Arteriovenous fistula: Difference between revisions
No edit summary |
|||
| Line 24: | Line 24: | ||
*Large arteriovenous fistulae (AVF) can lead to congestive heart failure associated with increased activity of vasoconstrictor neurohormonal systems, renin-angiotensin, sympathetic nervous system, endothelin system, and Arginine vasopressin.<ref name="pmid15320481">{{cite journal |vauthors=Abassi ZA, Winaver J, Hoffman A |title=Large A-V fistula: pathophysiological consequences and therapeutic perspectives |journal=Curr Vasc Pharmacol |volume=1 |issue=3 |pages=347–54 |date=October 2003 |pmid=15320481 |doi= |url=}}</ref> | *Large arteriovenous fistulae (AVF) can lead to congestive heart failure associated with increased activity of vasoconstrictor neurohormonal systems, renin-angiotensin, sympathetic nervous system, endothelin system, and Arginine vasopressin.<ref name="pmid15320481">{{cite journal |vauthors=Abassi ZA, Winaver J, Hoffman A |title=Large A-V fistula: pathophysiological consequences and therapeutic perspectives |journal=Curr Vasc Pharmacol |volume=1 |issue=3 |pages=347–54 |date=October 2003 |pmid=15320481 |doi= |url=}}</ref> | ||
*The increased activity of vasoconstrictor neurohormonal systems is in concurrence with compensatory activation of systemic and vasodilating systems, atrial natriuretic peptide (ANP) and nitric oxide (NO). | *The increased activity of vasoconstrictor neurohormonal systems is in concurrence with compensatory activation of systemic and vasodilating systems, atrial natriuretic peptide (ANP) and nitric oxide (NO). | ||
* | *A fistula can progress to an aneurysm, usually in the setting of a trauma, carrying a risk of rupture and necessitating surgical intervention.<ref name="pmid25623503">{{cite journal |vauthors=Soumer K, Benomrane S, Derbel B, Laribi J, Benmrad M, Elleuch N, Kalfat T, Khayati A |title=Popliteal pseudoaneurysm and arteriovenous fistula after acupuncture |journal=J Mal Vasc |volume=40 |issue=1 |pages=58–62 |date=February 2015 |pmid=25623503 |doi=10.1016/j.jmv.2014.11.001 |url=}}</ref> | ||
*The malformation can result in hemorrhage and the risk is significantly higher with small size malformation because of the significantly higher feeding artery pressures.<ref name="pmid1588424">{{cite journal |vauthors=Spetzler RF, Hargraves RW, McCormick PW, Zabramski JM, Flom RA, Zimmerman RS |title=Relationship of perfusion pressure and size to risk of hemorrhage from arteriovenous malformations |journal=J. Neurosurg. |volume=76 |issue=6 |pages=918–23 |date=June 1992 |pmid=1588424 |doi=10.3171/jns.1992.76.6.0918 |url=}}</ref> | *The malformation can result in hemorrhage and the risk is significantly higher with small size malformation because of the significantly higher feeding artery pressures.<ref name="pmid1588424">{{cite journal |vauthors=Spetzler RF, Hargraves RW, McCormick PW, Zabramski JM, Flom RA, Zimmerman RS |title=Relationship of perfusion pressure and size to risk of hemorrhage from arteriovenous malformations |journal=J. Neurosurg. |volume=76 |issue=6 |pages=918–23 |date=June 1992 |pmid=1588424 |doi=10.3171/jns.1992.76.6.0918 |url=}}</ref> | ||
Normal blood flow in the brachial artery is 85 to 110 milliliters per minute (mL/min). After the creation of a fistula, the blood flow increases to 400 to 500 mL/min immediately, and 700 to 1,000 mL/min within 1 month. A bracheocephalic fistula above the elbow has a greater flow rate than a radiocephalic fistula at the wrist. Both the artery and the vein dilate and elongate in response to the greater blood flow and shear stress, but the vein dilates more and becomes "arterialized". In one study, the cephalic vein increased from 2.3 mm to 6.3 mm diameter after 2 months. When the vein is large enough to allow cannulation, the fistula is defined as "mature." | Normal blood flow in the brachial artery is 85 to 110 milliliters per minute (mL/min). After the creation of a fistula, the blood flow increases to 400 to 500 mL/min immediately, and 700 to 1,000 mL/min within 1 month. A bracheocephalic fistula above the elbow has a greater flow rate than a radiocephalic fistula at the wrist. Both the artery and the vein dilate and elongate in response to the greater blood flow and shear stress, but the vein dilates more and becomes "arterialized". In one study, the cephalic vein increased from 2.3 mm to 6.3 mm diameter after 2 months. When the vein is large enough to allow cannulation, the fistula is defined as "mature." | ||
==Clinical Features== | |||
*In the case of coronary arteriovenous fistula (AVF) patients can be asymptomatic or present with:<ref name="pmid26221510">{{cite journal |vauthors=Zamani H, Meragi M, Arabi Moghadam MY, Alizadeh B, Babazadeh K, Mokhtari-Esbuie F |title=Clinical presentation of coronary arteriovenous fistula according to age and anatomic orientation |journal=Caspian J Intern Med |volume=6 |issue=2 |pages=108–12 |date=2015 |pmid=26221510 |pmc=4478461 |doi= |url=}}</ref><ref name="pmid2319939">{{cite journal |vauthors=Sapin P, Frantz E, Jain A, Nichols TC, Dehmer GJ |title=Coronary artery fistula: an abnormality affecting all age groups |journal=Medicine (Baltimore) |volume=69 |issue=2 |pages=101–13 |date=March 1990 |pmid=2319939 |doi= |url=}}</ref> | |||
:*Continuous murmur | |||
:*Cardiomegaly | |||
:*Chest pain | |||
:*Fatigue | |||
:*Palpitation | |||
:*Angina | |||
:*Bacterial endocarditis | |||
==Diagnosis== | ==Diagnosis== | ||
Revision as of 15:51, 31 October 2018
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sabawoon Mirwais, M.B.B.S, M.D.[2]
Overview
An arteriovenous fistula is an abnormal connection or passageway between an artery and a vein. It may be congenital, surgically created for hemodialysis treatments, or acquired due to pathologic process, such as trauma or erosion of an arterial aneurysm. These communications can occur at any point in the vascular system; varying in size, length, location, and number.
Historical Perspective
- Arteriovenous fistula (AVF) was first discovered by William Hunter, in 1758, during a venupuncture with accidental piercing of the artery.[1][2][3]
- Congenital arteriovenous fistula (AVF) of the coronary arteries, a rare cardiac anomaly, was first described by Krause W. Uber, in 1865.[4][5][6]
Classification
- Arteriovenous fistula (AVF) can be classified into:
Vascular Access for Hemodialysis
Patients with end stage renal failure are treated with hemodialysis. In dialysis, blood is withdrawn from an artery or vein, purified, and returned to a vein. The volume of blood is too great for veins to handle, so a vein must be enlarged. An artery and vein, usually in the arm above or below the elbow, are sewn together, to create a fistula, and arterial pressure eventually enlarges the vein. The enlarged vein can accommodate a cannula or large needle.
Pathophysiology
- The abnormal communication causes shunting of blood from high-pressure arterial side to the low-pressure venous side.
- An arteriovenous fistula (AVF) involving a major artery such as the abdominal aorta can lead to a large decrease in peripheral resistance, which in turn causes the heart to increase cardiac output in order to maintain proper blood flow to all tissues.
- The physical manifestations of this would be a relatively normal systolic blood pressure with a decreased diastolic blood pressure resulting in a wide (large) pulse pressure.
- Large arteriovenous fistulae (AVF) can lead to congestive heart failure associated with increased activity of vasoconstrictor neurohormonal systems, renin-angiotensin, sympathetic nervous system, endothelin system, and Arginine vasopressin.[11]
- The increased activity of vasoconstrictor neurohormonal systems is in concurrence with compensatory activation of systemic and vasodilating systems, atrial natriuretic peptide (ANP) and nitric oxide (NO).
- A fistula can progress to an aneurysm, usually in the setting of a trauma, carrying a risk of rupture and necessitating surgical intervention.[12]
- The malformation can result in hemorrhage and the risk is significantly higher with small size malformation because of the significantly higher feeding artery pressures.[13]
Normal blood flow in the brachial artery is 85 to 110 milliliters per minute (mL/min). After the creation of a fistula, the blood flow increases to 400 to 500 mL/min immediately, and 700 to 1,000 mL/min within 1 month. A bracheocephalic fistula above the elbow has a greater flow rate than a radiocephalic fistula at the wrist. Both the artery and the vein dilate and elongate in response to the greater blood flow and shear stress, but the vein dilates more and becomes "arterialized". In one study, the cephalic vein increased from 2.3 mm to 6.3 mm diameter after 2 months. When the vein is large enough to allow cannulation, the fistula is defined as "mature."
Clinical Features
- In the case of coronary arteriovenous fistula (AVF) patients can be asymptomatic or present with:[14][15]
- Continuous murmur
- Cardiomegaly
- Chest pain
- Fatigue
- Palpitation
- Angina
- Bacterial endocarditis
Diagnosis
Doppler Echocardiography
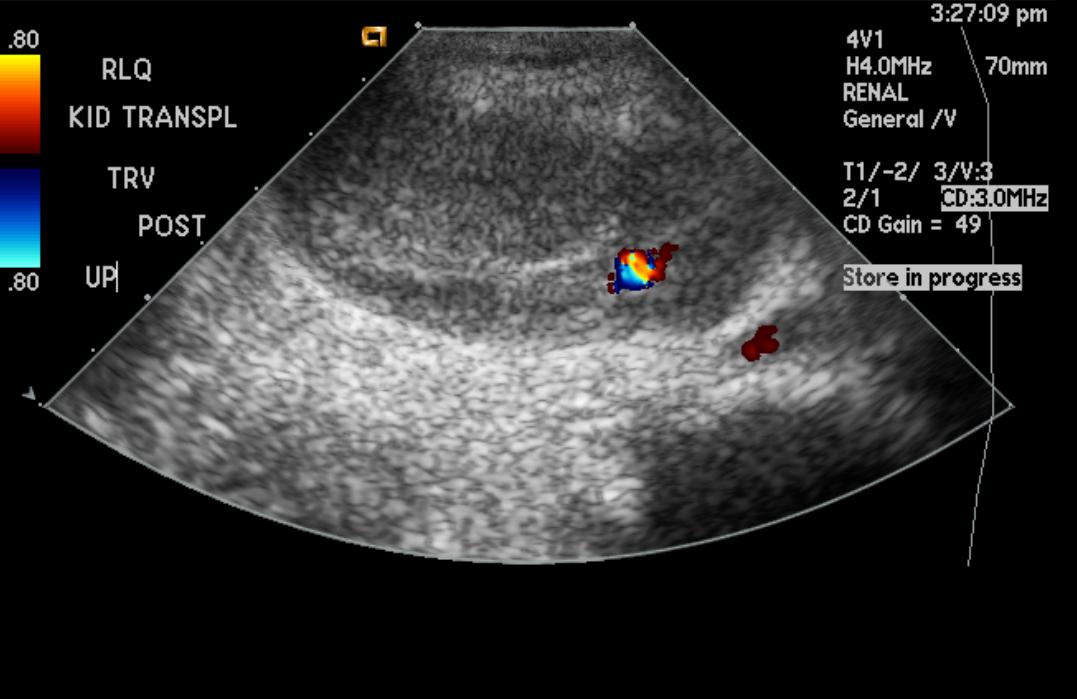
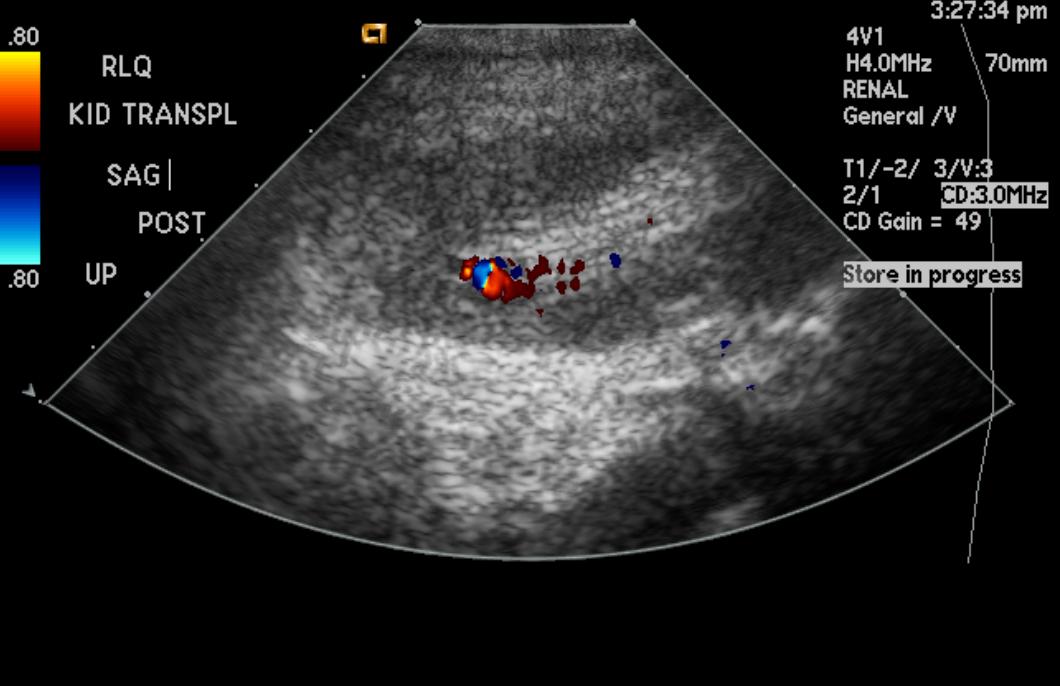
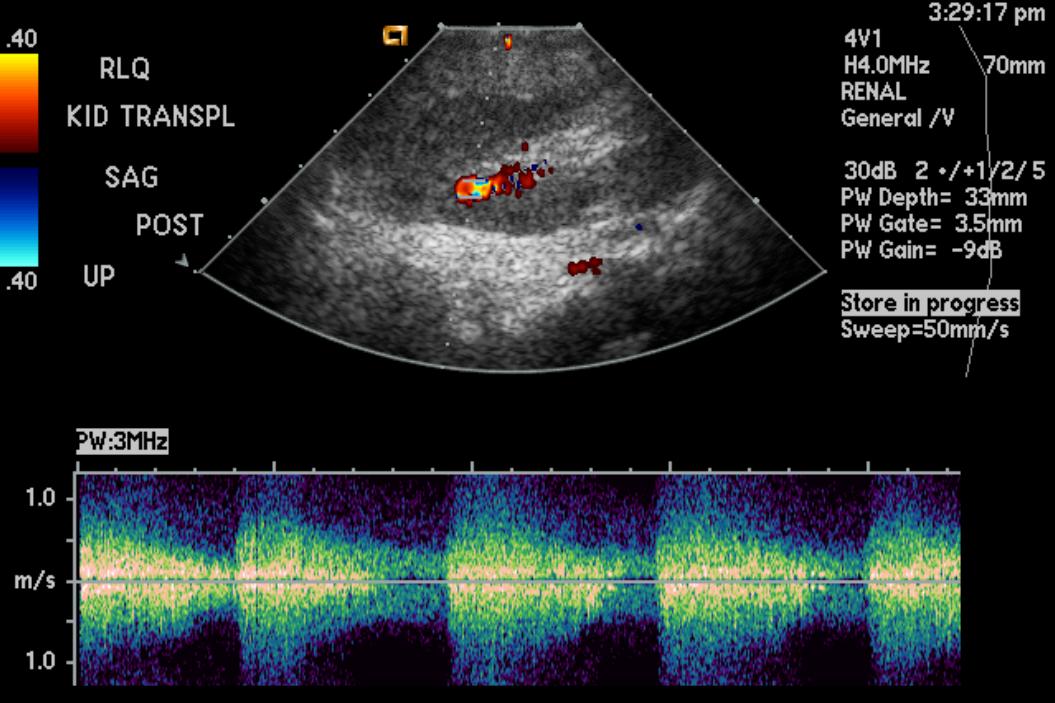
(Images shown below are courtesy of RadsWiki)
-
Renal arteriovenous fistula
-
Renal arteriovenous fistula
-
Renal arteriovenous fistula
Treatment
Congenital fistulas, if small, usually do not need treatment. Acquired fistulas can be treated by surgery.
Contraindicated medications
Compensatory hypertension due to Arteriovenous fistula is considered an absolute contraindication to the use of the following medications:
Related Chapters
External Links
{{#ev:youtube|hIw3IKB7LIs}}
{{#ev:youtube|If7lZCIpZgU}}
2008 ACC/AHA Guidelines for the Management of Adults With Congenital Heart Disease (DO NOT EDIT)
Coronary Arteriovenous Fistula (DO NOT EDIT)[16]
| Class I |
| "1. If a continuous murmur is present, its origin should be defined either by echocardiography, MRI, CT angiography, or cardiac catheterization. (Level of Evidence: C)" |
| ”2. A large coronary arteriovenous fistula (CAVF), regardless of symptomatology, should be closed via either a transcatheter or surgical route after delineation of its course and its potential to fully obliterate the fistula. (Level of Evidence: C)" |
| ”3. A small to moderate CAVF in the presence of documented myocardial ischemia, arrhythmia, otherwise unexplained ventricular systolic or diastolic dysfunction or enlargement, or endarteritis should be closed via either a transcatheter or surgical approach after delineation of its course and its potential to fully obliterate the fistula. (Level of Evidence: C)" |
| Class III |
| "1. Patients with small, asymptomatic CAVF should not undergo closure of CAVF. (Level of Evidence: C)" |
| Class IIa |
| "1. Clinical follow-up with echocardiography every 3 to 5 years can be useful for patients with small, asymptomatic CAVF to exclude development of symptoms or arrhythmias or progression of size or chamber enlargement that might alter management. (Level of Evidence: C)" |
Management Strategies for CAVF(DO NOT EDIT)[16]
| Class I |
| "1. Surgeons with training and expertise in CHD should perform operations for management of patients with CAVF. (Level of Evidence: C)" |
| ”2. Transcatheter closure of CAVF should be performed only in centers with expertise in such procedures. (Level of Evidence: C)" |
| ”3. Transcatheter delineation of CAVF course and access to distal drainage should be performed in all patients with audible continuous murmur and recognition of CAVF. (Level of Evidence: C)" |
References
- ↑ Khodadad G (January 1973). "Arteriovenous malformations of the scalp". Ann. Surg. 177 (1): 79–85. PMC 1355509. PMID 4682507.
- ↑ Liu J, Shimada Y (2014). "A Case of Intractable Left Forearm Congenital Arteriovenous Fistula Ending with Amputation: Importance of New Medical Information Obtained via the Internet". J Rural Med. 9 (1): 37–9. doi:10.2185/jrm.2878. PMC 4310049. PMID 25650050.
- ↑ 3.0 3.1 3.2 Yater WM (January 1928). "ACQUIRED ARTERIOVENOUS FISTULA". Ann. Surg. 87 (1): 19–31. PMC 1398373. PMID 17865813.
- ↑ Albeyoglu S, Aldag M, Ciloglu U, Sargin M, Oz TK, Kutlu H, Dagsali S (2017). "Coronary Arteriovenous Fistulas in Adult Patients: Surgical Management and Outcomes". Braz J Cardiovasc Surg. 32 (1): 15–21. doi:10.21470/1678-9741-2017-0005. PMC 5382904. PMID 28423125.
- ↑ Lim WH, Kang SH, Jeon K, Cho I, Kim KH, Hwang SW, Kim HK, Sohn DW (September 2009). "Asymptomatic Right Coronary Artery-to-Pulmonary Artery Fistula Incidentally Detected by Transthoracic Echocardiography". J Cardiovasc Ultrasound. 17 (3): 106–9. doi:10.4250/jcu.2009.17.3.106. PMC 2889379. PMID 20661326.
- ↑ Jang SN, Her SH, Do KR, Kim JS, Yoon HJ, Lee JM, Jin SW (December 2008). "A case of congenital bilateral coronary-to-right ventricle fistula coexisting with variant angina". Korean J. Intern. Med. 23 (4): 216–8. doi:10.3904/kjim.2008.23.4.216. PMC 2687685. PMID 19119260.
- ↑ Luke JC (April 1940). "CONGENITAL ARTERIOVENOUS FISTULA". Can Med Assoc J. 42 (4): 341–5. PMC 537854. PMID 20321666.
- ↑ Robbs JV, Carrim AA, Kadwa AM, Mars M (September 1994). "Traumatic arteriovenous fistula: experience with 202 patients". Br J Surg. 81 (9): 1296–9. PMID 7953391.
- ↑ Nagpal K, Ahmed K, Cuschieri R (2008). "Diagnosis and management of acute traumatic arteriovenous fistula". Int. J. Angiol. 17 (4): 214–6. PMC 2728918. PMID 22477453.
- ↑ Laberge JM (December 2004). "Interventional management of renal transplant arteriovenous fistula". Semin Intervent Radiol. 21 (4): 239–46. doi:10.1055/s-2004-861558. PMC 3036239. PMID 21331135.
- ↑ Abassi ZA, Winaver J, Hoffman A (October 2003). "Large A-V fistula: pathophysiological consequences and therapeutic perspectives". Curr Vasc Pharmacol. 1 (3): 347–54. PMID 15320481.
- ↑ Soumer K, Benomrane S, Derbel B, Laribi J, Benmrad M, Elleuch N, Kalfat T, Khayati A (February 2015). "Popliteal pseudoaneurysm and arteriovenous fistula after acupuncture". J Mal Vasc. 40 (1): 58–62. doi:10.1016/j.jmv.2014.11.001. PMID 25623503.
- ↑ Spetzler RF, Hargraves RW, McCormick PW, Zabramski JM, Flom RA, Zimmerman RS (June 1992). "Relationship of perfusion pressure and size to risk of hemorrhage from arteriovenous malformations". J. Neurosurg. 76 (6): 918–23. doi:10.3171/jns.1992.76.6.0918. PMID 1588424.
- ↑ Zamani H, Meragi M, Arabi Moghadam MY, Alizadeh B, Babazadeh K, Mokhtari-Esbuie F (2015). "Clinical presentation of coronary arteriovenous fistula according to age and anatomic orientation". Caspian J Intern Med. 6 (2): 108–12. PMC 4478461. PMID 26221510.
- ↑ Sapin P, Frantz E, Jain A, Nichols TC, Dehmer GJ (March 1990). "Coronary artery fistula: an abnormality affecting all age groups". Medicine (Baltimore). 69 (2): 101–13. PMID 2319939.
- ↑ 16.0 16.1 Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA; et al. (2008). "ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease). Developed in Collaboration With the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". J Am Coll Cardiol. 52 (23): e1–121. doi:10.1016/j.jacc.2008.10.001. PMID 19038677.