Aortic stenosis pathophysiology
|
Aortic Stenosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Percutaneous Aortic Balloon Valvotomy (PABV) or Aortic Valvuloplasty |
|
Transcatheter Aortic Valve Replacement (TAVR) |
|
Case Studies |
|
Aortic stenosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Aortic stenosis pathophysiology |
|
Directions to Hospitals Treating Aortic stenosis pathophysiology |
|
Risk calculators and risk factors for Aortic stenosis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editors-In-Chief: Mohammed A. Sbeih, M.D. [2], Claudia P. Hochberg, M.D. [3], Abdul-Rahman Arabi, M.D. [4], Keri Shafer, M.D. [5], Priyamvada Singh, MBBS [6]; Assistant Editor-In-Chief: Kristin Feeney, B.S. [7]
Overview
Aortic stenosis results in the onset of a chronic pressure overload of the left ventricle. As the disease progresses, an aortic stenosis can result in compromised functional integrity of the surrounding mitral valve. The most common complication of aortic stenosis is left ventricular hypertrophy. Aortic stenosis could be subvalvular, supravalvular or at the level of the aortic valve.
Pathophysiology
When the aortic valve becomes stenosed, it can result in the formation of a pressure gradient between the left ventricle (LV) and the aorta [1]. The more constricted the valve, the higher the gradient between the LV and the aorta. For instance, with a mild AS, the gradient may be 20 mmHg. This means that, at peak systole, while the LV may generate a pressure of 140 mmHg, the pressure that is transmitted to the aorta will only be 120 mmHg. So, while a blood pressure cuff may measure a normal systolic blood pressure, the actual pressure generated by the LV would be considerably higher.
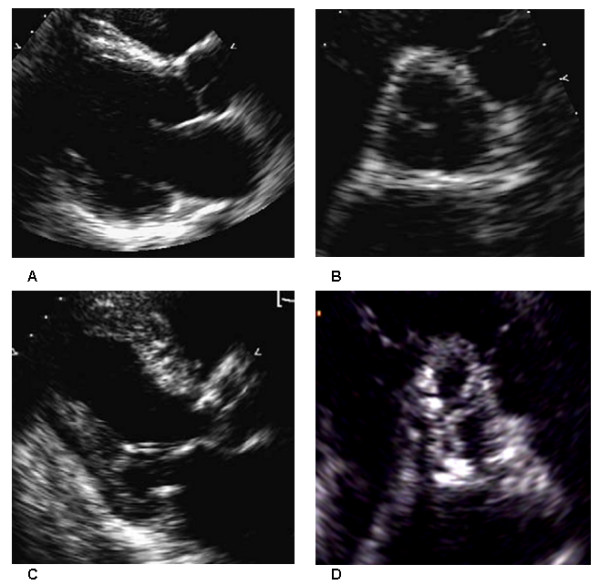
In individuals with AS, the left ventricle (LV) has to generate an increased pressure in order to overcome the increased afterload caused by the stenotic aortic valve and eject blood out of the LV. The more severe the aortic stenosis, the higher the gradient is between the left ventricular systolic pressures and the aortic systolic pressures. Due to the increased pressures generated by the left ventricle, the myocardium (muscle) of the LV undergoes hypertrophy (increase in muscle mass). This is seen as thickening of the walls of the LV. The type of hypertrophy most commonly seen in AS is concentric hypertrophy, meaning that all the walls of the LV are (approximately) equally thickened. As a result of increased the left ventricular wall thickness , the volume/mass ratio decreases, the compliance of the chamber also decreases, LV end-diastolic pressure increases without chamber dilatation [2].
Unfortunately, the adaptation to aortic stenosis by ventricular hypertrophy often carries adverse consequences. The hypertrophied heart may have reduced coronary blood flow even in the absence of coronary heart disease. This may lead to subendocardial ischemia during stress or exercise, which can contribute to systolic or diastolic dysfunction of the left ventricle [3][4]. If left ventricular systolic dysfunction occurs, this may resulting in reductions in stroke volume and cardiac output, and eventual heart failure. Another factor that may reduce ventricular function is incoordinate contraction, resulting from regional wall motion abnormalities, fibrosis or ischemia [5].
In aortic stenosis, the flow velocity across the stenosed valve is at least 2.6 m/sec. This is based upon echocardiographic estimation of the aortic jet velocity, aortic valve area and the mean transvalvular gradient. In aortic valve sclerosis; the aortic valve becomes calcified but the aortic jet velocity ≤2.5 m/sec (without a significant gradient). Aortic valve sclerosis is commonly defined as a focal or diffuse thickening of the aortic cusps with calcific nodules generally at the base of leaflets and transvalvular velocity at Doppler still in the normal range (Vmax <2 m/s). Until few years ago, it was considered a physiologic process related to aging without clinical relevance. However, aortic valve sclerosis is not observed in about 50% of people over 80 years old. Furthermore, several experimental and clinical studies have showed that it could represent an active phenomenon, significantly related to risk factors for atherosclerosis and cardiovascular morbidity and mortality [6].
.
The progressive nature of aortic valve calcification has also been confirmed. Several studies documented the rate of progression of severity of valve stenosis over time [8]; according to these reports an average reduction of 0.1 cm2 in valve area per year of follow-up is generally observed; unfortunately, there is a large variability in the rate of progression among patients. Furthermore, many factors associated with a faster progression have been identified. Of interest, among these there are hemodynamic and valve-related variables, such as left ventricular function, bicuspid type of stenosis, initial severity of stenosis, but also, and specially, risk factors for atherosclerosis, such as age, smoking, hypertension, obesity and diabetes, lipid abnormalities, chronic renal failure and dialysis, and atherosclerotic disease itself, such as concomitant coronary artery disease.
In general, symptoms in patients with aortic stenosis and normal left ventricular systolic function usually occur when:
- The valve area is <1.0 cm2.
- The jet velocity is over 4.0 m/sec.
- The mean transvalvular pressure gradient exceeds 40 mmHg.
However, many patients develop symptoms only when more severe valve obstruction is present, other patients become symptomatic at less severe degree of stenosis, particularly if there is coexisting aortic regurgitation.
In adults with AS, the obstruction develops gradually usually over decades. During this time, the left ventricle adapts to the systolic pressure overload through a hypertrophic process. However, if the hypertrophic process is inadequate and relative wall thickness does not increase in proportion to pressure, wall stress increases and the high afterload causes a decrease in ejection fraction [9]. Clinically, it is difficult to determine the cause of low ejection fraction whether it is due to depressed contractility or to excessive afterload. Corrective surgery will be more beneficial and will have better outcome when the low ejection fraction is caused by high afterload than when caused by depressed contractility of the myocardium.
ACC/AHA Guidelines- Classification of the Severity of Aortic Stenosis in Adults (DO NOT EDIT) [10]
Indicator Mild Moderate Severe Jet velocity (m per s) Less than 3.0 3.0–4.0 Greater than 4.0 Mean gradient (mm Hg)† Less than 25 25–40 Greater than 40 Valve area (cm2) Greater than 1.5 1.0–1.5 Less than 1.0 Valve area index (cm2 per m2) Less than 0.6
† Valve gradients are flow dependent and when used as estimates of severity of valve stenosis should be assessed with knowledge of cardiac output or forward flow across the valve.
Sources
- 2008 Focused Update Incorporated Into the ACC/AHA 2006 Guidelines for the Management of Patients With Valvular Heart Disease [10].
References
- ↑ Lilly LS (editor) (2003). Pathophysiology of Heart Disease (3rd ed. ed.). Lippincott Williams & Wilkins. ISBN 0-7817-4027-4.
- ↑ Gaasch WH, Levine HJ, Quinones MA, Alexander JK (1976). "Left ventricular compliance: mechanisms and clinical implications". Am J Cardiol. 38 (5): 645–53. PMID 136186.
- ↑ Marcus ML, Doty DB, Hiratzka LF, Wright CB, Eastham CL (1982). "Decreased coronary reserve: a mechanism for angina pectoris in patients with aortic stenosis and normal coronary arteries". N Engl J Med. 307 (22): 1362–6. doi:10.1056/NEJM198211253072202. PMID 6215582.
- ↑ Carabello BA (2002). "Clinical practice. Aortic stenosis". N Engl J Med. 346 (9): 677–82. doi:10.1056/NEJMcp010846. PMID 11870246.
- ↑ Jin XY, Pepper JR, Gibson DG (1996). "Effects of incoordination on left ventricular force-velocity relation in aortic stenosis". Heart. 76 (6): 495–501. PMC 484601. PMID 9014797.
- ↑ Branch KR, O'Brien KD, Otto CM (2002). "Aortic valve sclerosis as a marker of active atherosclerosis". Curr Cardiol Rep. 4 (2): 111–7. PMID 11827633.
- ↑ {{Faggiano P, D'Aloia A, Antonini-Canterin F, Pinamonti B, DiLenarda A, Brentana L, Metra M, Nodari S, Dei Cas L. Usefulness of cardiac calcification on two-dimensional echocardiography for distinguishing ischemic from nonischemic dilated cardiomyopathy: a preliminary report. J Cardiovasc Med. 2006.}}
- ↑ Faggiano P, Aurigemma GP, Rusconi C, Gaasch WH (1996). "Progression of valvular aortic stenosis in adults: literature review and clinical implications". Am Heart J. 132 (2 Pt 1): 408–17. PMID 8701905.
- ↑ Rydén L (1988). "Noninvasive techniques in the evaluation of the arrhythmogenic effects". Eur Heart J. 9 Suppl B: 19–23. PMID 3286263.
- ↑ 10.0 10.1 Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD; et al. (2008). "2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". J Am Coll Cardiol. 52 (13): e1–142. doi:10.1016/j.jacc.2008.05.007. PMID 18848134.