Aortic stenosis echocardiography: Difference between revisions
No edit summary |
|||
| (25 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{| class="infobox" style="float:right;" | |||
|- | |||
| [[File:Siren.gif|30px|link=Aortic stenosis resident survival guide]]|| <br> || <br> | |||
| [[Aortic stenosis resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] | |||
|} | |||
{{Template:Aortic stenosis}} | {{Template:Aortic stenosis}} | ||
{{CMG}}; {{AOEIC}} [[User:Mohammed Sbeih|Mohammed A. Sbeih, M.D.]] [mailto:msbeih@wikidoc.org]; {{LG}}; [[User:Rim Halaby|Rim Halaby]] | {{CMG}}; {{AOEIC}} [[User:Mohammed Sbeih|Mohammed A. Sbeih, M.D.]] [mailto:msbeih@wikidoc.org]; {{LG}}; [[User:Rim Halaby|Rim Halaby]]; {{USAMA}} | ||
==Overview== | ==Overview== | ||
[[Echocardiography]] is the best non-invasive test to evaluate the aortic valve anatomy and function. It is indicated in the case of presence of symptoms suggestive of valvular problems or in the case of detection of a systolic [[murmur]] with a grade greater than 3/6. Doppler echocardiography allows the measurement of the maximum jet velocity and can be used to estimate the effective orifice area of the [[aortic valve]] as well as the gradient across the aortic valve using the modified Bernoulli equation (gradient = 4 x velocity<sup>2</sup>). The flow must be constant, so as the velocity increases, the valve area decreases proportionally. Attention to technical details is important as they may lead to underestimation of the severity of the [[aortic stenosis]]<ref name="pmid18820172">{{cite journal| author=Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD et al.| title=2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. | journal=Circulation | year= 2008 | volume= 118 | issue= 15 | pages= e523-661 | pmid=18820172 | doi=10.1161/CIRCULATIONAHA.108.190748 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18820172 }} </ref> | [[Echocardiography]] is the best non-invasive test to evaluate the aortic valve anatomy and function. It is indicated in the case of presence of symptoms suggestive of valvular problems or in the case of detection of a systolic [[murmur]] with a grade greater than 3/6. Doppler echocardiography allows the measurement of the maximum jet velocity and can be used to estimate the effective orifice area of the [[aortic valve]] as well as the gradient across the aortic valve using the modified Bernoulli equation (gradient = 4 x velocity<sup>2</sup>). The flow must be constant, so as the velocity increases, the valve area decreases proportionally. Attention to technical details is important as they may lead to underestimation of the severity of the [[aortic stenosis]].<ref name="pmid18820172">{{cite journal| author=Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD et al.| title=2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. | journal=Circulation | year= 2008 | volume= 118 | issue= 15 | pages= e523-661 | pmid=18820172 | doi=10.1161/CIRCULATIONAHA.108.190748 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18820172 }} </ref> Echocardiography can also be used to assess the severity of [[left ventricular hypertrophy]].<ref>{{Cite journal | ||
| author = [[Christophe Martinez]], [[Anne Bernard]], [[Raluca Dulgheru]], [[Pierluigi Incarnato]], [[Cecile Oury]] & [[Patrizio Lancellotti]] | |||
| title = Pulmonary Hypertension in Aortic Stenosis and Mitral Regurgitation: Rest and Exercise Echocardiography Significance | |||
| journal = [[Progress in cardiovascular diseases]] | |||
| volume = 59 | |||
| issue = 1 | |||
| pages = 59–70 | |||
| year = 2016 | |||
| month = July-August | |||
| doi = 10.1016/j.pcad.2016.06.004 | |||
| pmid = 27389810 | |||
}}</ref> | |||
==Optimal Echocardiography Views== | ==Optimal Echocardiography Views== | ||
| Line 12: | Line 28: | ||
*Parasternal Short Axis View: | *Parasternal Short Axis View: | ||
:In the parasternal short axis view, the aortic leaflets open equally and form a circular orifice during systole. During diastole, the normal leaflets form a three pointed star with prominence at the closing point ( | :In the parasternal short axis view, the aortic leaflets open equally and form a circular orifice during systole. During diastole, the normal leaflets form a three pointed star with prominence at the closing point (nodules of Arentius). | ||
==Assessment of the Aortic Valve Area and Resistance== | ==Assessment of the Aortic Valve Area and Resistance== | ||
The assessment of Aortic Valve Area and Resistance are helpful in diagnosing Aortic Valve Stenosis. <ref>{{Cite journal | |||
| author = [[William A. Zoghbi]], [[Maurice Enriquez-Sarano]], [[Elyse Foster]], [[Paul A. Grayburn]], [[Carol D. Kraft]], [[Robert A. Levine]], [[Petros Nihoyannopoulos]], [[Catherine M. Otto]], [[Miguel A. Quinones]], [[Harry Rakowski]], [[William J. Stewart]], [[Alan Waggoner]] & [[Neil J. Weissman]] | |||
| title = Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography | |||
| journal = [[Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography]] | |||
| volume = 16 | |||
| issue = 7 | |||
| pages = 777–802 | |||
| year = 2003 | |||
| month = July | |||
| doi = 10.1016/S0894-7317(03)00335-3 | |||
| pmid = 12835667 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[J. D. Carroll]], [[E. P. Carroll]], [[T. Feldman]], [[D. M. Ward]], [[R. M. Lang]], [[D. McGaughey]] & [[R. B. Karp]] | |||
| title = Sex-associated differences in left ventricular function in aortic stenosis of the elderly | |||
| journal = [[Circulation]] | |||
| volume = 86 | |||
| issue = 4 | |||
| pages = 1099–1107 | |||
| year = 1992 | |||
| month = October | |||
| pmid = 1394918 | |||
}}</ref> | |||
*Based on [[Bernoulli equation|Bernoulli's equation]], using doppler echocardiography the [[Intravascular pressure gradient|pressure gradient]] across the valve can be measured using the formula: <blockquote>[[Intravascular pressure gradient|Pressure Gradient]] ([[mmHg]]) = 4 x (Maximum Stenotic Jet Velocity)<sup>2</sup> - 4 x ([[LVOT|Left Ventricular Outflow Tract Velocity]])<sup>2</sup></blockquote> | *Based on [[Bernoulli equation|Bernoulli's equation]], using doppler echocardiography the [[Intravascular pressure gradient|pressure gradient]] across the valve can be measured using the formula: <blockquote>[[Intravascular pressure gradient|Pressure Gradient]] ([[mmHg]]) = 4 x (Maximum Stenotic Jet Velocity)<sup>2</sup> - 4 x ([[LVOT|Left Ventricular Outflow Tract Velocity]])<sup>2</sup></blockquote> | ||
| Line 22: | Line 60: | ||
===Assessment of the Aortic Valve Area=== | ===Assessment of the Aortic Valve Area=== | ||
*The | Following are a few important points regarding the Aortic Valve Area Assessment.<ref>{{Cite journal | ||
| author = [[William A. Zoghbi]], [[Maurice Enriquez-Sarano]], [[Elyse Foster]], [[Paul A. Grayburn]], [[Carol D. Kraft]], [[Robert A. Levine]], [[Petros Nihoyannopoulos]], [[Catherine M. Otto]], [[Miguel A. Quinones]], [[Harry Rakowski]], [[William J. Stewart]], [[Alan Waggoner]] & [[Neil J. Weissman]] | |||
| title = Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography | |||
| journal = [[Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography]] | |||
| volume = 16 | |||
| issue = 7 | |||
| pages = 777–802 | |||
| year = 2003 | |||
| month = July | |||
| doi = 10.1016/S0894-7317(03)00335-3 | |||
| pmid = 12835667 | |||
}}</ref> | |||
*The [[Aortic valve area calculation#Continuity Equation|continuity principle]] states that the flow in one area must equal the flow in a second area if there are no shunts in between the two areas. | |||
*Using doppler velocities, aortic valve area can be calculated using the following continuity pinciple:<ref name="pmid19130998">{{cite journal |author=Baumgartner H, Hung J, Bermejo J, Chambers JB, Evangelista A, Griffin BP, Iung B, Otto CM, Pellikka PA, Quiñones M |title=Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice |journal=[[Journal of the American Society of Echocardiography : Official Publication of the American Society of Echocardiography]] |volume=22 |issue=1 |pages=1–23; quiz 101–2 |year=2009 |month=January |pmid=19130998 |doi=10.1016/j.echo.2008.11.029 |url=http://linkinghub.elsevier.com/retrieve/pii/S0894-7317(08)00776-1 |accessdate=2012-04-13}}</ref> | *Using doppler velocities, aortic valve area can be calculated using the following continuity pinciple:<ref name="pmid19130998">{{cite journal |author=Baumgartner H, Hung J, Bermejo J, Chambers JB, Evangelista A, Griffin BP, Iung B, Otto CM, Pellikka PA, Quiñones M |title=Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice |journal=[[Journal of the American Society of Echocardiography : Official Publication of the American Society of Echocardiography]] |volume=22 |issue=1 |pages=1–23; quiz 101–2 |year=2009 |month=January |pmid=19130998 |doi=10.1016/j.echo.2008.11.029 |url=http://linkinghub.elsevier.com/retrieve/pii/S0894-7317(08)00776-1 |accessdate=2012-04-13}}</ref> | ||
| Line 38: | Line 89: | ||
==Severity of Aortic Stenosis== | ==Severity of Aortic Stenosis== | ||
Aortic stenosis severity can be assessed by estimating both the pressure gradient across the valve and the [[aortic valve area]]. | Aortic stenosis severity can be assessed by estimating both the pressure gradient across the valve and the [[aortic valve area]].<ref>{{Cite journal | ||
| author = [[C. M. Otto]], [[I. G. Burwash]], [[M. E. Legget]], [[B. I. Munt]], [[M. Fujioka]], [[N. L. Healy]], [[C. D. Kraft]], [[C. Y. Miyake-Hull]] & [[R. G. Schwaegler]] | |||
| title = Prospective study of asymptomatic valvular aortic stenosis. Clinical, echocardiographic, and exercise predictors of outcome | |||
| journal = [[Circulation]] | |||
| volume = 95 | |||
| issue = 9 | |||
| pages = 2262–2270 | |||
| year = 1997 | |||
| month = May | |||
| pmid = 9142003 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[William A. Zoghbi]], [[Maurice Enriquez-Sarano]], [[Elyse Foster]], [[Paul A. Grayburn]], [[Carol D. Kraft]], [[Robert A. Levine]], [[Petros Nihoyannopoulos]], [[Catherine M. Otto]], [[Miguel A. Quinones]], [[Harry Rakowski]], [[William J. Stewart]], [[Alan Waggoner]] & [[Neil J. Weissman]] | |||
| title = Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography | |||
| journal = [[Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography]] | |||
| volume = 16 | |||
| issue = 7 | |||
| pages = 777–802 | |||
| year = 2003 | |||
| month = July | |||
| doi = 10.1016/S0894-7317(03)00335-3 | |||
| pmid = 12835667 | |||
}}</ref> | |||
*Using echocardiographic flow velocities, the [[aortic valve area]] can be calculated non-invasively to estimate the severity of [[aortic stenosis]]. | *Using echocardiographic flow velocities, the [[aortic valve area]] can be calculated non-invasively to estimate the severity of [[aortic stenosis]]. | ||
*Using the velocity of the blood through the valve, the pressure gradient across the valve can be calculated by the equation: <blockquote>Gradient = 4(velocity)² | *Using the velocity of the blood through the valve, the pressure gradient across the valve can be calculated by the equation: <blockquote>Gradient = 4(velocity)² mm Hg</blockquote> | ||
====Normal Aortic Valve==== | ====Normal Aortic Valve==== | ||
| Line 66: | Line 138: | ||
*Jet velocity is greater than 4.0 m per second | *Jet velocity is greater than 4.0 m per second | ||
'''Shown below is a table that summarizes the criteria for the classification of aortic stenosis into mild, moderate or severe:''' | |||
{| class="wikitable" border = 1 | {| class="wikitable" border = 1 | ||
| Line 77: | Line 150: | ||
| Jet Velocity (m/s) || 2 - 3 || 3 - 4 || >4 | | Jet Velocity (m/s) || 2 - 3 || 3 - 4 || >4 | ||
|- | |- | ||
| Peak Gradient ( | | Peak Gradient (mm Hg)|| <25 || 25 - 40 || >40 | ||
|- | |- | ||
| Mean Gradient ( | | Mean Gradient (mm Hg) || <20 || 20-40 || >40 | ||
|} | |} | ||
==Low Flow, Low Gradient Aortic Stenosis== | ==Low Flow, Low Gradient Aortic Stenosis== | ||
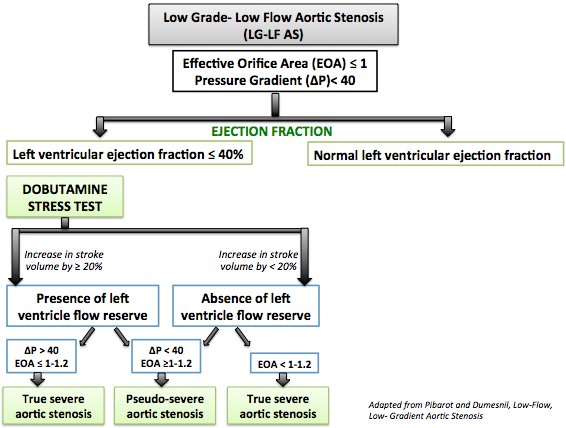
*Echocardiography is fairly accurate in the assessment of the severity of aortic stenosis in patients with normal or near normal [[cardiac output]]. However, [[Exercise stress testing#Exercise/Pharmacologic Stress Echocardiography|dobutamine stress echocardiography]] or [[Aortic stenosis cardiac catheterization|cardiac catheterization]] may be required to accurately assess the severity of aortic stenosis in patients with [[cardiac output|low output]] [[aortic stenosis]]. | *Echocardiography is fairly accurate in the assessment of the severity of aortic stenosis in patients with normal or near normal [[cardiac output]]. However, [[Exercise stress testing#Exercise/Pharmacologic Stress Echocardiography|dobutamine stress echocardiography]] or [[Aortic stenosis cardiac catheterization|cardiac catheterization]] may be required to accurately assess the severity of aortic stenosis in patients with [[cardiac output|low output]] [[aortic stenosis]].<ref>{{Cite journal | ||
*Low dose (<20 | | author = [[Silvia Aguiar Rosa]], [[Luisa Moura Branco]], [[Ana Galrinho]], [[Guilherme Portugal]], [[Joao Abreu]], [[Duarte Cacela]], [[Jose Fragata]] & [[Rui Cruz Ferreira]] | ||
| title = Contribution of Dobutamine Stress Echocardiography to the Diagnosis and Prognosis of Low-Flow/Low-Gradient Aortic Stenosis | |||
| journal = [[The Journal of heart valve disease]] | |||
| volume = 25 | |||
| issue = 2 | |||
| pages = 130–138 | |||
| year = 2016 | |||
| month = March | |||
| pmid = 27989054 | |||
}}</ref> | |||
*Low dose (<20 micro-gram/Kg/min) [[dobutamine stress echocardiography]] allows: | |||
** The differentiation between severe and pseudo-severe low flow low gradient aortic stenosis through the degree of change of both the [[aortic valve area|effective orifice area]] and the transvalvular gradient after dobutamine infusion. Changes following dobutamine infusion are due to the fact that dobutamine causes increase in the flow across the [[aortic valve]]. | ** The differentiation between severe and pseudo-severe low flow low gradient aortic stenosis through the degree of change of both the [[aortic valve area|effective orifice area]] and the transvalvular gradient after dobutamine infusion. Changes following dobutamine infusion are due to the fact that dobutamine causes increase in the flow across the [[aortic valve]]. | ||
***In pseudosevere aortic stenosis, there is increase in the [[aortic valve area|effective orifice area]] of the [[aortic valve]], in a way that it is larger than 1.2 cm<sup>2</sup>, and slight increase in the gradient, in a way that is inferior to 40 | ***In pseudosevere aortic stenosis, there is increase in the [[aortic valve area|effective orifice area]] of the [[aortic valve]], in a way that it is larger than 1.2 cm<sup>2</sup>, and slight increase in the gradient, in a way that is inferior to 40 mm Hg. | ||
***In severe aortic stenosis, there is absence or little increase in the [[aortic valve area|effective orifice area]] of the [[aortic valve]], in a way that is inferior to 1.2 cm<sup>2</sup>, and increase in the gradient to become greater than 40 | ***In severe aortic stenosis, there is absence or little increase in the [[aortic valve area|effective orifice area]] of the [[aortic valve]], in a way that is inferior to 1.2 cm<sup>2</sup>, and increase in the gradient to become greater than 40 mm Hg. | ||
** The assessment of the presence or absence of left ventricular flow reserve through the degree of change in stroke volume following dobutamine infusion. | ** The assessment of the presence or absence of left ventricular flow reserve through the degree of change in stroke volume following dobutamine infusion. | ||
***Left ventricular flow reserve is an indicator of operative mortality. Left ventricle flow reserve does not predict recovery of left ventricle after aortic valve replacement nor the resolution of symptoms.<ref name="pmid23062546">{{cite journal| author=Pibarot P, Dumesnil JG| title=Low-flow, low-gradient aortic stenosis with normal and depressed left ventricular ejection fraction. | journal=J Am Coll Cardiol | year= 2012 | volume= 60 | issue= 19 | pages= 1845-53 | pmid=23062546 | doi=10.1016/j.jacc.2012.06.051 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23062546 }} </ref> | ***Left ventricular flow reserve is an indicator of operative mortality. Left ventricle flow reserve does not predict recovery of left ventricle after aortic valve replacement nor the resolution of symptoms.<ref name="pmid23062546">{{cite journal| author=Pibarot P, Dumesnil JG| title=Low-flow, low-gradient aortic stenosis with normal and depressed left ventricular ejection fraction. | journal=J Am Coll Cardiol | year= 2012 | volume= 60 | issue= 19 | pages= 1845-53 | pmid=23062546 | doi=10.1016/j.jacc.2012.06.051 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23062546 }} </ref> | ||
***The [[aortic valve area]] should increase to more than 1-1.2 cm<sup>2</sup> with a dobutamine infusion and the [[Intravascular pressure gradient|mean pressure gradient]] should rise above 30 mm Hg. While early surgical mortality is | ***The [[aortic valve area]] should increase to more than 1-1.2 cm<sup>2</sup> with a dobutamine infusion and the [[Intravascular pressure gradient|mean pressure gradient]] should rise above 30 mm Hg. While early surgical mortality is 32–33% in patients who fail to to achieve these improvements with dobutamine infusions, it is only 5–7% in patients who demonstrate an increase in their contractility and gradient. Five years survival after surgery was 88% in patients with improved contractility and only 10–25% in patients with unimproved contractility. | ||
'''Shown below is an algorithm summarizing the interpretation of the results of low dose dobutamine stress echocardiography in the evaluation of low flow, low gradient aortic stenosis:''' | |||
[[Image:Diagnosis_of_LGLFAS.png|center|500px|Evaluation of low flow, low gradient aortic stenosis by low dose dobutamine stress echocardiography]] | [[Image:Diagnosis_of_LGLFAS.png|center|500px|Evaluation of low flow, low gradient aortic stenosis by low dose dobutamine stress echocardiography]] | ||
== | ==Utilisation of Echocardiography== | ||
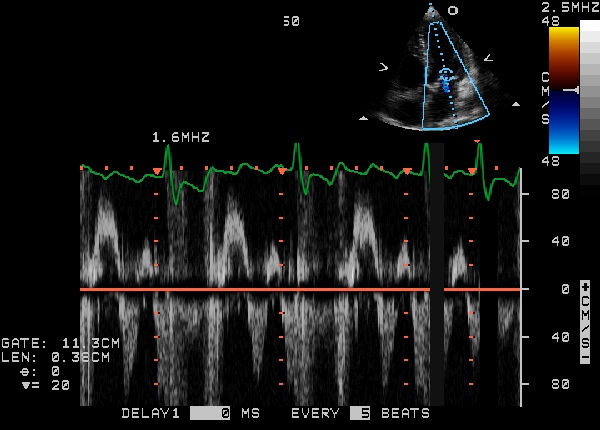
=====Demonstration of Diastolic Mitral Regurgitation due to Severe Aortic Stenosis===== | =====Demonstration of Diastolic Mitral Regurgitation due to Severe Aortic Stenosis:===== | ||
[[Image:Diastolic_MR_Due_to_AS.jpg|425px|left|Diastolic mitral regurgitation due to severe aortic stenosis]] | [[Image:Diastolic_MR_Due_to_AS.jpg|425px|left|Diastolic mitral regurgitation due to severe aortic stenosis]] | ||
<br clear="left"/> | <br clear="left"/> | ||
=====Demonstration of Aortic regurgitation combined with Aortic Stenosis===== | =====Demonstration of Aortic regurgitation combined with Aortic Stenosis:===== | ||
{{#ev:youtube|J-Qs_evodww}} | {{#ev:youtube|J-Qs_evodww}} | ||
=====Demonstration of Calcific Aortic Stenosis with Mitral Annular Calcification and Moderate Mitral Regurgitation===== | =====Demonstration of Calcific Aortic Stenosis with Mitral Annular Calcification and Moderate Mitral Regurgitation:===== | ||
{{#ev:youtube|qjpV19034sk}} | {{#ev:youtube|qjpV19034sk}} | ||
=====Low flow Aortic Stenosis===== | =====Low flow Aortic Stenosis:===== | ||
{{#ev:youtube|WC3uKS4ShSM&feature=related}} | {{#ev:youtube|WC3uKS4ShSM&feature=related}} | ||
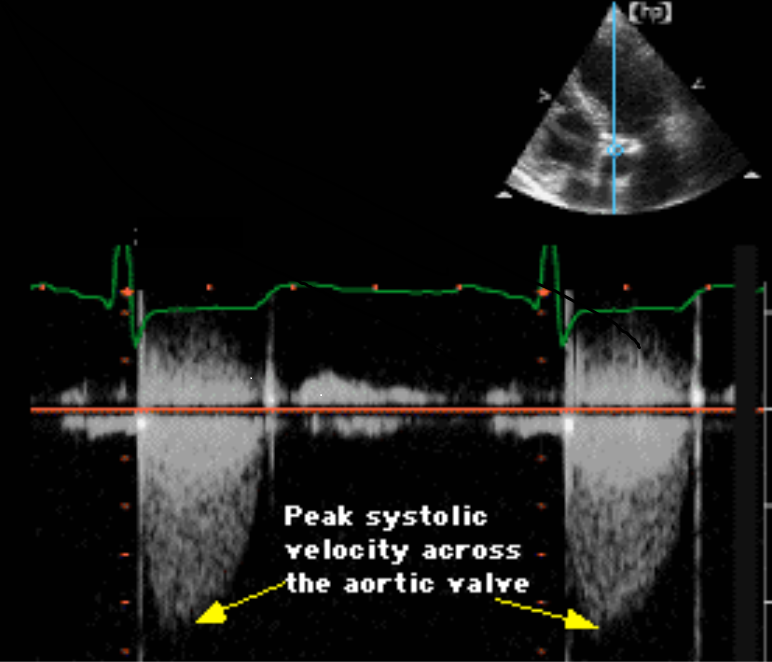
=====Severe Aortic Stenosis without Aortic Regurgitation===== | =====Severe Aortic Stenosis without Aortic Regurgitation:===== | ||
Continuous wave Doppler below shows a peak velocity across the aortic valve of a gradient of 85 mm Hg, which is compatible with severe aortic stenosis. No aortic regurgitation is present. | |||
[[Image:aortic stenosis echocardiography.png|left|425px]] | [[Image:aortic stenosis echocardiography.png|left|425px]] | ||
<br clear="left"/> | <br clear="left"/> | ||
== 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines<ref name="pmid33332150">{{cite journal| author=Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP, Gentile F | display-authors=etal| title=2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. | journal=Circulation | year= 2021 | volume= 143 | issue= 5 | pages= e72-e227 | pmid=33332150 | doi=10.1161/CIR.0000000000000923 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=33332150 }}</ref> == | |||
=== Recommendations for Diagnostic Testing: Initial Diagnosis of AS Referenced studies that support the recommendations are summarized in the Online Data Supplement === | |||
{| class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen" |[[EHS ESC guidelines classification scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen" |1. In patients with signs or symptoms of AS or a BAV, TTE is indicated for accurate diagnosis of the cause of AS, assessment of hemodynamic severity, measurement of LV size and systolic function, and determination of prognosis and timing of valve intervention([[ACC AHA guidelines classification scheme#Level of Evidence|''Level of Evidence: A'']]) | |||
2. In patients with suspected low-flow, low-gradient severe AS with normal LVEF (Stage D3), optimization of blood pressure control is recommended before measurement of AS severity by TTE, TEE, cardiac catheterization, or CMR.([[ACC AHA guidelines classification scheme#Level of Evidence|''Level of Evidence: B-NR'']]) | |||
|} | |||
{| class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon" |[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class IIa]] | |||
|- | |||
| bgcolor="LemonChiffon" | | |||
3. In patients with suspected low-flow, low-gradient severe AS with reduced LVEF (Stage D2), low-dose dobutamine stress testing with echocardiographic or invasive hemodynamic measurements is reasonable to further define severity and assess contractile reserve.([[ACC AHA guidelines classification scheme#Level of Evidence|''Level of Evidence: B-NR'']]) | |||
|} | |||
==AHA/ACC 2014 Guideline for the Management of Patients With Valvular Heart Diseases== | |||
===Diagnosis and Follow-Up=== | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen"|[[EHS ESC guidelines classification scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''1. '''TTE is indicated in patients with signs or symptoms of AS or a bicuspid aortic valve for accurate diagnosis of the cause of AS, hemodynamic severity, LV size, and systolic function, and for determining prognosis and timing of valve intervention. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B]])''<nowiki>"</nowiki> | |||
|- | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class IIa]] | |||
|- | |||
|bgcolor="LemonChiffon"| | |||
<nowiki>"</nowiki>'''1.''' Low-dose dobutamine stress testing using echocardiographic or invasive hemodynamic measurements is reasonable in patients with stage D2 AS with all of the following:<br> | |||
a. Calcified aortic valve with reduced systolic opening;<br> | |||
b. [[LVEF]] less than 50%;<br> | |||
c. Calculated valve area 1.0 cm2 or less; and<br> | |||
d. Aortic velocity less than 4.0 m per second or mean pressure gradient less than 40 mm Hg. ([[ACC AHA guidelines classification scheme#Level of Evidence|''Level of Evidence: B'']])<nowiki>"</nowiki> | |||
|- | |||
|} | |||
==2008 and Incorporated 2006 ACC/AHA Guidelines for the Management of Patients with Valvular Heart Disease (DO NOT EDIT) <ref name="pmid18820172">{{cite journal |author=Bonow RO, Carabello BA, Chatterjee K, ''et al.'' |title=2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons |journal=Circulation |volume=118 |issue=15 |pages=e523–661 |year=2008 |month=October |pmid=18820172 |doi=10.1161/CIRCULATIONAHA.108.190748 |url=}}</ref>== | ==2008 and Incorporated 2006 ACC/AHA Guidelines for the Management of Patients with Valvular Heart Disease (DO NOT EDIT) <ref name="pmid18820172">{{cite journal |author=Bonow RO, Carabello BA, Chatterjee K, ''et al.'' |title=2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons |journal=Circulation |volume=118 |issue=15 |pages=e523–661 |year=2008 |month=October |pmid=18820172 |doi=10.1161/CIRCULATIONAHA.108.190748 |url=}}</ref>== | ||
| Line 151: | Line 279: | ||
|} | |} | ||
== | ==2017 ESC/EACTS Guidelines for the Management of Valvular Heart Disease== | ||
===Stepwise Approach for the Assessment of Aortic Stenosis Severity=== | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[CME Category::Cardiology]] | |||
[[Category:Disease]] | [[Category:Disease]] | ||
| Line 163: | Line 295: | ||
[[Category:Cardiac surgery]] | [[Category:Cardiac surgery]] | ||
[[Category:Surgery]] | [[Category:Surgery]] | ||
Latest revision as of 03:32, 8 December 2022
| Resident Survival Guide |
|
Aortic Stenosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Percutaneous Aortic Balloon Valvotomy (PABV) or Aortic Valvuloplasty |
|
Transcatheter Aortic Valve Replacement (TAVR) |
|
Case Studies |
|
Aortic stenosis echocardiography On the Web |
|
American Roentgen Ray Society Images of Aortic stenosis echocardiography |
|
Directions to Hospitals Treating Aortic stenosis echocardiography |
|
Risk calculators and risk factors for Aortic stenosis echocardiography |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Mohammed A. Sbeih, M.D. [2]; Lakshmi Gopalakrishnan, M.B.B.S. [3]; Rim Halaby; Usama Talib, BSc, MD [4]
Overview
Echocardiography is the best non-invasive test to evaluate the aortic valve anatomy and function. It is indicated in the case of presence of symptoms suggestive of valvular problems or in the case of detection of a systolic murmur with a grade greater than 3/6. Doppler echocardiography allows the measurement of the maximum jet velocity and can be used to estimate the effective orifice area of the aortic valve as well as the gradient across the aortic valve using the modified Bernoulli equation (gradient = 4 x velocity2). The flow must be constant, so as the velocity increases, the valve area decreases proportionally. Attention to technical details is important as they may lead to underestimation of the severity of the aortic stenosis.[1] Echocardiography can also be used to assess the severity of left ventricular hypertrophy.[2]
Optimal Echocardiography Views
- Parasternal Long Axis View:
- The parasternal long axis view visualizes the right and non coronary leaflets.
- Parasternal Short Axis View:
- In the parasternal short axis view, the aortic leaflets open equally and form a circular orifice during systole. During diastole, the normal leaflets form a three pointed star with prominence at the closing point (nodules of Arentius).
Assessment of the Aortic Valve Area and Resistance
The assessment of Aortic Valve Area and Resistance are helpful in diagnosing Aortic Valve Stenosis. [3][4]
- Based on Bernoulli's equation, using doppler echocardiography the pressure gradient across the valve can be measured using the formula:
Pressure Gradient (mmHg) = 4 x (Maximum Stenotic Jet Velocity)2 - 4 x (Left Ventricular Outflow Tract Velocity)2
- However, for all practical purposes, since the left ventricular outflow tract velocity is usually less than 1 m/sec; the above equation can be simplified into:
Maximum Pressure Gradient (mmHg) = 4 x (Maximum stenotic Jet Velocity)2
- The above two equations derived, aid in calculating the maximum pressure gradient that is obtained using the instantaneous aortic jet velocity that is assessed with doppler echocardiography; however, cardiac catheterization is required to calculate peak pressure gradient across the valve.
Assessment of the Aortic Valve Area
Following are a few important points regarding the Aortic Valve Area Assessment.[5]
- The continuity principle states that the flow in one area must equal the flow in a second area if there are no shunts in between the two areas.
- Using doppler velocities, aortic valve area can be calculated using the following continuity pinciple:[6]
Aortic Valve Area (cms2) = { (Cross-sectional Area of LVOT x Time Velocity Integral across the LVOT) ÷ (Time Velocity Integral across Aortic Valve) }
- The weakest aspect of this calculation is the variability in measurement of cross-sectional area of LVOT, because it involves squaring the LVOT dimension. Such variations in the aortic valve area derived using doppler velocities may be observed during exercise[7] or in conditions that increase the blood flow across the valve.[8][9]
- Based on a study that simultaneously determined Gorlin formula and transesophageal echocardiography planimetry valve areas, demonstrated that acute changes in trans-valvular blood flow substantially altered valve area as calculated by the Gorlin formula but did not result in significant alterations of the anatomic valve area in aortic stenosis. This suggests that the flow-related variation in the Gorlin aortic valve area may be due to a disproportionate blood flow dependence of the formula itself and not a true change in valve area.[10] Therefore, the advantage of continuity equation over Gorlin formula is that the former is less susceptible to blood flow across the valve.
Assessment of the Aortic Valve Resistance
- Doppler derived aortic valve resistance correlates well with catheterization derived aortic valve resistance and hence may provide an additional non-invasive parameter for the assessment of aortic stenosis severity.[11]
- Although all doppler echocardiographic indexes of aortic stenosis are affected by blood flow, aortic valve resistance is more stable than aortic valve area under dobutamine-induced hemodynamic changes. However, baseline aortic valve area may be unreliable in patients with calcific degenerative aortic stenosis and low cardiac output states.[12]
Severity of Aortic Stenosis
Aortic stenosis severity can be assessed by estimating both the pressure gradient across the valve and the aortic valve area.[13][14]
- Using echocardiographic flow velocities, the aortic valve area can be calculated non-invasively to estimate the severity of aortic stenosis.
- Using the velocity of the blood through the valve, the pressure gradient across the valve can be calculated by the equation:
Gradient = 4(velocity)² mm Hg
Normal Aortic Valve
- A normal aortic valve has no gradient, and
- Aortic valve surface area is of 2.5 to 3.5 cms2
Mild Aortic Stenosis
- Mean pressure gradient across the valve is less than 25 mm Hg, or
- Valve surface area is between 1.5 and 2.5 cms2, or
- Jet velocity less than 3.0 m per second
Moderate Aortic Stenosis
- Mean pressure gradient across the valve is between 25 mm Hg and 40 mm Hg, or
- Valve surface area is between 1.0 and 1.5 cms2, or
- Jet velocity 3.0 to 4.0 m per second
Moderate to Severe Aortic Stenosis
- Valve surface area is between 0.7 and 1.0 cms2
Severe Aortic Stenosis
- Mean pressure gradient across the valve is more than 40 mm Hg, or
- Valve surface area is less than 0.7 cm2, or
- Jet velocity is greater than 4.0 m per second
Shown below is a table that summarizes the criteria for the classification of aortic stenosis into mild, moderate or severe:
| Severity | mild | moderate | severe |
|---|---|---|---|
| Valve Surface Area | 2.5 - 1.5 | 1.5 - 1.0 | <1.0 |
| Jet Velocity (m/s) | 2 - 3 | 3 - 4 | >4 |
| Peak Gradient (mm Hg) | <25 | 25 - 40 | >40 |
| Mean Gradient (mm Hg) | <20 | 20-40 | >40 |
Low Flow, Low Gradient Aortic Stenosis
- Echocardiography is fairly accurate in the assessment of the severity of aortic stenosis in patients with normal or near normal cardiac output. However, dobutamine stress echocardiography or cardiac catheterization may be required to accurately assess the severity of aortic stenosis in patients with low output aortic stenosis.[15]
- Low dose (<20 micro-gram/Kg/min) dobutamine stress echocardiography allows:
- The differentiation between severe and pseudo-severe low flow low gradient aortic stenosis through the degree of change of both the effective orifice area and the transvalvular gradient after dobutamine infusion. Changes following dobutamine infusion are due to the fact that dobutamine causes increase in the flow across the aortic valve.
- In pseudosevere aortic stenosis, there is increase in the effective orifice area of the aortic valve, in a way that it is larger than 1.2 cm2, and slight increase in the gradient, in a way that is inferior to 40 mm Hg.
- In severe aortic stenosis, there is absence or little increase in the effective orifice area of the aortic valve, in a way that is inferior to 1.2 cm2, and increase in the gradient to become greater than 40 mm Hg.
- The assessment of the presence or absence of left ventricular flow reserve through the degree of change in stroke volume following dobutamine infusion.
- Left ventricular flow reserve is an indicator of operative mortality. Left ventricle flow reserve does not predict recovery of left ventricle after aortic valve replacement nor the resolution of symptoms.[16]
- The aortic valve area should increase to more than 1-1.2 cm2 with a dobutamine infusion and the mean pressure gradient should rise above 30 mm Hg. While early surgical mortality is 32–33% in patients who fail to to achieve these improvements with dobutamine infusions, it is only 5–7% in patients who demonstrate an increase in their contractility and gradient. Five years survival after surgery was 88% in patients with improved contractility and only 10–25% in patients with unimproved contractility.
- The differentiation between severe and pseudo-severe low flow low gradient aortic stenosis through the degree of change of both the effective orifice area and the transvalvular gradient after dobutamine infusion. Changes following dobutamine infusion are due to the fact that dobutamine causes increase in the flow across the aortic valve.
Shown below is an algorithm summarizing the interpretation of the results of low dose dobutamine stress echocardiography in the evaluation of low flow, low gradient aortic stenosis:
Utilisation of Echocardiography
Demonstration of Diastolic Mitral Regurgitation due to Severe Aortic Stenosis:
Demonstration of Aortic regurgitation combined with Aortic Stenosis:
{{#ev:youtube|J-Qs_evodww}}
Demonstration of Calcific Aortic Stenosis with Mitral Annular Calcification and Moderate Mitral Regurgitation:
{{#ev:youtube|qjpV19034sk}}
Low flow Aortic Stenosis:
{{#ev:youtube|WC3uKS4ShSM&feature=related}}
Severe Aortic Stenosis without Aortic Regurgitation:
Continuous wave Doppler below shows a peak velocity across the aortic valve of a gradient of 85 mm Hg, which is compatible with severe aortic stenosis. No aortic regurgitation is present.
2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines[17]
Recommendations for Diagnostic Testing: Initial Diagnosis of AS Referenced studies that support the recommendations are summarized in the Online Data Supplement
| Class I |
| 1. In patients with signs or symptoms of AS or a BAV, TTE is indicated for accurate diagnosis of the cause of AS, assessment of hemodynamic severity, measurement of LV size and systolic function, and determination of prognosis and timing of valve intervention(Level of Evidence: A)
2. In patients with suspected low-flow, low-gradient severe AS with normal LVEF (Stage D3), optimization of blood pressure control is recommended before measurement of AS severity by TTE, TEE, cardiac catheterization, or CMR.(Level of Evidence: B-NR) |
| Class IIa |
|
3. In patients with suspected low-flow, low-gradient severe AS with reduced LVEF (Stage D2), low-dose dobutamine stress testing with echocardiographic or invasive hemodynamic measurements is reasonable to further define severity and assess contractile reserve.(Level of Evidence: B-NR) |
AHA/ACC 2014 Guideline for the Management of Patients With Valvular Heart Diseases
Diagnosis and Follow-Up
| Class I |
| "1. TTE is indicated in patients with signs or symptoms of AS or a bicuspid aortic valve for accurate diagnosis of the cause of AS, hemodynamic severity, LV size, and systolic function, and for determining prognosis and timing of valve intervention. (Level of Evidence: B)" |
| Class IIa |
|
"1. Low-dose dobutamine stress testing using echocardiographic or invasive hemodynamic measurements is reasonable in patients with stage D2 AS with all of the following: |
2008 and Incorporated 2006 ACC/AHA Guidelines for the Management of Patients with Valvular Heart Disease (DO NOT EDIT) [1]
Echocardiography (DO NOT EDIT) [1]
| Class I |
| "1. Echocardiography is recommended for the diagnosis and assessment of aortic stenosis severity. (Level of Evidence: B)" |
| "2. Echocardiography is recommended in patients with aortic stenosis for the assessment of left ventricular wall thickness, size, and function. (Level of Evidence: B)" |
| "3. Echocardiography is recommended for re-evaluation of patients with known aortic stenosis and changing symptoms or signs. (Level of Evidence: B)" |
| "4. Echocardiography is recommended for the assessment of changes in hemodynamic severity and left ventricular function in patients with known aortic stenosis during pregnancy. (Level of Evidence: B)" |
| "5. Transthoracic echocardiography is recommended for re-evaluation of asymptomatic patients: every year for severe aortic stenosis; every 1 to 2 years for moderate aortic stenosis; and every 3 to 5 years for mild aortic stenosis. (Level of Evidence: B)" |
| Class IIa |
|
"1. Dobutamine stress echocardiography is reasonable to evaluate patients with low-flow/low-gradient AS and LV dysfunction. (Level of Evidence: B)" |
Asymptomatic Adolescents (DO NOT EDIT) [1]
| Class I |
| "1. Doppler echocardiography is recommended yearly in the asymptomatic adolescent or young adult with AS who has a Doppler mean gradient greater than 30 mm Hg or a peak velocity greater than 3.5 m per second (peak gradient greater than 50 mm Hg) and every 2 years if the Doppler gradient is less than or equal to 30 mm Hg or the peak jet velocity is less than or equal to 3.5 m per second (peak gradient less than or equal to 50 mm Hg). (Level of Evidence: C)" |
2017 ESC/EACTS Guidelines for the Management of Valvular Heart Disease
Stepwise Approach for the Assessment of Aortic Stenosis Severity
References
- ↑ 1.0 1.1 1.2 1.3 Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD; et al. (2008). "2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 118 (15): e523–661. doi:10.1161/CIRCULATIONAHA.108.190748. PMID 18820172.
- ↑ Christophe Martinez, Anne Bernard, Raluca Dulgheru, Pierluigi Incarnato, Cecile Oury & Patrizio Lancellotti (2016). "Pulmonary Hypertension in Aortic Stenosis and Mitral Regurgitation: Rest and Exercise Echocardiography Significance". Progress in cardiovascular diseases. 59 (1): 59–70. doi:10.1016/j.pcad.2016.06.004. PMID 27389810. Unknown parameter
|month=ignored (help) - ↑ William A. Zoghbi, Maurice Enriquez-Sarano, Elyse Foster, Paul A. Grayburn, Carol D. Kraft, Robert A. Levine, Petros Nihoyannopoulos, Catherine M. Otto, Miguel A. Quinones, Harry Rakowski, William J. Stewart, Alan Waggoner & Neil J. Weissman (2003). "Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography". Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 16 (7): 777–802. doi:10.1016/S0894-7317(03)00335-3. PMID 12835667. Unknown parameter
|month=ignored (help) - ↑ J. D. Carroll, E. P. Carroll, T. Feldman, D. M. Ward, R. M. Lang, D. McGaughey & R. B. Karp (1992). "Sex-associated differences in left ventricular function in aortic stenosis of the elderly". Circulation. 86 (4): 1099–1107. PMID 1394918. Unknown parameter
|month=ignored (help) - ↑ William A. Zoghbi, Maurice Enriquez-Sarano, Elyse Foster, Paul A. Grayburn, Carol D. Kraft, Robert A. Levine, Petros Nihoyannopoulos, Catherine M. Otto, Miguel A. Quinones, Harry Rakowski, William J. Stewart, Alan Waggoner & Neil J. Weissman (2003). "Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography". Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 16 (7): 777–802. doi:10.1016/S0894-7317(03)00335-3. PMID 12835667. Unknown parameter
|month=ignored (help) - ↑ Baumgartner H, Hung J, Bermejo J, Chambers JB, Evangelista A, Griffin BP, Iung B, Otto CM, Pellikka PA, Quiñones M (2009). "Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice". Journal of the American Society of Echocardiography : Official Publication of the American Society of Echocardiography. 22 (1): 1–23, quiz 101–2. doi:10.1016/j.echo.2008.11.029. PMID 19130998. Retrieved 2012-04-13. Unknown parameter
|month=ignored (help) - ↑ Kadem L, Rieu R, Dumesnil JG, Durand LG, Pibarot P (2006). "Flow-dependent changes in Doppler-derived aortic valve effective orifice area are real and not due to artifact". Journal of the American College of Cardiology. 47 (1): 131–7. doi:10.1016/j.jacc.2005.05.100. PMID 16386676. Retrieved 2012-04-13. Unknown parameter
|month=ignored (help) - ↑ Arsenault M, Masani N, Magni G, Yao J, Deras L, Pandian N (1998). "Variation of anatomic valve area during ejection in patients with valvular aortic stenosis evaluated by two-dimensional echocardiographic planimetry: comparison with traditional Doppler data". Journal of the American College of Cardiology. 32 (7): 1931–7. PMID 9857874. Retrieved 2012-04-13. Unknown parameter
|month=ignored (help) - ↑ Lester SJ, McElhinney DB, Miller JP, Lutz JT, Otto CM, Redberg RF (2000). "Rate of change in aortic valve area during a cardiac cycle can predict the rate of hemodynamic progression of aortic stenosis". Circulation. 101 (16): 1947–52. PMID 10779461. Retrieved 2012-04-13. Unknown parameter
|month=ignored (help) - ↑ Tardif JC, Rodrigues AG, Hardy JF, Leclerc Y, Petitclerc R, Mongrain R, Mercier LA (1997). "Simultaneous determination of aortic valve area by the Gorlin formula and by transesophageal echocardiography under different transvalvular flow conditions. Evidence that anatomic aortic valve area does not change with variations in flow in aortic stenosis". Journal of the American College of Cardiology. 29 (6): 1296–302. PMID 9137227. Retrieved 2012-04-13. Unknown parameter
|month=ignored (help) - ↑ Ho PP, Pauls GL, Lamberton DF, Portnoff JS, Pai RG, Shah PM (1994). "Doppler derived aortic valve resistance in aortic stenosis: its hemodynamic validation". The Journal of Heart Valve Disease. 3 (3): 283–7. PMID 8087265. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Bermejo J, García-Fernández MA, Torrecilla EG, Bueno H, Moreno MM, San Román D, Delcán JL (1996). "Effects of dobutamine on Doppler echocardiographic indexes of aortic stenosis". Journal of the American College of Cardiology. 28 (5): 1206–13. doi:10.1016/S0735-1097(96)00287-2. PMID 8890817. Retrieved 2012-04-13. Unknown parameter
|month=ignored (help) - ↑ C. M. Otto, I. G. Burwash, M. E. Legget, B. I. Munt, M. Fujioka, N. L. Healy, C. D. Kraft, C. Y. Miyake-Hull & R. G. Schwaegler (1997). "Prospective study of asymptomatic valvular aortic stenosis. Clinical, echocardiographic, and exercise predictors of outcome". Circulation. 95 (9): 2262–2270. PMID 9142003. Unknown parameter
|month=ignored (help) - ↑ William A. Zoghbi, Maurice Enriquez-Sarano, Elyse Foster, Paul A. Grayburn, Carol D. Kraft, Robert A. Levine, Petros Nihoyannopoulos, Catherine M. Otto, Miguel A. Quinones, Harry Rakowski, William J. Stewart, Alan Waggoner & Neil J. Weissman (2003). "Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography". Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 16 (7): 777–802. doi:10.1016/S0894-7317(03)00335-3. PMID 12835667. Unknown parameter
|month=ignored (help) - ↑ Silvia Aguiar Rosa, Luisa Moura Branco, Ana Galrinho, Guilherme Portugal, Joao Abreu, Duarte Cacela, Jose Fragata & Rui Cruz Ferreira (2016). "Contribution of Dobutamine Stress Echocardiography to the Diagnosis and Prognosis of Low-Flow/Low-Gradient Aortic Stenosis". The Journal of heart valve disease. 25 (2): 130–138. PMID 27989054. Unknown parameter
|month=ignored (help) - ↑ Pibarot P, Dumesnil JG (2012). "Low-flow, low-gradient aortic stenosis with normal and depressed left ventricular ejection fraction". J Am Coll Cardiol. 60 (19): 1845–53. doi:10.1016/j.jacc.2012.06.051. PMID 23062546.
- ↑ Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP, Gentile F; et al. (2021). "2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines". Circulation. 143 (5): e72–e227. doi:10.1161/CIR.0000000000000923. PMID 33332150 Check
|pmid=value (help).