COVID-19-associated myocardial injury: Difference between revisions
Syed rizvi (talk | contribs) |
Syed rizvi (talk | contribs) |
||
| Line 7: | Line 7: | ||
'''For COVID-19 frequently asked outpatient questions, click [[COVID-19 frequently asked outpatient questions|here]]''' | '''For COVID-19 frequently asked outpatient questions, click [[COVID-19 frequently asked outpatient questions|here]]''' | ||
{{CMG}}; {{AE}} [[User:Syed rizvi|Syed rizvi, M.B.B.S]][[Mailto:syedrizvi555@gmail.com|[2]]] | {{CMG}}; {{AE}} [[User:Syed rizvi|Syed rizvi, M.B.B.S]]<nowiki>[[Mailto:syedrizvi555@gmail.com|[2]]]</nowiki> | ||
'''''Synonyms and Keywords:''''' [[Novel human coronavirus infection|Novel coronavirus]], [[COVID-19]], [[COVID-19|Wuhan coronavirus]], coronavirus disease-19, [[COVID-19|coronavirus disease 2019]], [[SARS-CoV-2]], [[COVID-19]], COVID-19, 2019-nCoV, 2019 novel coronavirus, cardiovascular finding in COVID-19, myocardial injury in COVID-19, COVID-19-associated myocardial injury, SARS-CoV2-associated myocardial injury, COVID-19 myocardial injury. | '''''Synonyms and Keywords:''''' [[Novel human coronavirus infection|Novel coronavirus]], [[COVID-19]], [[COVID-19|Wuhan coronavirus]], coronavirus disease-19, [[COVID-19|coronavirus disease 2019]], [[SARS-CoV-2]], [[COVID-19]], COVID-19, 2019-nCoV, 2019 novel coronavirus, cardiovascular finding in COVID-19, myocardial injury in COVID-19, COVID-19-associated myocardial injury, SARS-CoV2-associated myocardial injury, COVID-19 myocardial injury. | ||
| Line 16: | Line 16: | ||
==Historical Perspective== | ==Historical Perspective== | ||
* [[COVID-19]] ([[SARS-CoV-2]]) [[outbreak]] initiated and was discovered in December, 2019 in Wuhan, Hubei Province, China. | *[[COVID-19]] ([[SARS-CoV-2]]) [[outbreak]] initiated and was discovered in December, 2019 in Wuhan, Hubei Province, China. | ||
* January 30, 2020 - [[World Health Organization]]([[WHO]]) declared the outbreak as a Public Health Emergency of International Concern. | *January 30, 2020 - [[World Health Organization]]([[WHO]]) declared the outbreak as a Public Health Emergency of International Concern. | ||
* March 12, 2020 - WHO declared the [[COVID-19]] outbreak a [[pandemic]]. | *March 12, 2020 - WHO declared the [[COVID-19]] outbreak a [[pandemic]]. | ||
* January 2, 2020 - first observational study of 41 patients with COVID-19 [[pneumonia]] showed that 5 (12%) of the 41 patients had elevated hs-TnI ( [[Troponin|high sensitivity troponin]]) level above the defined threshold (28 pg/ml) <ref name="HuangWang2020">{{cite journal|last1=Huang|first1=Chaolin|last2=Wang|first2=Yeming|last3=Li|first3=Xingwang|last4=Ren|first4=Lili|last5=Zhao|first5=Jianping|last6=Hu|first6=Yi|last7=Zhang|first7=Li|last8=Fan|first8=Guohui|last9=Xu|first9=Jiuyang|last10=Gu|first10=Xiaoying|last11=Cheng|first11=Zhenshun|last12=Yu|first12=Ting|last13=Xia|first13=Jiaan|last14=Wei|first14=Yuan|last15=Wu|first15=Wenjuan|last16=Xie|first16=Xuelei|last17=Yin|first17=Wen|last18=Li|first18=Hui|last19=Liu|first19=Min|last20=Xiao|first20=Yan|last21=Gao|first21=Hong|last22=Guo|first22=Li|last23=Xie|first23=Jungang|last24=Wang|first24=Guangfa|last25=Jiang|first25=Rongmeng|last26=Gao|first26=Zhancheng|last27=Jin|first27=Qi|last28=Wang|first28=Jianwei|last29=Cao|first29=Bin|title=Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China|journal=The Lancet|volume=395|issue=10223|year=2020|pages=497–506|issn=01406736|doi=10.1016/S0140-6736(20)30183-5}}</ref> | *January 2, 2020 - first observational study of 41 patients with COVID-19 [[pneumonia]] showed that 5 (12%) of the 41 patients had elevated hs-TnI ( [[Troponin|high sensitivity troponin]]) level above the defined threshold (28 pg/ml) <ref name="HuangWang2020">{{cite journal|last1=Huang|first1=Chaolin|last2=Wang|first2=Yeming|last3=Li|first3=Xingwang|last4=Ren|first4=Lili|last5=Zhao|first5=Jianping|last6=Hu|first6=Yi|last7=Zhang|first7=Li|last8=Fan|first8=Guohui|last9=Xu|first9=Jiuyang|last10=Gu|first10=Xiaoying|last11=Cheng|first11=Zhenshun|last12=Yu|first12=Ting|last13=Xia|first13=Jiaan|last14=Wei|first14=Yuan|last15=Wu|first15=Wenjuan|last16=Xie|first16=Xuelei|last17=Yin|first17=Wen|last18=Li|first18=Hui|last19=Liu|first19=Min|last20=Xiao|first20=Yan|last21=Gao|first21=Hong|last22=Guo|first22=Li|last23=Xie|first23=Jungang|last24=Wang|first24=Guangfa|last25=Jiang|first25=Rongmeng|last26=Gao|first26=Zhancheng|last27=Jin|first27=Qi|last28=Wang|first28=Jianwei|last29=Cao|first29=Bin|title=Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China|journal=The Lancet|volume=395|issue=10223|year=2020|pages=497–506|issn=01406736|doi=10.1016/S0140-6736(20)30183-5}}</ref> | ||
*To view the historical perspective of COVID-19, [[COVID-19 historical perspective|click here]]. | *To view the historical perspective of COVID-19, [[COVID-19 historical perspective|click here]]. | ||
==Classification== | ==Classification== | ||
* There is no established system for the classification of Acute [[myocardial injury]] in [[COVID-19]]. | *There is no established system for the classification of Acute [[myocardial injury]] in [[COVID-19]]. | ||
* To view the classification of COVID-19, [[COVID-19 classification|click here]]. | *To view the classification of COVID-19, [[COVID-19 classification|click here]]. | ||
A possible classification of COVID-19 associated [[myocardial injury]] is as follows: | A possible classification of COVID-19 associated [[myocardial injury]] is as follows: | ||
* Vascular injury-induced [[myocardial]] death | *Vascular injury-induced [[myocardial]] death | ||
**[[Macrovascular disease|Macrovascular]] disease: Coronary artery thrombosis/plaque rupture | **[[Macrovascular disease|Macrovascular]] disease: Coronary artery thrombosis/plaque rupture | ||
**[[Microvascular disease]]: microvascular thrombosis and [[hypercoagulability]] | **[[Microvascular disease]]: microvascular thrombosis and [[hypercoagulability]] | ||
* Direct myocardial tissue invasion associated injury | *Direct myocardial tissue invasion associated injury | ||
**Acute myocardial depression induced [[heart failure]] | **Acute myocardial depression induced [[heart failure]] | ||
**[[Myocarditis]] | **[[Myocarditis]] | ||
| Line 41: | Line 41: | ||
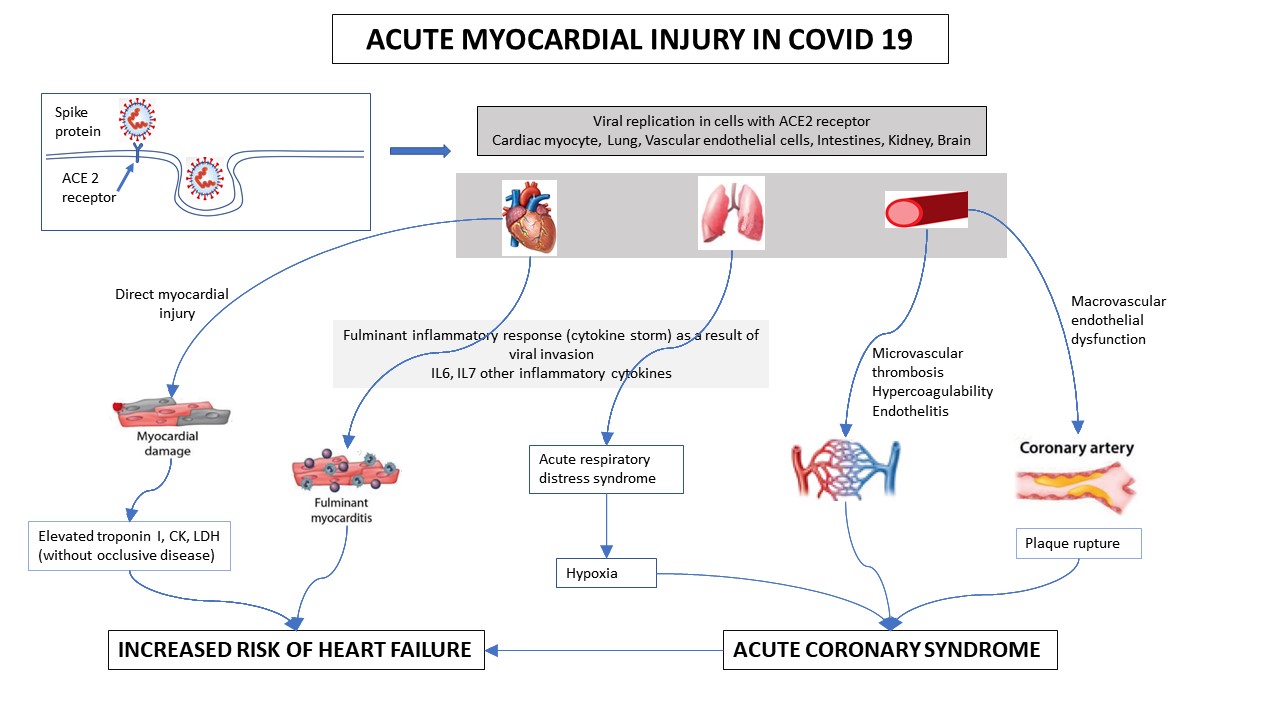
The [[pathophysiology]] of COVID-19 acute [[myocardial injury]] depends on the underlying cause of [[Myocardium|myocardial]] tissue death. However, the overall trigger is an exaggerated [[Inflammation|inflammatory]] response (hyperinflammation) in response to viral infiltration into cells. [[SARS-CoV-2]] virus gains entry via the ACE-2 ([[Angiotensin Converting Enzyme]] 2) receptor that is found abundantly in [[Myocardium|myocardial]] tissue and [[endothelium]] of blood vessels. | The [[pathophysiology]] of COVID-19 acute [[myocardial injury]] depends on the underlying cause of [[Myocardium|myocardial]] tissue death. However, the overall trigger is an exaggerated [[Inflammation|inflammatory]] response (hyperinflammation) in response to viral infiltration into cells. [[SARS-CoV-2]] virus gains entry via the ACE-2 ([[Angiotensin Converting Enzyme]] 2) receptor that is found abundantly in [[Myocardium|myocardial]] tissue and [[endothelium]] of blood vessels. | ||
==== Proposed pathophysiological mechanisms of COVID-19 associated myocardial injury: ==== | ====Proposed pathophysiological mechanisms of COVID-19 associated myocardial injury:==== | ||
*SAQRS-CoV-2 down regulate ACE-2 expression and subsequent protective signaling pathways in [[cardiac myocytes]] | *SAQRS-CoV-2 down regulate ACE-2 expression and subsequent protective signaling pathways in [[cardiac myocytes]] | ||
| Line 56: | Line 56: | ||
**[[Immune]] dysregulation, including [[T cell]] and immune signaling dysfunction, recognized as an important factor in the [[pathogenesis]] of [[vascular disease]], may also adversely affect the body's response to [[SARS-CoV-2]] infection<ref name="MengYang20152">{{cite journal|last1=Meng|first1=Xiao|last2=Yang|first2=Jianmin|last3=Dong|first3=Mei|last4=Zhang|first4=Kai|last5=Tu|first5=Eric|last6=Gao|first6=Qi|last7=Chen|first7=Wanjun|last8=Zhang|first8=Cheng|last9=Zhang|first9=Yun|title=Regulatory T cells in cardiovascular diseases|journal=Nature Reviews Cardiology|volume=13|issue=3|year=2015|pages=167–179|issn=1759-5002|doi=10.1038/nrcardio.2015.169}}</ref> | **[[Immune]] dysregulation, including [[T cell]] and immune signaling dysfunction, recognized as an important factor in the [[pathogenesis]] of [[vascular disease]], may also adversely affect the body's response to [[SARS-CoV-2]] infection<ref name="MengYang20152">{{cite journal|last1=Meng|first1=Xiao|last2=Yang|first2=Jianmin|last3=Dong|first3=Mei|last4=Zhang|first4=Kai|last5=Tu|first5=Eric|last6=Gao|first6=Qi|last7=Chen|first7=Wanjun|last8=Zhang|first8=Cheng|last9=Zhang|first9=Yun|title=Regulatory T cells in cardiovascular diseases|journal=Nature Reviews Cardiology|volume=13|issue=3|year=2015|pages=167–179|issn=1759-5002|doi=10.1038/nrcardio.2015.169}}</ref> | ||
** [[CD4+ cell|CD4]](+) [[CD25]](+) [[FOXP3]](+) [[Regulatory T cell|regulatory T]] (TREG) cells have played a role in [[inflammation]]. TREG cells { T regulatory cells}) plays a vital role in the induction and maintenance of immune [[homeostasis]] and tolerance, any dysregulation in the function or regenaration of TREG cells{ [[Regulatory T cell|Regulatory T]] cells}) can trigger abnormal [[immune responses]], that can lead to [[pathology]]. | **[[CD4+ cell|CD4]](+) [[CD25]](+) [[FOXP3]](+) [[Regulatory T cell|regulatory T]] (TREG) cells have played a role in [[inflammation]]. TREG cells { T regulatory cells}) plays a vital role in the induction and maintenance of immune [[homeostasis]] and tolerance, any dysregulation in the function or regenaration of TREG cells{ [[Regulatory T cell|Regulatory T]] cells}) can trigger abnormal [[immune responses]], that can lead to [[pathology]]. | ||
** [[Naive T cell|Naive]] [[T lymphocytes]] can be primed for [[viral]] [[antigens]] via [[antigen-presenting cells]].<ref name="KomarowskaCoe2015">{{cite journal|last1=Komarowska|first1=Izabela|last2=Coe|first2=David|last3=Wang|first3=Guosu|last4=Haas|first4=Robert|last5=Mauro|first5=Claudio|last6=Kishore|first6=Madhav|last7=Cooper|first7=Dianne|last8=Nadkarni|first8=Suchita|last9=Fu|first9=Hongmei|last10=Steinbruchel|first10=Daniel A.|last11=Pitzalis|first11=Costantino|last12=Anderson|first12=Graham|last13=Bucy|first13=Pat|last14=Lombardi|first14=Giovanna|last15=Breckenridge|first15=Ross|last16=Marelli-Berg|first16=Federica M.|title=Hepatocyte Growth Factor Receptor c-Met Instructs T Cell Cardiotropism and Promotes T Cell Migration to the Heart via Autocrine Chemokine Release|journal=Immunity|volume=42|issue=6|year=2015|pages=1087–1099|issn=10747613|doi=10.1016/j.immuni.2015.05.014}}</ref> | **[[Naive T cell|Naive]] [[T lymphocytes]] can be primed for [[viral]] [[antigens]] via [[antigen-presenting cells]].<ref name="KomarowskaCoe2015">{{cite journal|last1=Komarowska|first1=Izabela|last2=Coe|first2=David|last3=Wang|first3=Guosu|last4=Haas|first4=Robert|last5=Mauro|first5=Claudio|last6=Kishore|first6=Madhav|last7=Cooper|first7=Dianne|last8=Nadkarni|first8=Suchita|last9=Fu|first9=Hongmei|last10=Steinbruchel|first10=Daniel A.|last11=Pitzalis|first11=Costantino|last12=Anderson|first12=Graham|last13=Bucy|first13=Pat|last14=Lombardi|first14=Giovanna|last15=Breckenridge|first15=Ross|last16=Marelli-Berg|first16=Federica M.|title=Hepatocyte Growth Factor Receptor c-Met Instructs T Cell Cardiotropism and Promotes T Cell Migration to the Heart via Autocrine Chemokine Release|journal=Immunity|volume=42|issue=6|year=2015|pages=1087–1099|issn=10747613|doi=10.1016/j.immuni.2015.05.014}}</ref> | ||
** The primed [[CD8+ T cells|CD8+]] [[T lymphocytes]] migrate to the [[Cardiomyocyte|cardiomyocytes]] and through cell-mediated cytotoxicity, cause [[Myocardium|myocardial]] [[inflammation]] and cardio-[[tropism]] by heart-produced [[Hepatocyte Growth Factor]] ([[Hepatocyte Growth Factor|HGF]]) which interacts with [[c-Met]], an [[Hepatocyte Growth Factor|HGF]] receptor on naïve [[T lymphocytes]].<ref name="KomarowskaCoe20152">{{cite journal|last1=Komarowska|first1=Izabela|last2=Coe|first2=David|last3=Wang|first3=Guosu|last4=Haas|first4=Robert|last5=Mauro|first5=Claudio|last6=Kishore|first6=Madhav|last7=Cooper|first7=Dianne|last8=Nadkarni|first8=Suchita|last9=Fu|first9=Hongmei|last10=Steinbruchel|first10=Daniel A.|last11=Pitzalis|first11=Costantino|last12=Anderson|first12=Graham|last13=Bucy|first13=Pat|last14=Lombardi|first14=Giovanna|last15=Breckenridge|first15=Ross|last16=Marelli-Berg|first16=Federica M.|title=Hepatocyte Growth Factor Receptor c-Met Instructs T Cell Cardiotropism and Promotes T Cell Migration to the Heart via Autocrine Chemokine Release|journal=Immunity|volume=42|issue=6|year=2015|pages=1087–1099|issn=10747613|doi=10.1016/j.immuni.2015.05.014}}</ref> | **The primed [[CD8+ T cells|CD8+]] [[T lymphocytes]] migrate to the [[Cardiomyocyte|cardiomyocytes]] and through cell-mediated cytotoxicity, cause [[Myocardium|myocardial]] [[inflammation]] and cardio-[[tropism]] by heart-produced [[Hepatocyte Growth Factor]] ([[Hepatocyte Growth Factor|HGF]]) which interacts with [[c-Met]], an [[Hepatocyte Growth Factor|HGF]] receptor on naïve [[T lymphocytes]].<ref name="KomarowskaCoe20152">{{cite journal|last1=Komarowska|first1=Izabela|last2=Coe|first2=David|last3=Wang|first3=Guosu|last4=Haas|first4=Robert|last5=Mauro|first5=Claudio|last6=Kishore|first6=Madhav|last7=Cooper|first7=Dianne|last8=Nadkarni|first8=Suchita|last9=Fu|first9=Hongmei|last10=Steinbruchel|first10=Daniel A.|last11=Pitzalis|first11=Costantino|last12=Anderson|first12=Graham|last13=Bucy|first13=Pat|last14=Lombardi|first14=Giovanna|last15=Breckenridge|first15=Ross|last16=Marelli-Berg|first16=Federica M.|title=Hepatocyte Growth Factor Receptor c-Met Instructs T Cell Cardiotropism and Promotes T Cell Migration to the Heart via Autocrine Chemokine Release|journal=Immunity|volume=42|issue=6|year=2015|pages=1087–1099|issn=10747613|doi=10.1016/j.immuni.2015.05.014}}</ref> | ||
** In the [[Cytokine storm|cytokine storm syndrome]], [[proinflammatory]] [[cytokines]] such as [[Interleukin-6]] ([[IL-6]]) are released into the [[circulation]], which further augments [[T-lymphocytes|T-lymphocyte]] activation and causes the release of more [[Cytokine|cytokines]].<ref name="ZhouYu20203">{{cite journal|last1=Zhou|first1=Fei|last2=Yu|first2=Ting|last3=Du|first3=Ronghui|last4=Fan|first4=Guohui|last5=Liu|first5=Ying|last6=Liu|first6=Zhibo|last7=Xiang|first7=Jie|last8=Wang|first8=Yeming|last9=Song|first9=Bin|last10=Gu|first10=Xiaoying|last11=Guan|first11=Lulu|last12=Wei|first12=Yuan|last13=Li|first13=Hui|last14=Wu|first14=Xudong|last15=Xu|first15=Jiuyang|last16=Tu|first16=Shengjin|last17=Zhang|first17=Yi|last18=Chen|first18=Hua|last19=Cao|first19=Bin|title=Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study|journal=The Lancet|volume=395|issue=10229|year=2020|pages=1054–1062|issn=01406736|doi=10.1016/S0140-6736(20)30566-3}}</ref> | **In the [[Cytokine storm|cytokine storm syndrome]], [[proinflammatory]] [[cytokines]] such as [[Interleukin-6]] ([[IL-6]]) are released into the [[circulation]], which further augments [[T-lymphocytes|T-lymphocyte]] activation and causes the release of more [[Cytokine|cytokines]].<ref name="ZhouYu20203">{{cite journal|last1=Zhou|first1=Fei|last2=Yu|first2=Ting|last3=Du|first3=Ronghui|last4=Fan|first4=Guohui|last5=Liu|first5=Ying|last6=Liu|first6=Zhibo|last7=Xiang|first7=Jie|last8=Wang|first8=Yeming|last9=Song|first9=Bin|last10=Gu|first10=Xiaoying|last11=Guan|first11=Lulu|last12=Wei|first12=Yuan|last13=Li|first13=Hui|last14=Wu|first14=Xudong|last15=Xu|first15=Jiuyang|last16=Tu|first16=Shengjin|last17=Zhang|first17=Yi|last18=Chen|first18=Hua|last19=Cao|first19=Bin|title=Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study|journal=The Lancet|volume=395|issue=10229|year=2020|pages=1054–1062|issn=01406736|doi=10.1016/S0140-6736(20)30566-3}}</ref> | ||
** [[Cytokine storm|Cytokine storms]] result in increased [[vascular]] wall [[Permeability|permeabilityand]] [[Myocardium|myocardial]] [[edema]].<ref name="HanKim2020">{{cite journal|last1=Han|first1=Seongwook|last2=Kim|first2=Hyun Ah|last3=Kim|first3=Jin Young|last4=Kim|first4=In-Cheol|title=COVID-19-related myocarditis in a 21-year-old female patient|journal=European Heart Journal|volume=41|issue=19|year=2020|pages=1859–1859|issn=0195-668X|doi=10.1093/eurheartj/ehaa288}}</ref> | **[[Cytokine storm|Cytokine storms]] result in increased [[vascular]] wall [[Permeability|permeabilityand]] [[Myocardium|myocardial]] [[edema]].<ref name="HanKim2020">{{cite journal|last1=Han|first1=Seongwook|last2=Kim|first2=Hyun Ah|last3=Kim|first3=Jin Young|last4=Kim|first4=In-Cheol|title=COVID-19-related myocarditis in a 21-year-old female patient|journal=European Heart Journal|volume=41|issue=19|year=2020|pages=1859–1859|issn=0195-668X|doi=10.1093/eurheartj/ehaa288}}</ref> | ||
** A [[positive feedback]] loop of [[immune]] activation and [[myocardial]] damage is established. | **A [[positive feedback]] loop of [[immune]] activation and [[myocardial]] damage is established. | ||
** Thus [[cytokine storm]] activated by [[T helper cells]] ([[Th1]] and [[Th2]]) and a systemic hyperinflammatory response is triggered.<ref name="MehtaMcAuley2020">{{cite journal|last1=Mehta|first1=Puja|last2=McAuley|first2=Daniel F|last3=Brown|first3=Michael|last4=Sanchez|first4=Emilie|last5=Tattersall|first5=Rachel S|last6=Manson|first6=Jessica J|title=COVID-19: consider cytokine storm syndromes and immunosuppression|journal=The Lancet|volume=395|issue=10229|year=2020|pages=1033–1034|issn=01406736|doi=10.1016/S0140-6736(20)30628-0}}</ref> | **Thus [[cytokine storm]] activated by [[T helper cells]] ([[Th1]] and [[Th2]]) and a systemic hyperinflammatory response is triggered.<ref name="MehtaMcAuley2020">{{cite journal|last1=Mehta|first1=Puja|last2=McAuley|first2=Daniel F|last3=Brown|first3=Michael|last4=Sanchez|first4=Emilie|last5=Tattersall|first5=Rachel S|last6=Manson|first6=Jessica J|title=COVID-19: consider cytokine storm syndromes and immunosuppression|journal=The Lancet|volume=395|issue=10229|year=2020|pages=1033–1034|issn=01406736|doi=10.1016/S0140-6736(20)30628-0}}</ref> | ||
| Line 84: | Line 84: | ||
*To view causes of COVID-19, [[COVID-19 causes|click here]]. | *To view causes of COVID-19, [[COVID-19 causes|click here]]. | ||
== Differentiating COVID-19 associated Acute myocardial injury from other Diseases == | ==Differentiating COVID-19 associated Acute myocardial injury from other Diseases== | ||
*[[COVID-19]] associated acute myocardial injury must be differentiated from other causes of [[myocardial injury]] not related to [[COVID-19]] infection. | *[[COVID-19]] associated acute myocardial injury must be differentiated from other causes of [[myocardial injury]] not related to [[COVID-19]] infection. | ||
*<nowiki/>The signs and symptoms of [[Acute coronary syndromes|acute coronary syndrome]], acute [[Congestive heart failure|heart failure]] and [[Myocarditis in COVID 19|myocarditis i]]<nowiki/>nduced by [[COVID-19]] cannot be differentiated from non-COVID-19 acute cardiac disease. Laboratory evaluation with hs-TnI, [[CK]] and [[LDH]] as well as [[EKG]] changes are similar and cannot differentiate between the two disease states | *<nowiki/>The signs and symptoms of [[Acute coronary syndromes|acute coronary syndrome]], acute [[Congestive heart failure|heart failure]] and [[Myocarditis in COVID 19|myocarditis i]]<nowiki/>nduced by [[COVID-19]] cannot be differentiated from non-COVID-19 acute cardiac disease. Laboratory evaluation with hs-TnI, [[CK]] and [[LDH]] as well as [[EKG]] changes are similar and cannot differentiate between the two disease states | ||
*All patients with COVID-19 induced [[myocardial injury]] must be [[PCR]] positive for [[SARS-CoV-2]] | *All patients with COVID-19 induced [[myocardial injury]] must be [[PCR]] positive for [[SARS-CoV-2]] | ||
* The majority of patients have other features of COVID-19, primarily fever, [[pneumonia]] and/or [[ARDS]] at initial presentation <ref name="pmid32139904">{{cite journal |vauthors=Zheng YY, Ma YT, Zhang JY, Xie X |title=COVID-19 and the cardiovascular system |journal=Nat Rev Cardiol |volume=17 |issue=5 |pages=259–260 |date=May 2020 |pmid=32139904 |pmc=7095524 |doi=10.1038/s41569-020-0360-5 |url=}}</ref> | *The majority of patients have other features of COVID-19, primarily fever, [[pneumonia]] and/or [[ARDS]] at initial presentation <ref name="pmid32139904">{{cite journal |vauthors=Zheng YY, Ma YT, Zhang JY, Xie X |title=COVID-19 and the cardiovascular system |journal=Nat Rev Cardiol |volume=17 |issue=5 |pages=259–260 |date=May 2020 |pmid=32139904 |pmc=7095524 |doi=10.1038/s41569-020-0360-5 |url=}}</ref> | ||
* A small number of patients have been reported to present primarily with [[COVID-19]] associated myocardial injury and minimal to no other [[pulmonary]]/systemic symptom | *A small number of patients have been reported to present primarily with [[COVID-19]] associated myocardial injury and minimal to no other [[pulmonary]]/systemic symptom | ||
**For [[chest pain]] differential diagnosis [[Chest pain differential diagnosis|Click here]] | **For [[chest pain]] differential diagnosis [[Chest pain differential diagnosis|Click here]] | ||
**For [[ACS]] differential diagnosis [[ACS|Click here]] | **For [[ACS]] differential diagnosis [[ACS|Click here]] | ||
| Line 98: | Line 98: | ||
{| class="wikitable" | {| class="wikitable" | ||
| colspan="3" | | colspan="3" align="center" style="background: #4479BA; color: #FFFFFF " |'''COVID-19 associated AMI vs non COVID-19 AMI''' | ||
|- | |- | ||
|align="center"|'''Causes''' | | align="center" |'''Causes''' | ||
|align="center"|'''Similar features''' | | align="center" |'''Similar features''' | ||
|align="center"|'''Features specific to COVID-19''' | | align="center" |'''Features specific to COVID-19''' | ||
|- | |- | ||
|[[Acute coronary syndromes|Acute coronary syndrome]] | |[[Acute coronary syndromes|Acute coronary syndrome]] | ||
| Line 171: | Line 171: | ||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
| colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF |'''Study''' | | colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF " |'''Study''' | ||
| colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF |'''Site/''' | | colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF " |'''Site/''' | ||
'''Location''' | '''Location''' | ||
| colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF |'''Sample size (n)''' | | colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF " |'''Sample size (n)''' | ||
| colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF |'''Age (years)''' | | colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF " |'''Age (years)''' | ||
| colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF |'''Pre-existing cardiac disease''' | | colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF " |'''Pre-existing cardiac disease''' | ||
| colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF |'''Definition of myocardial injury used in study''' | | colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF " |'''Definition of myocardial injury used in study''' | ||
| colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF |'''Percent with myocardial injury''' | | colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF " |'''Percent with myocardial injury''' | ||
|- | |- | ||
| colspan="1" rowspan="1" |Huang ''et al'' <ref name="HuangWang20202">{{cite journal|last1=Huang|first1=Chaolin|last2=Wang|first2=Yeming|last3=Li|first3=Xingwang|last4=Ren|first4=Lili|last5=Zhao|first5=Jianping|last6=Hu|first6=Yi|last7=Zhang|first7=Li|last8=Fan|first8=Guohui|last9=Xu|first9=Jiuyang|last10=Gu|first10=Xiaoying|last11=Cheng|first11=Zhenshun|last12=Yu|first12=Ting|last13=Xia|first13=Jiaan|last14=Wei|first14=Yuan|last15=Wu|first15=Wenjuan|last16=Xie|first16=Xuelei|last17=Yin|first17=Wen|last18=Li|first18=Hui|last19=Liu|first19=Min|last20=Xiao|first20=Yan|last21=Gao|first21=Hong|last22=Guo|first22=Li|last23=Xie|first23=Jungang|last24=Wang|first24=Guangfa|last25=Jiang|first25=Rongmeng|last26=Gao|first26=Zhancheng|last27=Jin|first27=Qi|last28=Wang|first28=Jianwei|last29=Cao|first29=Bin|title=Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China|journal=The Lancet|volume=395|issue=10223|year=2020|pages=497–506|issn=01406736|doi=10.1016/S0140-6736(20)30183-5}}</ref> | | colspan="1" rowspan="1" |Huang ''et al'' <ref name="HuangWang20202">{{cite journal|last1=Huang|first1=Chaolin|last2=Wang|first2=Yeming|last3=Li|first3=Xingwang|last4=Ren|first4=Lili|last5=Zhao|first5=Jianping|last6=Hu|first6=Yi|last7=Zhang|first7=Li|last8=Fan|first8=Guohui|last9=Xu|first9=Jiuyang|last10=Gu|first10=Xiaoying|last11=Cheng|first11=Zhenshun|last12=Yu|first12=Ting|last13=Xia|first13=Jiaan|last14=Wei|first14=Yuan|last15=Wu|first15=Wenjuan|last16=Xie|first16=Xuelei|last17=Yin|first17=Wen|last18=Li|first18=Hui|last19=Liu|first19=Min|last20=Xiao|first20=Yan|last21=Gao|first21=Hong|last22=Guo|first22=Li|last23=Xie|first23=Jungang|last24=Wang|first24=Guangfa|last25=Jiang|first25=Rongmeng|last26=Gao|first26=Zhancheng|last27=Jin|first27=Qi|last28=Wang|first28=Jianwei|last29=Cao|first29=Bin|title=Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China|journal=The Lancet|volume=395|issue=10223|year=2020|pages=497–506|issn=01406736|doi=10.1016/S0140-6736(20)30183-5}}</ref> | ||
| Line 227: | Line 227: | ||
| colspan="1" rowspan="1" |7.2 | | colspan="1" rowspan="1" |7.2 | ||
|}<br /> | |}<br /> | ||
=== Incidence === | ===Incidence=== | ||
* The incidence of [[COVID-19]] associated [[myocardial injury]] has not been established yet. | *The incidence of [[COVID-19]] associated [[myocardial injury]] has not been established yet. | ||
=== Prevalence === | ===Prevalence=== | ||
* The prevalence of [[myocardial]] injury (as reflected by elevation in [[Cardiac troponin I (cTnI) and T (cTnT)|cardiac troponin]] levels) is variable among hospitalized patients with [[COVID-19]] and its around 5000-38000 per 100,000 hospitalized individuals worldwide.<ref name="pmid32512122">{{cite journal |vauthors=Bavishi C, Bonow RO, Trivedi V, Abbott JD, Messerli FH, Bhatt DL |title=Acute myocardial injury in patients hospitalized with COVID-19 infection: A review |journal=Prog Cardiovasc Dis |volume= |issue= |pages= |date=June 2020 |pmid=32512122 |pmc=7274977 |doi=10.1016/j.pcad.2020.05.013 |url=}}</ref> | *The prevalence of [[myocardial]] injury (as reflected by elevation in [[Cardiac troponin I (cTnI) and T (cTnT)|cardiac troponin]] levels) is variable among hospitalized patients with [[COVID-19]] and its around 5000-38000 per 100,000 hospitalized individuals worldwide.<ref name="pmid32512122">{{cite journal |vauthors=Bavishi C, Bonow RO, Trivedi V, Abbott JD, Messerli FH, Bhatt DL |title=Acute myocardial injury in patients hospitalized with COVID-19 infection: A review |journal=Prog Cardiovasc Dis |volume= |issue= |pages= |date=June 2020 |pmid=32512122 |pmc=7274977 |doi=10.1016/j.pcad.2020.05.013 |url=}}</ref> | ||
*Reported frequencies of 5 to 38 percent <ref name="pmid325121222">{{cite journal |vauthors=Bavishi C, Bonow RO, Trivedi V, Abbott JD, Messerli FH, Bhatt DL |title=Acute myocardial injury in patients hospitalized with COVID-19 infection: A review |journal=Prog Cardiovasc Dis |volume= |issue= |pages= |date=June 2020 |pmid=32512122 |pmc=7274977 |doi=10.1016/j.pcad.2020.05.013 |url=}}</ref> <ref name="pmid32211816">{{cite journal |vauthors=Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C |title=Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China |journal=JAMA Cardiol |volume= |issue= |pages= |date=March 2020 |pmid=32211816 |pmc=7097841 |doi=10.1001/jamacardio.2020.0950 |url=}}</ref> <ref name="pmid32169400">{{cite journal |vauthors=Lippi G, Lavie CJ, Sanchis-Gomar F |title=Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): Evidence from a meta-analysis |journal=Prog Cardiovasc Dis |volume= |issue= |pages= |date=March 2020 |pmid=32169400 |pmc=7127395 |doi=10.1016/j.pcad.2020.03.001 |url=}}</ref> | *Reported frequencies of 5 to 38 percent <ref name="pmid325121222">{{cite journal |vauthors=Bavishi C, Bonow RO, Trivedi V, Abbott JD, Messerli FH, Bhatt DL |title=Acute myocardial injury in patients hospitalized with COVID-19 infection: A review |journal=Prog Cardiovasc Dis |volume= |issue= |pages= |date=June 2020 |pmid=32512122 |pmc=7274977 |doi=10.1016/j.pcad.2020.05.013 |url=}}</ref> <ref name="pmid32211816">{{cite journal |vauthors=Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C |title=Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China |journal=JAMA Cardiol |volume= |issue= |pages= |date=March 2020 |pmid=32211816 |pmc=7097841 |doi=10.1001/jamacardio.2020.0950 |url=}}</ref> <ref name="pmid32169400">{{cite journal |vauthors=Lippi G, Lavie CJ, Sanchis-Gomar F |title=Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): Evidence from a meta-analysis |journal=Prog Cardiovasc Dis |volume= |issue= |pages= |date=March 2020 |pmid=32169400 |pmc=7127395 |doi=10.1016/j.pcad.2020.03.001 |url=}}</ref> | ||
*In a series of 416 patients with COVID-19 who were hospitalized in Wuhan, China, 19.7 percent had high-sensitivity [[troponin I]] (hs-TnI) above the 99th percentile upper reference limit on admission.<ref name="pmid322118163">{{cite journal |vauthors=Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C |title=Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China |journal=JAMA Cardiol |volume= |issue= |pages= |date=March 2020 |pmid=32211816 |pmc=7097841 |doi=10.1001/jamacardio.2020.0950 |url=}}</ref> | *In a series of 416 patients with COVID-19 who were hospitalized in Wuhan, China, 19.7 percent had high-sensitivity [[troponin I]] (hs-TnI) above the 99th percentile upper reference limit on admission.<ref name="pmid322118163">{{cite journal |vauthors=Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C |title=Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China |journal=JAMA Cardiol |volume= |issue= |pages= |date=March 2020 |pmid=32211816 |pmc=7097841 |doi=10.1001/jamacardio.2020.0950 |url=}}</ref> | ||
=== Case-fatality rate/Mortality rate === | ===Case-fatality rate/Mortality rate=== | ||
* A summary of 44,672 COVID-19 cases documented by the Chinese Center for Disease Control and Prevention demonstrated a [[case fatality rate]] of 10.5% with comorbid CVD ( [[cardiovascular]] disease) compared to a 2.4% overall [[case fatality rate]]<ref name="pmid32294238">{{cite journal |vauthors=Bodini G, Demarzo MG, Casagrande E, De Maria C, Kayali S, Ziola S, Giannini EG |title=Concerns related to COVID-19 pandemic among patients with inflammatory bowel disease and its influence on patient management |journal=Eur. J. Clin. Invest. |volume=50 |issue=5 |pages=e13233 |date=May 2020 |pmid=32294238 |pmc=7235524 |doi=10.1111/eci.13233 |url=}}</ref> | *A summary of 44,672 COVID-19 cases documented by the Chinese Center for Disease Control and Prevention demonstrated a [[case fatality rate]] of 10.5% with comorbid CVD ( [[cardiovascular]] disease) compared to a 2.4% overall [[case fatality rate]]<ref name="pmid32294238">{{cite journal |vauthors=Bodini G, Demarzo MG, Casagrande E, De Maria C, Kayali S, Ziola S, Giannini EG |title=Concerns related to COVID-19 pandemic among patients with inflammatory bowel disease and its influence on patient management |journal=Eur. J. Clin. Invest. |volume=50 |issue=5 |pages=e13233 |date=May 2020 |pmid=32294238 |pmc=7235524 |doi=10.1111/eci.13233 |url=}}</ref> | ||
*The [[mortality rate]] was also higher in those with [[myocardial injury]] (51.2 versus 4.5 percent).<ref name="pmid32294238" /> | *The [[mortality rate]] was also higher in those with [[myocardial injury]] (51.2 versus 4.5 percent).<ref name="pmid32294238" /> | ||
=== Age === | ===Age=== | ||
* Patients with this marker of [[myocardial injury]] were older and had more comorbidities (including chronic [[Congestive heart failure|heart failure]] in 14.6 versus 1.5 percent), greater laboratory abnormalities (including higher levels of [[C-reactive protein]], [[procalcitonin]], and [[aspartate aminotransferase]]), more lung [[Radiography|radiographic]] abnormalities, and more complications compared with those without [[myocardial injury]]. | *Patients with this marker of [[myocardial injury]] were older and had more comorbidities (including chronic [[Congestive heart failure|heart failure]] in 14.6 versus 1.5 percent), greater laboratory abnormalities (including higher levels of [[C-reactive protein]], [[procalcitonin]], and [[aspartate aminotransferase]]), more lung [[Radiography|radiographic]] abnormalities, and more complications compared with those without [[myocardial injury]]. | ||
=== Race === | ===Race=== | ||
* As of June 12, 2020, age-adjusted hospitalization rates are highest among non-Hispanic American Indian or Alaska Native and non-Hispanic black persons, followed by Hispanic or Latino persons. [https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html CDC] | *As of June 12, 2020, age-adjusted hospitalization rates are highest among non-Hispanic American Indian or Alaska Native and non-Hispanic black persons, followed by Hispanic or Latino persons. [https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html CDC] | ||
** Non-Hispanic American Indian or Alaska Native persons have a rate approximately 5 times that of non-Hispanic white persons, | **Non-Hispanic American Indian or Alaska Native persons have a rate approximately 5 times that of non-Hispanic white persons, | ||
** non-Hispanic black persons have a rate approximately 5 times that of non-Hispanic white persons, | **non-Hispanic black persons have a rate approximately 5 times that of non-Hispanic white persons, | ||
** Hispanic or Latino persons have a rate approximately 4 times that of non-Hispanic white persons | **Hispanic or Latino persons have a rate approximately 4 times that of non-Hispanic white persons | ||
=== Gender === | ===Gender=== | ||
* .There is no data on gender predilection to acute [[myocardial injury]] in [[COVID-19]]. | *.There is no data on gender predilection to acute [[myocardial injury]] in [[COVID-19]]. | ||
=== Region === | ===Region=== | ||
*[[COVID-19]] is a pandemic. | *[[COVID-19]] is a pandemic. | ||
| Line 269: | Line 269: | ||
==Risk Factors== | ==Risk Factors== | ||
* A meta-analysis of 6 studies inclusive of 1,527 patients with [[COVID-19]] examined the prevalence of [[cardiovascular disease]] (CVD) and reported the [[prevalence]] of [[hypertension]], [[cardiac]] and [[cerebrovascular disease]], and [[diabetes]] to be 17.1%, 16.4%, and 9.7%, respectively <ref name="LiYang2020">{{cite journal|last1=Li|first1=Bo|last2=Yang|first2=Jing|last3=Zhao|first3=Faming|last4=Zhi|first4=Lili|last5=Wang|first5=Xiqian|last6=Liu|first6=Lin|last7=Bi|first7=Zhaohui|last8=Zhao|first8=Yunhe|title=Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China|journal=Clinical Research in Cardiology|volume=109|issue=5|year=2020|pages=531–538|issn=1861-0684|doi=10.1007/s00392-020-01626-9}}</ref> | *A meta-analysis of 6 studies inclusive of 1,527 patients with [[COVID-19]] examined the prevalence of [[cardiovascular disease]] (CVD) and reported the [[prevalence]] of [[hypertension]], [[cardiac]] and [[cerebrovascular disease]], and [[diabetes]] to be 17.1%, 16.4%, and 9.7%, respectively <ref name="LiYang2020">{{cite journal|last1=Li|first1=Bo|last2=Yang|first2=Jing|last3=Zhao|first3=Faming|last4=Zhi|first4=Lili|last5=Wang|first5=Xiqian|last6=Liu|first6=Lin|last7=Bi|first7=Zhaohui|last8=Zhao|first8=Yunhe|title=Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China|journal=Clinical Research in Cardiology|volume=109|issue=5|year=2020|pages=531–538|issn=1861-0684|doi=10.1007/s00392-020-01626-9}}</ref> | ||
*To view the risk factors of COVID-19, [[COVID-19 risk factors|click here]]. | *To view the risk factors of COVID-19, [[COVID-19 risk factors|click here]]. | ||
| Line 279: | Line 279: | ||
==Natural History, Complications, and Prognosis== | ==Natural History, Complications, and Prognosis== | ||
=== Complications === | ===Complications=== | ||
*The disease also contributes to cardiovascular complications, including | *The disease also contributes to cardiovascular complications, including | ||
| Line 290: | Line 290: | ||
**Death | **Death | ||
=== Prognosis === | ===Prognosis=== | ||
*Prognosis of [[COVID-19]] [[myocardial]] injury patients is generally poor. | *Prognosis of [[COVID-19]] [[myocardial]] injury patients is generally poor. | ||
* A [[retrospective]] analysis of the cause of death in Chinese patients infected with [[COVID-19]] revealed that 40% of patients died at least in part because of [[myocardial injury]] and [[circulatory]] collapse. | *A [[retrospective]] analysis of the cause of death in Chinese patients infected with [[COVID-19]] revealed that 40% of patients died at least in part because of [[myocardial injury]] and [[circulatory]] collapse. | ||
* In another study, patients hospitalized for [[COVID-19]] infection developed [[cardiac]] injury in roughly 20% of cases; thus leading to greater than 50% [[mortality]]. | *In another study, patients hospitalized for [[COVID-19]] infection developed [[cardiac]] injury in roughly 20% of cases; thus leading to greater than 50% [[mortality]]. | ||
* Older patients with preexisting cardiovascular [[comorbidities]] and [[diabetes]] are prone to develop a higher acuity of illness after contracting [[SARS-CoV-2]] associated with higher risk of myocardial injury and a markedly higher short-term mortality rate.<ref name="GuoFan2020">{{cite journal|last1=Guo|first1=Tao|last2=Fan|first2=Yongzhen|last3=Chen|first3=Ming|last4=Wu|first4=Xiaoyan|last5=Zhang|first5=Lin|last6=He|first6=Tao|last7=Wang|first7=Hairong|last8=Wan|first8=Jing|last9=Wang|first9=Xinghuan|last10=Lu|first10=Zhibing|title=Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19)|journal=JAMA Cardiology|year=2020|issn=2380-6583|doi=10.1001/jamacardio.2020.1017}}</ref> | *Older patients with preexisting cardiovascular [[comorbidities]] and [[diabetes]] are prone to develop a higher acuity of illness after contracting [[SARS-CoV-2]] associated with higher risk of myocardial injury and a markedly higher short-term mortality rate.<ref name="GuoFan2020">{{cite journal|last1=Guo|first1=Tao|last2=Fan|first2=Yongzhen|last3=Chen|first3=Ming|last4=Wu|first4=Xiaoyan|last5=Zhang|first5=Lin|last6=He|first6=Tao|last7=Wang|first7=Hairong|last8=Wan|first8=Jing|last9=Wang|first9=Xinghuan|last10=Lu|first10=Zhibing|title=Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19)|journal=JAMA Cardiology|year=2020|issn=2380-6583|doi=10.1001/jamacardio.2020.1017}}</ref> | ||
**To view natural history, complications, and prognosis of COVID-19, [[COVID-19 natural history, complications and prognosis|click here]]. | **To view natural history, complications, and prognosis of COVID-19, [[COVID-19 natural history, complications and prognosis|click here]]. | ||
==Diagnosis== | ==Diagnosis== | ||
{| class="wikitable" | {| class="wikitable" | ||
| align="center" style="background: #4479BA; color: #FFFFFF |'''Initial evaluation of suspected acute myocardial injury in COVID-19''' | | align="center" style="background: #4479BA; color: #FFFFFF " |'''Initial evaluation of suspected acute myocardial injury in COVID-19''' | ||
|- | |- | ||
|'''History''' <ref name="pmid325121223">{{cite journal |vauthors=Bavishi C, Bonow RO, Trivedi V, Abbott JD, Messerli FH, Bhatt DL |title=Acute myocardial injury in patients hospitalized with COVID-19 infection: A review |journal=Prog Cardiovasc Dis |volume= |issue= |pages= |date=June 2020 |pmid=32512122 |pmc=7274977 |doi=10.1016/j.pcad.2020.05.013 |url=}}</ref> | |'''History''' <ref name="pmid325121223">{{cite journal |vauthors=Bavishi C, Bonow RO, Trivedi V, Abbott JD, Messerli FH, Bhatt DL |title=Acute myocardial injury in patients hospitalized with COVID-19 infection: A review |journal=Prog Cardiovasc Dis |volume= |issue= |pages= |date=June 2020 |pmid=32512122 |pmc=7274977 |doi=10.1016/j.pcad.2020.05.013 |url=}}</ref> | ||
| Line 359: | Line 359: | ||
===Physical Examination=== | ===Physical Examination=== | ||
* To view the complete physical examination in COVID-19, [[COVID-19 physical examination|click here]]. | *To view the complete physical examination in COVID-19, [[COVID-19 physical examination|click here]]. | ||
*To view physical exam of [[Acute coronary syndromes|ACS]] [[Acute coronary syndromes|Click here]] | *To view physical exam of [[Acute coronary syndromes|ACS]] [[Acute coronary syndromes|Click here]] | ||
*To view physical exam of [[Heart failure]] [[Heart failure|Click here]] | *To view physical exam of [[Heart failure]] [[Heart failure|Click here]] | ||
| Line 372: | Line 372: | ||
**Guo et al<sup>11</sup> provide additional novel insights that TnT levels are significantly associated with levels of [[C-reactive protein]] and [[Natriuretic peptides|N-terminal pro-B-type natriuretic peptide]] (NT-proBNP), thus linking myocardial injury to severity of [[inflammation]] and [[ventricular dysfunction]]<ref name="GuoFan20202">{{cite journal|last1=Guo|first1=Tao|last2=Fan|first2=Yongzhen|last3=Chen|first3=Ming|last4=Wu|first4=Xiaoyan|last5=Zhang|first5=Lin|last6=He|first6=Tao|last7=Wang|first7=Hairong|last8=Wan|first8=Jing|last9=Wang|first9=Xinghuan|last10=Lu|first10=Zhibing|title=Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19)|journal=JAMA Cardiology|year=2020|issn=2380-6583|doi=10.1001/jamacardio.2020.1017}}</ref> | **Guo et al<sup>11</sup> provide additional novel insights that TnT levels are significantly associated with levels of [[C-reactive protein]] and [[Natriuretic peptides|N-terminal pro-B-type natriuretic peptide]] (NT-proBNP), thus linking myocardial injury to severity of [[inflammation]] and [[ventricular dysfunction]]<ref name="GuoFan20202">{{cite journal|last1=Guo|first1=Tao|last2=Fan|first2=Yongzhen|last3=Chen|first3=Ming|last4=Wu|first4=Xiaoyan|last5=Zhang|first5=Lin|last6=He|first6=Tao|last7=Wang|first7=Hairong|last8=Wan|first8=Jing|last9=Wang|first9=Xinghuan|last10=Lu|first10=Zhibing|title=Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19)|journal=JAMA Cardiology|year=2020|issn=2380-6583|doi=10.1001/jamacardio.2020.1017}}</ref> | ||
===== Inflammatory biomarkers: ===== | =====Inflammatory biomarkers:===== | ||
* Elevated levels of inflammatory markers including [[erythrocyte sedimentation rate]], [[C reactive protein]], and [[procalcitonin]] are usually seen in myocarditis but they are non-specific and do not confirm the diagnosis. Increases levels of [[Interleukin-6]] (IL-6), [[d-dimer]], serum [[ferritin]], [[prothrombin time]] were seen in COVID-19 patients. | |||
*Elevated levels of inflammatory markers including [[erythrocyte sedimentation rate]], [[C reactive protein]], and [[procalcitonin]] are usually seen in myocarditis but they are non-specific and do not confirm the diagnosis. Increases levels of [[Interleukin-6]] (IL-6), [[d-dimer]], serum [[ferritin]], [[prothrombin time]] were seen in COVID-19 patients. | |||
**To view the laboratory findings on COVID-19, [[COVID-19 laboratory findings|click here]]. | **To view the laboratory findings on COVID-19, [[COVID-19 laboratory findings|click here]]. | ||
| Line 389: | Line 390: | ||
===X-ray=== | ===X-ray=== | ||
* There are no specific X-ray findings in [[COVID-19]] associated myocardial injury. | |||
* To view the x-ray finidings on COVID-19, [[COVID-19 x ray|click here]].<br /> | *There are no specific X-ray findings in [[COVID-19]] associated myocardial injury. | ||
*To view the x-ray finidings on COVID-19, [[COVID-19 x ray|click here]].<br /> | |||
===Ultrasound/Echocardiography=== | ===Ultrasound/Echocardiography=== | ||
* There are no specific ultrasound/ echocardiographic findings related to COVID-19-associated acute myocardial injury | |||
* To view the echocardiographic findings on COVID-19, [[COVID-19 echocardiography and ultrasound|click here]].<br /> | *There are no specific ultrasound/ echocardiographic findings related to COVID-19-associated acute myocardial injury | ||
*To view the echocardiographic findings on COVID-19, [[COVID-19 echocardiography and ultrasound|click here]].<br /> | |||
===CT Scan=== | ===CT Scan=== | ||
* There are no specific CT scan findings related to COVID-19-associated acute myocardial injury. | |||
*There are no specific CT scan findings related to COVID-19-associated acute myocardial injury. | |||
*To view the CT scan findings on COVID-19, [[COVID-19 CT scan|click here]]. | *To view the CT scan findings on COVID-19, [[COVID-19 CT scan|click here]]. | ||
===MRI=== | ===MRI=== | ||
* There are no specific MRI findings related to COVID-19-associated acute myocardial injury. | |||
* To view the MRI findings on COVID-19, [[COVID-19 MRI|click here]].<br /> | *There are no specific MRI findings related to COVID-19-associated acute myocardial injury. | ||
*To view the MRI findings on COVID-19, [[COVID-19 MRI|click here]].<br /> | |||
===Other Imaging Findings=== | ===Other Imaging Findings=== | ||
* There are no other [[imaging]] findings related to COVID-19-associated acute myocardial injury. | |||
* To view other [[imaging]] findings on COVID-19, [[COVID-19 other imaging findings|click here]].<br /> | *There are no other [[imaging]] findings related to COVID-19-associated acute myocardial injury. | ||
*To view other [[imaging]] findings on COVID-19, [[COVID-19 other imaging findings|click here]].<br /> | |||
===Other Diagnostic Findings=== | ===Other Diagnostic Findings=== | ||
* There are no other [[diagnostic]] studies related to COVID-19-associated acute myocardial injury. | |||
* To view other [[diagnostic]] studies for COVID-19, [[COVID-19 other diagnostic studies|click here]].<br /> | *There are no other [[diagnostic]] studies related to COVID-19-associated acute myocardial injury. | ||
*To view other [[diagnostic]] studies for COVID-19, [[COVID-19 other diagnostic studies|click here]].<br /> | |||
==Treatment== | ==Treatment== | ||
=== Medical Therapy === | ===Medical Therapy=== | ||
* There are no specific treatments, and treatment varies depending upon presentation, please click on the conditions to see the management. | |||
** ([[COVID-19-associated myocarditis]] | *There are no specific treatments, and treatment varies depending upon presentation, please click on the conditions to see the management. | ||
** [[COVID-19-associated myocardial infarction]] | **([[COVID-19-associated myocarditis]] | ||
** [[COVID-19-associated heart failure]] | **[[COVID-19-associated myocardial infarction]] | ||
** [[COVID-19-associated arrhythmia and conduction system disease]] | **[[COVID-19-associated heart failure]] | ||
** [[COVID-19-associated cardiogenic shock]] | **[[COVID-19-associated arrhythmia and conduction system disease]] | ||
** [[COVID-19-associated cardiac arrest]] | **[[COVID-19-associated cardiogenic shock]] | ||
** [[COVID-19-associated pericarditis]] | **[[COVID-19-associated cardiac arrest]] | ||
** [[COVID-19-associated spontaneous coronary artery dissection]] | **[[COVID-19-associated pericarditis]] | ||
**[[COVID-19-associated spontaneous coronary artery dissection]] | |||
**To view medical treatment for COVID-19, click here. | **To view medical treatment for COVID-19, click here. | ||
=== Surgery === | ===Surgery=== | ||
* There is no established surgical intervention for the treatment of COVID-19-associated acute myocardial injury. | |||
*There is no established surgical intervention for the treatment of COVID-19-associated acute myocardial injury. | |||
===Primary Prevention=== | ===Primary Prevention=== | ||
Revision as of 15:30, 20 July 2020
Main article: COVID-19
For COVID-19 frequently asked inpatient questions, click here
For COVID-19 frequently asked outpatient questions, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Syed rizvi, M.B.B.S[[Mailto:syedrizvi555@gmail.com|[2]]]
Synonyms and Keywords: Novel coronavirus, COVID-19, Wuhan coronavirus, coronavirus disease-19, coronavirus disease 2019, SARS-CoV-2, COVID-19, COVID-19, 2019-nCoV, 2019 novel coronavirus, cardiovascular finding in COVID-19, myocardial injury in COVID-19, COVID-19-associated myocardial injury, SARS-CoV2-associated myocardial injury, COVID-19 myocardial injury.
Overview
Coronavirus disease 2019 (COVID-19) is a rapidly expanding global pandemic which is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). COVID-19 is associated with significant morbidity and mortality. It has been seen to cause myocardial injury, usually in patients requiring hospitalization with more severe SARS-CoV 2 infection. COVID-19 associated myocardial injury is a broad term that is used to describe any cause of myocardial tissue death induced by the SARS-CoV-2 virus. This includes acute coronary syndrome, cardiomyopathy and acute heart failure (with or without cardiogenic shock) and myocarditis. Diagnosis is largely based on elevated high sensitivity troponin I (hs-TnI) level of > 99th percentile of the upper limit of normal. The exact prevalence of COVID-19 associated myocardial injury is around 5000-38000 per 100,000 hospitalized individuals worldwide[1].
Historical Perspective
- COVID-19 (SARS-CoV-2) outbreak initiated and was discovered in December, 2019 in Wuhan, Hubei Province, China.
- January 30, 2020 - World Health Organization(WHO) declared the outbreak as a Public Health Emergency of International Concern.
- March 12, 2020 - WHO declared the COVID-19 outbreak a pandemic.
- January 2, 2020 - first observational study of 41 patients with COVID-19 pneumonia showed that 5 (12%) of the 41 patients had elevated hs-TnI ( high sensitivity troponin) level above the defined threshold (28 pg/ml) [2]
- To view the historical perspective of COVID-19, click here.
Classification
- There is no established system for the classification of Acute myocardial injury in COVID-19.
- To view the classification of COVID-19, click here.
A possible classification of COVID-19 associated myocardial injury is as follows:
- Vascular injury-induced myocardial death
- Macrovascular disease: Coronary artery thrombosis/plaque rupture
- Microvascular disease: microvascular thrombosis and hypercoagulability
- Direct myocardial tissue invasion associated injury
- Acute myocardial depression induced heart failure
- Myocarditis
Pathophysiology
The pathophysiology of COVID-19 acute myocardial injury depends on the underlying cause of myocardial tissue death. However, the overall trigger is an exaggerated inflammatory response (hyperinflammation) in response to viral infiltration into cells. SARS-CoV-2 virus gains entry via the ACE-2 (Angiotensin Converting Enzyme 2) receptor that is found abundantly in myocardial tissue and endothelium of blood vessels.
Proposed pathophysiological mechanisms of COVID-19 associated myocardial injury:
- SAQRS-CoV-2 down regulate ACE-2 expression and subsequent protective signaling pathways in cardiac myocytes
- Hyperinflammation and cytokine storm mediated through pathologic T-cells and monocytes leading to myocarditis[3]
- Respiratory failure and hypoxemia resulting in damage to cardiac myocytes[4]
- Hypercoagulability and development of coronary microvascular thrombosis[5]
- Diffuse endothelial injury and ‘endothelitis’ from direct cell invasion of SARS-CoV-2 and/or resulting from host inflammatory response.[6]
- Inflammation and/or stress causing coronary plaque rupture or supply-demand mismatch leading to myocardial ischemia/infarction.[7]
- Direct invasion of the cardiac tissue by COVID-19.[8]
Hyperinflammation and cytokine storm:
- Immune dysregulation, including T cell and immune signaling dysfunction, recognized as an important factor in the pathogenesis of vascular disease, may also adversely affect the body's response to SARS-CoV-2 infection[9]
- CD4(+) CD25(+) FOXP3(+) regulatory T (TREG) cells have played a role in inflammation. TREG cells { T regulatory cells}) plays a vital role in the induction and maintenance of immune homeostasis and tolerance, any dysregulation in the function or regenaration of TREG cells{ Regulatory T cells}) can trigger abnormal immune responses, that can lead to pathology.
- Naive T lymphocytes can be primed for viral antigens via antigen-presenting cells.[10]
- The primed CD8+ T lymphocytes migrate to the cardiomyocytes and through cell-mediated cytotoxicity, cause myocardial inflammation and cardio-tropism by heart-produced Hepatocyte Growth Factor (HGF) which interacts with c-Met, an HGF receptor on naïve T lymphocytes.[11]
- In the cytokine storm syndrome, proinflammatory cytokines such as Interleukin-6 (IL-6) are released into the circulation, which further augments T-lymphocyte activation and causes the release of more cytokines.[12]
- Cytokine storms result in increased vascular wall permeabilityand myocardial edema.[13]
- A positive feedback loop of immune activation and myocardial damage is established.
- Thus cytokine storm activated by T helper cells (Th1 and Th2) and a systemic hyperinflammatory response is triggered.[14]
Role of ACE-2 Receptor :
- ACE-2 is a membrane-bound aminopeptidate receptor expressed on the epithelial cells of the lungs, intestines, kidneys and blood vessels. It has important immune and cardiovascular roles. Angiotensin-converting enzyme (ACE) cleaves angiotensin I to generate angiotensin II (Ang II), which binds to and activates AT1R, thus promoting vasoconstriction.
- ACE-2 cleaves angiotensin II and generates angiotensin 1–7, a powerful vasodilator acting through Mas receptors
- SARS-CoV-2 has a spike protein receptor-binding domain, similar to SARS-CoV, which interacts with the ACE-2 receptor and acts as the primary functional receptor for pathogenicity and human-to-human transmission.[15] Furthermore, SARS-CoV-2 binding to ACE-2 leads to its down regulation and increases angiotensin II,a pro-inflammatory factor in the lung.
- This subsequently leads to lower amount of angiotensin 1–7. Thus loss of protective signaling pathway in cardiac myocytes. The detrimental effect of ACE-2 downregulation would impede cardioprotective effects of angiotensin 1–7 leading to increased TNFα production, other cytokines release that can result in acute respiratory distress syndrome, acute cardiac injury and multiorgan dysfunction.[16]
- To view the pathophysiology of COVID-19, click here
Causes
- Hypoxemia induced by Acute respiratory distress syndrome (ARDS)
- Hypercoagulability and plaque rupture
- Hyperinflammation and cytokine storm
- Direct invasion of the cardiac tissue by SARS-CoV-2
- Myocarditis and myocyte necrosis.
- To view causes of COVID-19, click here.
Differentiating COVID-19 associated Acute myocardial injury from other Diseases
- COVID-19 associated acute myocardial injury must be differentiated from other causes of myocardial injury not related to COVID-19 infection.
- The signs and symptoms of acute coronary syndrome, acute heart failure and myocarditis induced by COVID-19 cannot be differentiated from non-COVID-19 acute cardiac disease. Laboratory evaluation with hs-TnI, CK and LDH as well as EKG changes are similar and cannot differentiate between the two disease states
- All patients with COVID-19 induced myocardial injury must be PCR positive for SARS-CoV-2
- The majority of patients have other features of COVID-19, primarily fever, pneumonia and/or ARDS at initial presentation [17]
- A small number of patients have been reported to present primarily with COVID-19 associated myocardial injury and minimal to no other pulmonary/systemic symptom
- For chest pain differential diagnosis Click here
- For ACS differential diagnosis Click here
- For heart failure differential diagnosis Click here
- For myocarditis differential diagnosis Click here
- For the differential diagnosis of COVID-19, click here.
| COVID-19 associated AMI vs non COVID-19 AMI | ||
| Causes | Similar features | Features specific to COVID-19 |
| Acute coronary syndrome
- Type I & II MI |
Chest pain
Shortness of breath Elevated troponin I level Evidence of coronary occlusion by imaging/PCI |
Clinical evidence of SARS-CoV2 infection
- Fever - Cough - Dyspnea - Bilateral ground glass opacities on chest imaging (Patients may have nonspecific symptoms such as fatigue and malaise without specific symptoms of cardiac disease) |
| Acute Heart failure | Chest pain/pressure
Shortness of breath Elevated BNP Depressed ventricular function on echocardiography | |
| Myocarditis | Chest pain
Fatigue S3,S4 or summation gallop Elevated troponin I EKG abnormalities Absence of coronary occlusion | |
| AMI- acute myocardial injury; BNP – Brain Natriuretic peptide; MI – myocardial infarction; NSTEMI - non ST Elevation Myocardial Infarction; PCI – percutaneous intervention; STEMI - ST elevation Myocardial Infarction | ||
Epidemiology and Demographics
| Study | Site/
Location |
Sample size (n) | Age (years) | Pre-existing cardiac disease | Definition of myocardial injury used in study | Percent with myocardial injury |
| Huang et al [18] | Wuhan, China | 41 | Median 49.0 | 15% cardiovascular disease
15% hypertension |
Cardiac injury=troponin I above 99th percentile upper reference limit or new abnormalities on electrocardiography or echocardiography | 12 |
| Shi et al[19] | Wuhan, China | 416 | Median 64.0 (range 21.0–95.0) | 4% chronic heart failure
11% coronary heart disease 31% hypertension |
Cardiac injury=troponin I above 99th percentile upper reference limit, regardless of new abnormalities on electrocardiography or echocardiography | 19.7 |
| Zhou et al [20] | Wuhan, China | 191 | Median 56.0 | 8% coronary heart disease
30% hypertension |
Cardiac injury=high-sensitivity troponin I above 99th percentile upper reference limit or new abnormalities on electrocardiography or echocardiography | 17 |
| Guo et al[21] | Wuhan, China | 187 | Mean 58.5±14.7 | 4% cardiomyopathy
11% coronary heart disease 33% hypertension |
Myocardial injury=troponin T above 99th percentile upper reference limit | 27.8 |
| Wang et al [22] | Wuhan, China | 138 | Median 56.0 | 15% cardiovascular disease
31% hypertension |
Cardiac injury=troponin I above 99th percentile upper reference limit or new abnormalities on electrocardiography or echocardiography | 7.2 |
Incidence
- The incidence of COVID-19 associated myocardial injury has not been established yet.
Prevalence
- The prevalence of myocardial injury (as reflected by elevation in cardiac troponin levels) is variable among hospitalized patients with COVID-19 and its around 5000-38000 per 100,000 hospitalized individuals worldwide.[1]
- Reported frequencies of 5 to 38 percent [23] [24] [25]
- In a series of 416 patients with COVID-19 who were hospitalized in Wuhan, China, 19.7 percent had high-sensitivity troponin I (hs-TnI) above the 99th percentile upper reference limit on admission.[26]
Case-fatality rate/Mortality rate
- A summary of 44,672 COVID-19 cases documented by the Chinese Center for Disease Control and Prevention demonstrated a case fatality rate of 10.5% with comorbid CVD ( cardiovascular disease) compared to a 2.4% overall case fatality rate[27]
- The mortality rate was also higher in those with myocardial injury (51.2 versus 4.5 percent).[27]
Age
- Patients with this marker of myocardial injury were older and had more comorbidities (including chronic heart failure in 14.6 versus 1.5 percent), greater laboratory abnormalities (including higher levels of C-reactive protein, procalcitonin, and aspartate aminotransferase), more lung radiographic abnormalities, and more complications compared with those without myocardial injury.
Race
- As of June 12, 2020, age-adjusted hospitalization rates are highest among non-Hispanic American Indian or Alaska Native and non-Hispanic black persons, followed by Hispanic or Latino persons. CDC
- Non-Hispanic American Indian or Alaska Native persons have a rate approximately 5 times that of non-Hispanic white persons,
- non-Hispanic black persons have a rate approximately 5 times that of non-Hispanic white persons,
- Hispanic or Latino persons have a rate approximately 4 times that of non-Hispanic white persons
Gender
- .There is no data on gender predilection to acute myocardial injury in COVID-19.
Region
- COVID-19 is a pandemic.
Risk Factors
- A meta-analysis of 6 studies inclusive of 1,527 patients with COVID-19 examined the prevalence of cardiovascular disease (CVD) and reported the prevalence of hypertension, cardiac and cerebrovascular disease, and diabetes to be 17.1%, 16.4%, and 9.7%, respectively [28]
- To view the risk factors of COVID-19, click here.
Screening
- There is insufficient evidence to recommend routine screening for acute myocardial injury in COVID-19 patients.
- To view screening for COVID-19, click here.
Natural History, Complications, and Prognosis
Complications
- The disease also contributes to cardiovascular complications, including
Prognosis
- Prognosis of COVID-19 myocardial injury patients is generally poor.
- A retrospective analysis of the cause of death in Chinese patients infected with COVID-19 revealed that 40% of patients died at least in part because of myocardial injury and circulatory collapse.
- In another study, patients hospitalized for COVID-19 infection developed cardiac injury in roughly 20% of cases; thus leading to greater than 50% mortality.
- Older patients with preexisting cardiovascular comorbidities and diabetes are prone to develop a higher acuity of illness after contracting SARS-CoV-2 associated with higher risk of myocardial injury and a markedly higher short-term mortality rate.[29]
- To view natural history, complications, and prognosis of COVID-19, click here.
Diagnosis
| Initial evaluation of suspected acute myocardial injury in COVID-19 |
| History [30] |
|
| Physical exam |
|
| EKG changes |
| Laboratory evaluation |
|
| Imaging studies |
For diagnosing of chest pain Click here
History and Symptoms
- Patients with COVID-19 present with the typical symptoms and signs of SARS-CoV-2 infection such as fever, cough, dyspnea. Acute myocardial injury in COVID-19 presents similar to non COVID-19 realted ACS and heart failure. [32] [33]
- For ACS sign and symptoms please Click here
- For Heart failure sign and symptoms please Click here
- To view the history and symptoms of COVID-19, click here.
Physical Examination
- To view the complete physical examination in COVID-19, click here.
- To view physical exam of ACS Click here
- To view physical exam of Heart failure Click here
Laboratory Findings
- Cardiac Biomarkers:
- The upper reference limit for the high-sensitivity troponin I (hs-TnI) test (0.04ng/mL), based on the 99th percentile of measurements reported in healthy population without the occlusion of coronary arteries.[34][35]
- In the recently published retrospective study of 191 COVID-19 patients from two separate hospitals in China, the incidence of elevation in high-sensitivity cardiac troponin I (cTnI) (>28 pg/ml) was 17%, and it was significantly higher among non-survivors (46% versus 1%, p<0.001).
- Furthermore, elevation of this biomarker was noted to be a predictor of in-hospital death (univariable OR 80.07, 95% CI [10.34–620.36], p<0.0001). The most abrupt increase in cTnI in non-survivors was noted beyond day 16 after the onset of disease. In the same study, the incidence of acute cardiac injury was 17% among all-comers, but significantly higher among non-survivors (59% versus 1%, p<0.0001).[36]
- CK-MB >2.2 ng/mL
- Guo et al11 provide additional novel insights that TnT levels are significantly associated with levels of C-reactive protein and N-terminal pro-B-type natriuretic peptide (NT-proBNP), thus linking myocardial injury to severity of inflammation and ventricular dysfunction[37]
Inflammatory biomarkers:
- Elevated levels of inflammatory markers including erythrocyte sedimentation rate, C reactive protein, and procalcitonin are usually seen in myocarditis but they are non-specific and do not confirm the diagnosis. Increases levels of Interleukin-6 (IL-6), d-dimer, serum ferritin, prothrombin time were seen in COVID-19 patients.
- To view the laboratory findings on COVID-19, click here.
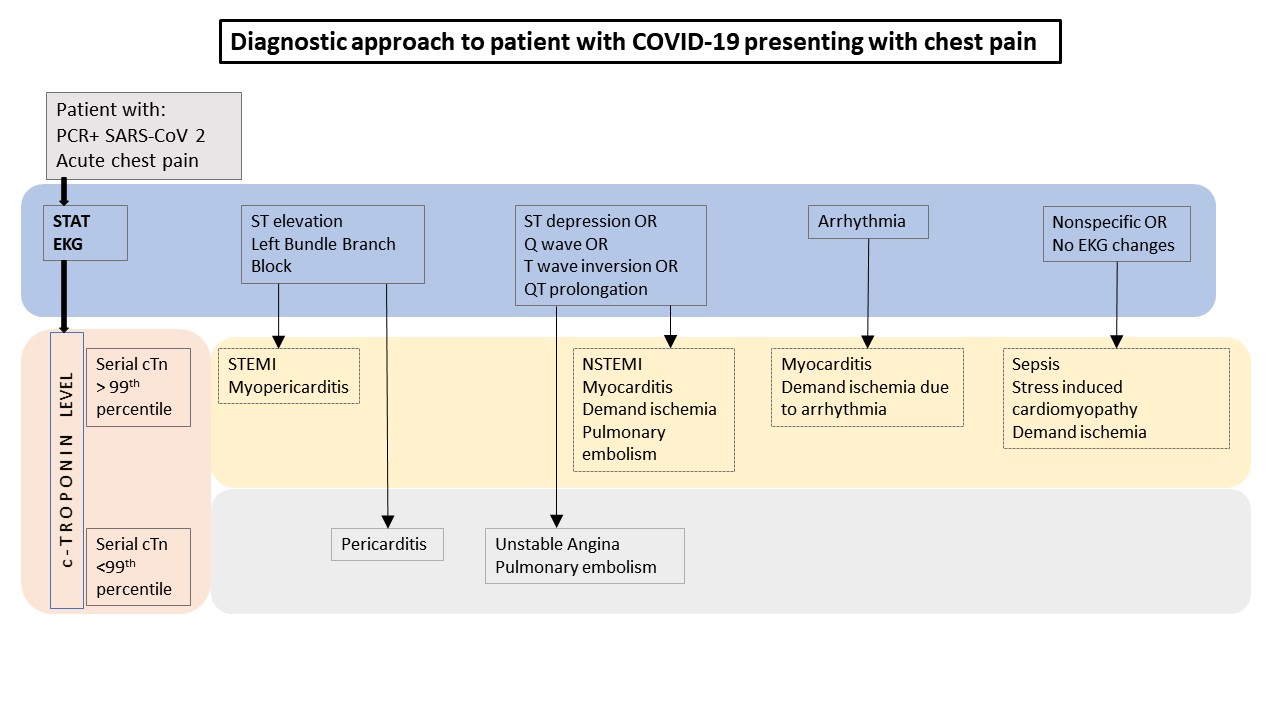
Electrocardiogram
- The electrocardiogram (ECG) can demonstrate a range of findings
- In some cases mimicking acute coronary syndrome (ACS).
- The ECG abnormalities result from myocardial inflammation and include non-specific ST segment-T wave abnormalities.
- T wave inversion.
- PR segment and ST segment deviations (depression and elevation)
- The ECG can help to find previous cardiac abnormalities and triggering factors, such as acute myocardial infarction, and arrhythmias.
- To view the electrocardiogram findings of ACS Click here
- To view the electrocardiogram findings heart failure Click here
- To view the electrocardiogram findings on COVID-19, click here.
X-ray
- There are no specific X-ray findings in COVID-19 associated myocardial injury.
- To view the x-ray finidings on COVID-19, click here.
Ultrasound/Echocardiography
- There are no specific ultrasound/ echocardiographic findings related to COVID-19-associated acute myocardial injury
- To view the echocardiographic findings on COVID-19, click here.
CT Scan
- There are no specific CT scan findings related to COVID-19-associated acute myocardial injury.
- To view the CT scan findings on COVID-19, click here.
MRI
- There are no specific MRI findings related to COVID-19-associated acute myocardial injury.
- To view the MRI findings on COVID-19, click here.
Other Imaging Findings
- There are no other imaging findings related to COVID-19-associated acute myocardial injury.
- To view other imaging findings on COVID-19, click here.
Other Diagnostic Findings
- There are no other diagnostic studies related to COVID-19-associated acute myocardial injury.
- To view other diagnostic studies for COVID-19, click here.
Treatment
Medical Therapy
- There are no specific treatments, and treatment varies depending upon presentation, please click on the conditions to see the management.
- (COVID-19-associated myocarditis
- COVID-19-associated myocardial infarction
- COVID-19-associated heart failure
- COVID-19-associated arrhythmia and conduction system disease
- COVID-19-associated cardiogenic shock
- COVID-19-associated cardiac arrest
- COVID-19-associated pericarditis
- COVID-19-associated spontaneous coronary artery dissection
- To view medical treatment for COVID-19, click here.
Surgery
- There is no established surgical intervention for the treatment of COVID-19-associated acute myocardial injury.
Primary Prevention
- There are no available vaccines against COVID-19 and studies are going on for finding an effective vaccine.
- Other primary prevention strategies include measures to reduce the occurrence of myocardial injury among COVID-19 patients. Recent studies have suggested the use of medications improving microcirculation, especially for the high-risk group such as males, smokers, diabetic patients, and patients with established cardiovascular disease comorbidities.[38]
- For Risk factors associated with COVID-19 please click here
Secondary Prevention
- There are no established measures for the secondary prevention of COVID-19-associated myocardial injury.
References
- ↑ 1.0 1.1 Bavishi C, Bonow RO, Trivedi V, Abbott JD, Messerli FH, Bhatt DL (June 2020). "Acute myocardial injury in patients hospitalized with COVID-19 infection: A review". Prog Cardiovasc Dis. doi:10.1016/j.pcad.2020.05.013. PMC 7274977 Check
|pmc=value (help). PMID 32512122 Check|pmid=value (help). - ↑ Huang, Chaolin; Wang, Yeming; Li, Xingwang; Ren, Lili; Zhao, Jianping; Hu, Yi; Zhang, Li; Fan, Guohui; Xu, Jiuyang; Gu, Xiaoying; Cheng, Zhenshun; Yu, Ting; Xia, Jiaan; Wei, Yuan; Wu, Wenjuan; Xie, Xuelei; Yin, Wen; Li, Hui; Liu, Min; Xiao, Yan; Gao, Hong; Guo, Li; Xie, Jungang; Wang, Guangfa; Jiang, Rongmeng; Gao, Zhancheng; Jin, Qi; Wang, Jianwei; Cao, Bin (2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". The Lancet. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. ISSN 0140-6736.
- ↑ Wei, Haiming; Xu, Xiaoling; Tian, Zhigang; Sun, Rui; Qi, Yingjie; Zhao, Changcheng; Wang, Dongsheng; Zheng, Xiaohu; Fu, Binqing; Zhou, Yonggang (2020). "Pathogenic T-cells and inflammatory monocytes incite inflammatory storms in severe COVID-19 patients". National Science Review. 7 (6): 998–1002. doi:10.1093/nsr/nwaa041. ISSN 2095-5138.
- ↑ Kubasiak, L. A.; Hernandez, O. M.; Bishopric, N. H.; Webster, K. A. (2002). "Hypoxia and acidosis activate cardiac myocyte death through the Bcl-2 family protein BNIP3". Proceedings of the National Academy of Sciences. 99 (20): 12825–12830. doi:10.1073/pnas.202474099. ISSN 0027-8424.
- ↑ Han, Huan; Yang, Lan; Liu, Rui; Liu, Fang; Wu, Kai-lang; Li, Jie; Liu, Xing-hui; Zhu, Cheng-liang (2020). "Prominent changes in blood coagulation of patients with SARS-CoV-2 infection". Clinical Chemistry and Laboratory Medicine (CCLM). 58 (7): 1116–1120. doi:10.1515/cclm-2020-0188. ISSN 1437-4331.
- ↑ Tavazzi, Guido; Pellegrini, Carlo; Maurelli, Marco; Belliato, Mirko; Sciutti, Fabio; Bottazzi, Andrea; Sepe, Paola Alessandra; Resasco, Tullia; Camporotondo, Rita; Bruno, Raffaele; Baldanti, Fausto; Paolucci, Stefania; Pelenghi, Stefano; Iotti, Giorgio Antonio; Mojoli, Francesco; Arbustini, Eloisa (2020). "Myocardial localization of coronavirus in COVID‐19 cardiogenic shock". European Journal of Heart Failure. 22 (5): 911–915. doi:10.1002/ejhf.1828. ISSN 1388-9842.
- ↑ Zhou, Fei; Yu, Ting; Du, Ronghui; Fan, Guohui; Liu, Ying; Liu, Zhibo; Xiang, Jie; Wang, Yeming; Song, Bin; Gu, Xiaoying; Guan, Lulu; Wei, Yuan; Li, Hui; Wu, Xudong; Xu, Jiuyang; Tu, Shengjin; Zhang, Yi; Chen, Hua; Cao, Bin (2020). "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study". The Lancet. 395 (10229): 1054–1062. doi:10.1016/S0140-6736(20)30566-3. ISSN 0140-6736.
- ↑ Tavazzi, Guido; Pellegrini, Carlo; Maurelli, Marco; Belliato, Mirko; Sciutti, Fabio; Bottazzi, Andrea; Sepe, Paola Alessandra; Resasco, Tullia; Camporotondo, Rita; Bruno, Raffaele; Baldanti, Fausto; Paolucci, Stefania; Pelenghi, Stefano; Iotti, Giorgio Antonio; Mojoli, Francesco; Arbustini, Eloisa (2020). "Myocardial localization of coronavirus in COVID‐19 cardiogenic shock". European Journal of Heart Failure. 22 (5): 911–915. doi:10.1002/ejhf.1828. ISSN 1388-9842.
- ↑ Meng, Xiao; Yang, Jianmin; Dong, Mei; Zhang, Kai; Tu, Eric; Gao, Qi; Chen, Wanjun; Zhang, Cheng; Zhang, Yun (2015). "Regulatory T cells in cardiovascular diseases". Nature Reviews Cardiology. 13 (3): 167–179. doi:10.1038/nrcardio.2015.169. ISSN 1759-5002.
- ↑ Komarowska, Izabela; Coe, David; Wang, Guosu; Haas, Robert; Mauro, Claudio; Kishore, Madhav; Cooper, Dianne; Nadkarni, Suchita; Fu, Hongmei; Steinbruchel, Daniel A.; Pitzalis, Costantino; Anderson, Graham; Bucy, Pat; Lombardi, Giovanna; Breckenridge, Ross; Marelli-Berg, Federica M. (2015). "Hepatocyte Growth Factor Receptor c-Met Instructs T Cell Cardiotropism and Promotes T Cell Migration to the Heart via Autocrine Chemokine Release". Immunity. 42 (6): 1087–1099. doi:10.1016/j.immuni.2015.05.014. ISSN 1074-7613.
- ↑ Komarowska, Izabela; Coe, David; Wang, Guosu; Haas, Robert; Mauro, Claudio; Kishore, Madhav; Cooper, Dianne; Nadkarni, Suchita; Fu, Hongmei; Steinbruchel, Daniel A.; Pitzalis, Costantino; Anderson, Graham; Bucy, Pat; Lombardi, Giovanna; Breckenridge, Ross; Marelli-Berg, Federica M. (2015). "Hepatocyte Growth Factor Receptor c-Met Instructs T Cell Cardiotropism and Promotes T Cell Migration to the Heart via Autocrine Chemokine Release". Immunity. 42 (6): 1087–1099. doi:10.1016/j.immuni.2015.05.014. ISSN 1074-7613.
- ↑ Zhou, Fei; Yu, Ting; Du, Ronghui; Fan, Guohui; Liu, Ying; Liu, Zhibo; Xiang, Jie; Wang, Yeming; Song, Bin; Gu, Xiaoying; Guan, Lulu; Wei, Yuan; Li, Hui; Wu, Xudong; Xu, Jiuyang; Tu, Shengjin; Zhang, Yi; Chen, Hua; Cao, Bin (2020). "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study". The Lancet. 395 (10229): 1054–1062. doi:10.1016/S0140-6736(20)30566-3. ISSN 0140-6736.
- ↑ Han, Seongwook; Kim, Hyun Ah; Kim, Jin Young; Kim, In-Cheol (2020). "COVID-19-related myocarditis in a 21-year-old female patient". European Heart Journal. 41 (19): 1859–1859. doi:10.1093/eurheartj/ehaa288. ISSN 0195-668X.
- ↑ Mehta, Puja; McAuley, Daniel F; Brown, Michael; Sanchez, Emilie; Tattersall, Rachel S; Manson, Jessica J (2020). "COVID-19: consider cytokine storm syndromes and immunosuppression". The Lancet. 395 (10229): 1033–1034. doi:10.1016/S0140-6736(20)30628-0. ISSN 0140-6736.
- ↑ Wan, Yushun; Shang, Jian; Graham, Rachel; Baric, Ralph S.; Li, Fang; Gallagher, Tom (2020). "Receptor Recognition by the Novel Coronavirus from Wuhan: an Analysis Based on Decade-Long Structural Studies of SARS Coronavirus". Journal of Virology. 94 (7). doi:10.1128/JVI.00127-20. ISSN 0022-538X.
- ↑ Zhou, Peng; Yang, Xing-Lou; Wang, Xian-Guang; Hu, Ben; Zhang, Lei; Zhang, Wei; Si, Hao-Rui; Zhu, Yan; Li, Bei; Huang, Chao-Lin; Chen, Hui-Dong; Chen, Jing; Luo, Yun; Guo, Hua; Jiang, Ren-Di; Liu, Mei-Qin; Chen, Ying; Shen, Xu-Rui; Wang, Xi; Zheng, Xiao-Shuang; Zhao, Kai; Chen, Quan-Jiao; Deng, Fei; Liu, Lin-Lin; Yan, Bing; Zhan, Fa-Xian; Wang, Yan-Yi; Xiao, Geng-Fu; Shi, Zheng-Li (2020). "A pneumonia outbreak associated with a new coronavirus of probable bat origin". Nature. 579 (7798): 270–273. doi:10.1038/s41586-020-2012-7. ISSN 0028-0836.
- ↑ Zheng YY, Ma YT, Zhang JY, Xie X (May 2020). "COVID-19 and the cardiovascular system". Nat Rev Cardiol. 17 (5): 259–260. doi:10.1038/s41569-020-0360-5. PMC 7095524 Check
|pmc=value (help). PMID 32139904 Check|pmid=value (help). - ↑ Huang, Chaolin; Wang, Yeming; Li, Xingwang; Ren, Lili; Zhao, Jianping; Hu, Yi; Zhang, Li; Fan, Guohui; Xu, Jiuyang; Gu, Xiaoying; Cheng, Zhenshun; Yu, Ting; Xia, Jiaan; Wei, Yuan; Wu, Wenjuan; Xie, Xuelei; Yin, Wen; Li, Hui; Liu, Min; Xiao, Yan; Gao, Hong; Guo, Li; Xie, Jungang; Wang, Guangfa; Jiang, Rongmeng; Gao, Zhancheng; Jin, Qi; Wang, Jianwei; Cao, Bin (2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". The Lancet. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. ISSN 0140-6736.
- ↑ Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C (March 2020). "Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China". JAMA Cardiol. doi:10.1001/jamacardio.2020.0950. PMC 7097841 Check
|pmc=value (help). PMID 32211816 Check|pmid=value (help). - ↑ Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B (March 2020). "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study". Lancet. 395 (10229): 1054–1062. doi:10.1016/S0140-6736(20)30566-3. PMC 7270627 Check
|pmc=value (help). PMID 32171076 Check|pmid=value (help). - ↑ Guo, Tao; Fan, Yongzhen; Chen, Ming; Wu, Xiaoyan; Zhang, Lin; He, Tao; Wang, Hairong; Wan, Jing; Wang, Xinghuan; Lu, Zhibing (2020). "Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19)". JAMA Cardiology. doi:10.1001/jamacardio.2020.1017. ISSN 2380-6583.
- ↑ Wang, Dawei; Hu, Bo; Hu, Chang; Zhu, Fangfang; Liu, Xing; Zhang, Jing; Wang, Binbin; Xiang, Hui; Cheng, Zhenshun; Xiong, Yong; Zhao, Yan; Li, Yirong; Wang, Xinghuan; Peng, Zhiyong (2020). "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China". JAMA. 323 (11): 1061. doi:10.1001/jama.2020.1585. ISSN 0098-7484.
- ↑ Bavishi C, Bonow RO, Trivedi V, Abbott JD, Messerli FH, Bhatt DL (June 2020). "Acute myocardial injury in patients hospitalized with COVID-19 infection: A review". Prog Cardiovasc Dis. doi:10.1016/j.pcad.2020.05.013. PMC 7274977 Check
|pmc=value (help). PMID 32512122 Check|pmid=value (help). - ↑ Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C (March 2020). "Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China". JAMA Cardiol. doi:10.1001/jamacardio.2020.0950. PMC 7097841 Check
|pmc=value (help). PMID 32211816 Check|pmid=value (help). - ↑ Lippi G, Lavie CJ, Sanchis-Gomar F (March 2020). "Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): Evidence from a meta-analysis". Prog Cardiovasc Dis. doi:10.1016/j.pcad.2020.03.001. PMC 7127395 Check
|pmc=value (help). PMID 32169400 Check|pmid=value (help). - ↑ Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C (March 2020). "Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China". JAMA Cardiol. doi:10.1001/jamacardio.2020.0950. PMC 7097841 Check
|pmc=value (help). PMID 32211816 Check|pmid=value (help). - ↑ 27.0 27.1 Bodini G, Demarzo MG, Casagrande E, De Maria C, Kayali S, Ziola S, Giannini EG (May 2020). "Concerns related to COVID-19 pandemic among patients with inflammatory bowel disease and its influence on patient management". Eur. J. Clin. Invest. 50 (5): e13233. doi:10.1111/eci.13233. PMC 7235524 Check
|pmc=value (help). PMID 32294238 Check|pmid=value (help). - ↑ Li, Bo; Yang, Jing; Zhao, Faming; Zhi, Lili; Wang, Xiqian; Liu, Lin; Bi, Zhaohui; Zhao, Yunhe (2020). "Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China". Clinical Research in Cardiology. 109 (5): 531–538. doi:10.1007/s00392-020-01626-9. ISSN 1861-0684.
- ↑ Guo, Tao; Fan, Yongzhen; Chen, Ming; Wu, Xiaoyan; Zhang, Lin; He, Tao; Wang, Hairong; Wan, Jing; Wang, Xinghuan; Lu, Zhibing (2020). "Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19)". JAMA Cardiology. doi:10.1001/jamacardio.2020.1017. ISSN 2380-6583.
- ↑ Bavishi C, Bonow RO, Trivedi V, Abbott JD, Messerli FH, Bhatt DL (June 2020). "Acute myocardial injury in patients hospitalized with COVID-19 infection: A review". Prog Cardiovasc Dis. doi:10.1016/j.pcad.2020.05.013. PMC 7274977 Check
|pmc=value (help). PMID 32512122 Check|pmid=value (help). - ↑ Bavishi C, Bonow RO, Trivedi V, Abbott JD, Messerli FH, Bhatt DL (June 2020). "Acute myocardial injury in patients hospitalized with COVID-19 infection: A review". Prog Cardiovasc Dis. doi:10.1016/j.pcad.2020.05.013. PMC 7274977 Check
|pmc=value (help). PMID 32512122 Check|pmid=value (help). - ↑ Wu, Zunyou; McGoogan, Jennifer M. (2020). "Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China". JAMA. 323 (13): 1239. doi:10.1001/jama.2020.2648. ISSN 0098-7484.
- ↑ Ruan, Qiurong; Yang, Kun; Wang, Wenxia; Jiang, Lingyu; Song, Jianxin (2020). "Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China". Intensive Care Medicine. 46 (5): 846–848. doi:10.1007/s00134-020-05991-x. ISSN 0342-4642.
- ↑ Driggin, Elissa; Madhavan, Mahesh V.; Bikdeli, Behnood; Chuich, Taylor; Laracy, Justin; Biondi-Zoccai, Giuseppe; Brown, Tyler S.; Der Nigoghossian, Caroline; Zidar, David A.; Haythe, Jennifer; Brodie, Daniel; Beckman, Joshua A.; Kirtane, Ajay J.; Stone, Gregg W.; Krumholz, Harlan M.; Parikh, Sahil A. (2020). "Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic". Journal of the American College of Cardiology. 75 (18): 2352–2371. doi:10.1016/j.jacc.2020.03.031. ISSN 0735-1097.
- ↑ Li, Dongze; Chen, You; Jia, Yu; Tong, Le; Tong, Jiale; Wang, Wei; Liu, Yanmei; Wan, Zhi; Cao, Yu; Zeng, Rui (2020). "SARS-CoV-2-Induced Immune Dysregulation and Myocardial Injury Risk in China: Insights from the ERS-COVID-19 Study". Circulation Research. doi:10.1161/CIRCRESAHA.120.317070. ISSN 0009-7330.
- ↑ Zhou, Fei; Yu, Ting; Du, Ronghui; Fan, Guohui; Liu, Ying; Liu, Zhibo; Xiang, Jie; Wang, Yeming; Song, Bin; Gu, Xiaoying; Guan, Lulu; Wei, Yuan; Li, Hui; Wu, Xudong; Xu, Jiuyang; Tu, Shengjin; Zhang, Yi; Chen, Hua; Cao, Bin (2020). "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study". The Lancet. 395 (10229): 1054–1062. doi:10.1016/S0140-6736(20)30566-3. ISSN 0140-6736.
- ↑ Guo, Tao; Fan, Yongzhen; Chen, Ming; Wu, Xiaoyan; Zhang, Lin; He, Tao; Wang, Hairong; Wan, Jing; Wang, Xinghuan; Lu, Zhibing (2020). "Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19)". JAMA Cardiology. doi:10.1001/jamacardio.2020.1017. ISSN 2380-6583.
- ↑ Montone, Rocco A; Iannaccone, Giulia; Meucci, Maria Chiara; Gurgoglione, Filippo; Niccoli, Giampaolo (2020). "Myocardial and Microvascular Injury Due to Coronavirus Disease 2019". European Cardiology Review. 15. doi:10.15420/ecr.2020.22. ISSN 1758-3764.
COVID 19