Chickenpox differential diagnosis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 100: | Line 100: | ||
|} | |} | ||
''' | === '''Oral lesions to be differentiated from chicken pox:''' === | ||
<small><div style="width: 70%;"> | <small><div style="width: 70%;"> | ||
{| class="wikitable" | {| class="wikitable" | ||
Revision as of 14:47, 30 June 2017
|
Chickenpox Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Chickenpox differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Chickenpox differential diagnosis |
|
Risk calculators and risk factors for Chickenpox differential diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Michael Maddaleni, B.S. João André Alves Silva, M.D. [2] Aravind Reddy Kothagadi M.B.B.S[3]
Overview
Chickenpox must be differentiated from various rash causing conditions like Coxsackievirus, Stevens-Johnson syndrome (SJS), Measles, Rubella, rocky mountain spotted fever and Syphilis.
Differentiating Chickenpox from other Diseases
Different rash-like conditions can be confused with chickenpox and are thus included in its differential diagnosis. The various conditions that should be differentiated from chickenpox include:[1][2][3][4][5][6][7]
Common conditions to be differentiated from chickenpox:
| Common Conditions | Features |
|---|---|
| Coxsackievirus |
|
| Stevens-Johnson syndrome |
|
| Kawasaki disease |
|
| Measles |
|
| Syphilis | It commonly presents with gneralized systemic symptoms such as malaise, fatigue, headache and fever. Skin eruptions may be subtle and asymptomatic It is classically described as:
|
| Rubella |
|
| Cytomegalovirus |
|
| Meningococcemia | |
| Meningitis |
|
| Rocky Mountain spotted fever |
|
| Molluscum contagiosum |
|
| Mononucleosis |
|
Less common conditions to be differentiated from chickenpox:
| Less Common Diseases | Features |
|---|---|
| Atypical measles |
|
| Parvovirus B19 | |
| Rickettsial pox | |
| Toxic erythema | |
| Monkeypox |
|
| Rat-bite fever | |
| Scarlet fever |
|
Oral lesions to be differentiated from chicken pox:
| Disease | Presentation | Risk Factors | Diagnosis | Affected Organ Systems | Important features | Picture |
|---|---|---|---|---|---|---|
| Coxsackie virus |
|
|
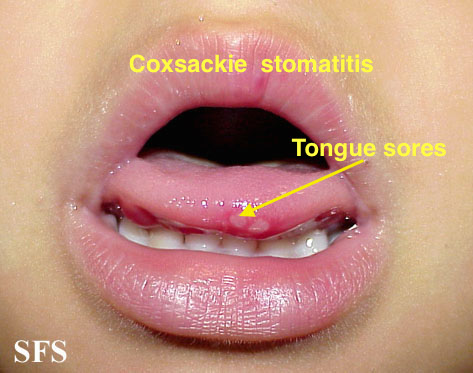
| |||
| Chicken pox |
|
|
|
|
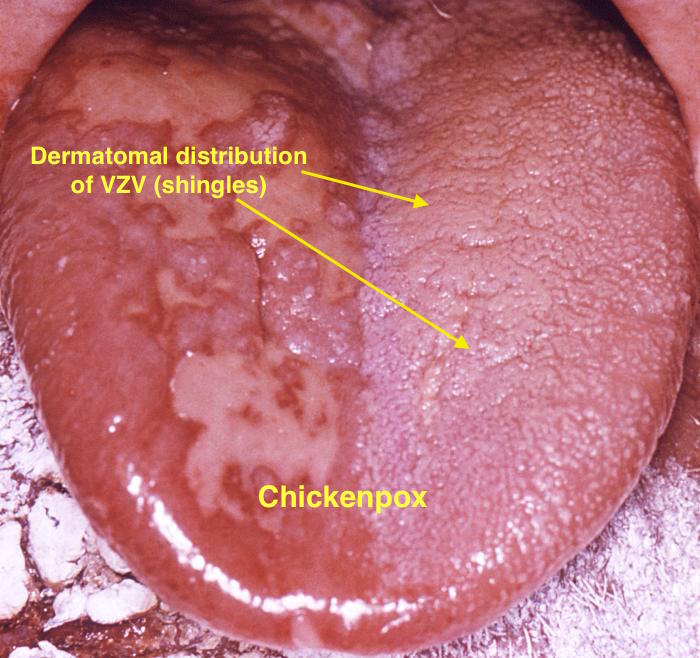
| |
| Measles |
|
|
|
|
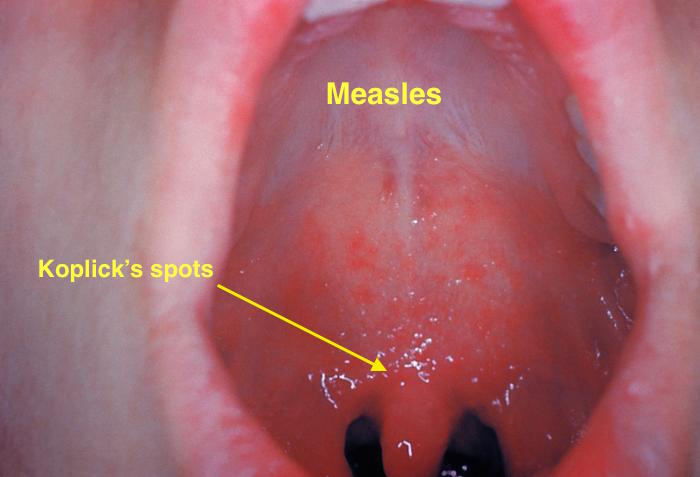
| |
| Herpangina |
|
|
|
|
|
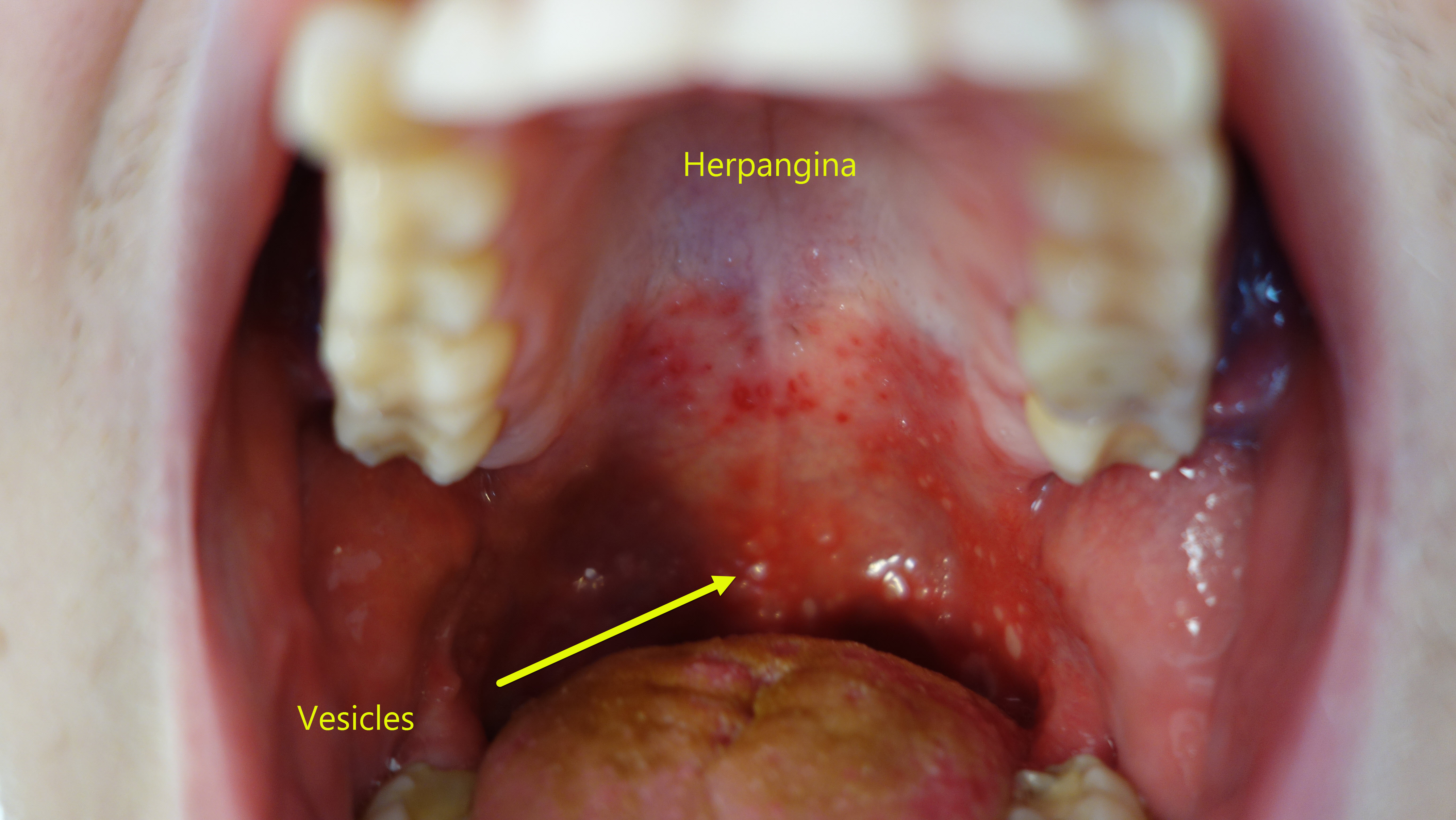 |
| Primary herpetic gingivoestomatitis[10] |
|
|
|
|
|
|
| Oral Candidiasis |
|
|
Localized candidiasis
Invasive candidasis |
|
 |
References
- ↑ Hartman-Adams H, Banvard C, Juckett G (2014). "Impetigo: diagnosis and treatment". Am Fam Physician. 90 (4): 229–35. PMID 25250996.
- ↑ Mehta N, Chen KK, Kroumpouzos G (2016). "Skin disease in pregnancy: The approach of the obstetric medicine physician". Clin Dermatol. 34 (3): 320–6. doi:10.1016/j.clindermatol.2016.02.003. PMID 27265069.
- ↑ Moore, Zack S; Seward, Jane F; Lane, J Michael (2006). "Smallpox". The Lancet. 367 (9508): 425–435. doi:10.1016/S0140-6736(06)68143-9. ISSN 0140-6736.
- ↑ Ibrahim F, Khan T, Pujalte GG (2015). "Bacterial Skin Infections". Prim Care. 42 (4): 485–99. doi:10.1016/j.pop.2015.08.001. PMID 26612370.
- ↑ Ramoni S, Boneschi V, Cusini M (2016). "Syphilis as "the great imitator": a case of impetiginoid syphiloderm". Int J Dermatol. 55 (3): e162–3. doi:10.1111/ijd.13072. PMID 26566601.
- ↑ Kimura U, Yokoyama K, Hiruma M, Kano R, Takamori K, Suga Y (2015). "Tinea faciei caused by Trichophyton mentagrophytes (molecular type Arthroderma benhamiae ) mimics impetigo : a case report and literature review of cases in Japan". Med Mycol J. 56 (1): E1–5. doi:10.3314/mmj.56.E1. PMID 25855021.
- ↑ CEDEF (2012). "[Item 87--Mucocutaneous bacterial infections]". Ann Dermatol Venereol. 139 (11 Suppl): A32–9. doi:10.1016/j.annder.2012.01.002. PMID 23176858.
- ↑ Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE (2000). "Individual and community risks of measles and pertussis associated with personal exemptions to immunization". JAMA. 284 (24): 3145–50. PMID 11135778.
- ↑ Ratnam S, West R, Gadag V, Williams B, Oates E (1996). "Immunity against measles in school-aged children: implications for measles revaccination strategies". Can J Public Health. 87 (6): 407–10. PMID 9009400.
- ↑ Kolokotronis, A.; Doumas, S. (2006). "Herpes simplex virus infection, with particular reference to the progression and complications of primary herpetic gingivostomatitis". Clinical Microbiology and Infection. 12 (3): 202–211. doi:10.1111/j.1469-0691.2005.01336.x. ISSN 1198-743X.
- ↑ Chauvin PJ, Ajar AH (2002). "Acute herpetic gingivostomatitis in adults: a review of 13 cases, including diagnosis and management". J Can Dent Assoc. 68 (4): 247–51. PMID 12626280.
