Military Medical Consortium for the Advancement of Retroviral Research (MMCARR)". Int. J. Dermatol. 36 (2): 104–9. PMID 9109005.
- ↑ Jiamton S, Tangjaturonrusamee C, Kulthanan K (2013). "Clinical features and aggravating factors in nummular eczema in Thais". Asian Pac. J. Allergy Immunol. 31 (1): 36–42. PMID 23517392.
- ↑ "STD Facts - Syphilis".
- ↑ Neagu TP, Ţigliş M, Botezatu D, Enache V, Cobilinschi CO, Vâlcea-Precup MS, GrinŢescu IM (2017). "Clinical, histological and therapeutic features of Bowen's disease". Rom J Morphol Embryol. 58 (1): 33–40. PMID 28523295.
- ↑ Murao K, Yoshioka R, Kubo Y (2014). "Human papillomavirus infection in Bowen disease: negative p53 expression, not p16(INK4a) overexpression, is correlated with human papillomavirus-associated Bowen disease". J. Dermatol. 41 (10): 878–84. doi:10.1111/1346-8138.12613. PMID 25201325.
- ↑ Szatkowski J, Schwartz RA (2015). "Acute generalized exanthematous pustulosis (AGEP): A review and update". J. Am. Acad. Dermatol. 73 (5): 843–8. doi:10.1016/j.jaad.2015.07.017. PMID 26354880.
- ↑ Schmid S, Kuechler PC, Britschgi M, Steiner UC, Yawalkar N, Limat A, Baltensperger K, Braathen L, Pichler WJ (2002). "Acute generalized exanthematous pustulosis: role of cytotoxic T cells in pustule formation". Am. J. Pathol. 161 (6): 2079–86. doi:10.1016/S0002-9440(10)64486-0. PMC 1850901. PMID 12466124.
- ↑ Ankad BS, Beergouder SL (2016). "Hypertrophic lichen planus versus prurigo nodularis: a dermoscopic perspective". Dermatol Pract Concept. 6 (2): 9–15. doi:10.5826/dpc.0602a03. PMC 4866621. PMID 27222766.
- ↑ Shengyuan L, Songpo Y, Wen W, Wenjing T, Haitao Z, Binyou W (2009). "Hepatitis C virus and lichen planus: a reciprocal association determined by a meta-analysis". Arch Dermatol. 145 (9): 1040–7. doi:10.1001/archdermatol.2009.200. PMID 19770446.
- ↑ Lutz ME, Daoud MS, McEvoy MT, Gibson LE (1998). "Subcorneal pustular dermatosis: a clinical study of ten patients". Cutis. 61 (4): 203–8. PMID 9564592.
- ↑ Kasha EE, Epinette WW (1988). "Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) in association with a monoclonal IgA gammopathy: a report and review of the literature". J. Am. Acad. Dermatol. 19 (5 Pt 1): 854–8. PMID 3056995.
- ↑ Delaporte E, Colombel JF, Nguyen-Mailfer C, Piette F, Cortot A, Bergoend H (1992). "Subcorneal pustular dermatosis in a patient with Crohn's disease". Acta Derm. Venereol. 72 (4): 301–2. PMID 1357895.
- ↑ Sauder MB, Glassman SJ (2013). "Palmoplantar subcorneal pustular dermatosis following adalimumab therapy for rheumatoid arthritis". Int. J. Dermatol. 52 (5): 624–8. doi:10.1111/j.1365-4632.2012.05707.x. PMID 23489057.
- ↑ Lambert WC, Everett MA (1981). "The nosology of parapsoriasis". J. Am. Acad. Dermatol. 5 (4): 373–95. PMID 7026622.
- ↑ Väkevä L, Sarna S, Vaalasti A, Pukkala E, Kariniemi AL, Ranki A (2005). "A retrospective study of the probability of the evolution of parapsoriasis en plaques into mycosis fungoides". Acta Derm. Venereol. 85 (4): 318–23. doi:10.1080/00015550510030087. PMID 16191852.
- ↑ Janniger CK, Schwartz RA, Szepietowski JC, Reich A (2005). "Intertrigo and common secondary skin infections". Am Fam Physician. 72 (5): 833–8. PMID 16156342.
- ↑ Satter EK, High WA (2008). "Langerhans cell histiocytosis: a review of the current recommendations of the Histiocyte Society". Pediatr Dermatol. 25 (3): 291–5. doi:10.1111/j.1525-1470.2008.00669.x. PMID 18577030.
- ↑ Stull MA, Kransdorf MJ, Devaney KO (1992). "Langerhans cell histiocytosis of bone". Radiographics. 12 (4): 801–23. doi:10.1148/radiographics.12.4.1636041. PMID 1636041.
- ↑ Sholl LM, Hornick JL, Pinkus JL, Pinkus GS, Padera RF (2007). "Immunohistochemical analysis of langerin in langerhans cell histiocytosis and pulmonary inflammatory and infectious diseases". Am. J. Surg. Pathol. 31 (6): 947–52. doi:10.1097/01.pas.0000249443.82971.bb. PMID 17527085.
- ↑ Grois N, Pötschger U, Prosch H, Minkov M, Arico M, Braier J, Henter JI, Janka-Schaub G, Ladisch S, Ritter J, Steiner M, Unger E, Gadner H (2006). "Risk factors for diabetes insipidus in langerhans cell histiocytosis". Pediatr Blood Cancer. 46 (2): 228–33. doi:10.1002/pbc.20425. PMID 16047354.
- ↑ Al Hasan M, Fitzgerald SM, Saoudian M, Krishnaswamy G (2004). "Dermatology for the practicing allergist: Tinea pedis and its complications". Clin Mol Allergy. 2 (1): 5. doi:10.1186/1476-7961-2-5. PMC 419368. PMID 15050029.
- ↑ Schwartz RA, Janusz CA, Janniger CK (2006). "Seborrheic dermatitis: an overview". Am Fam Physician. 74 (1): 125–30. PMID 16848386.
- ↑ Misery L, Touboul S, Vinçot C, Dutray S, Rolland-Jacob G, Consoli SG, Farcet Y, Feton-Danou N, Cardinaud F, Callot V, De La Chapelle C, Pomey-Rey D, Consoli SM (2007). "[Stress and seborrheic dermatitis]". Ann Dermatol Venereol (in French). 134 (11): 833–7. PMID 18033062.