Prostatitis pathophysiology
|
Prostatitis Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Prostatitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Prostatitis pathophysiology |
|
Risk calculators and risk factors for Prostatitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Yazan Daaboul, M.D. Maliha Shakil, M.D. [2], Usama Talib, BSc, MD [3]
Overview
The pathogenesis of prostatitis is not completely understood. An infection ascending from the urethra, chemical damage caused by the reflux of urine through the ejaculatory and prostatic ducts and autoimmune involvement are a few possible theories related to the pathogenesis of various types of prostatitis.[1][2] Chronic prostatitis/chronic pelvic pain syndrome is thought to be caused by an abnormality in the hypothalamic-pituitary-adrenal axis and hormonal derangements involving the adrenocortical hormone that can stem from variable response to stress, neurogenic inflammation, and myofascial pain syndrome. On microscopic examination, neutrophils or lymphocytes can be seen inside the prostate gland, among the cells of the epithelium or inside the stromal component of the gland.[3][4]
Pathogenesis
Acute Bacterial Prostatitis
The exact pathogenesis of acute prostatitis is not fully understood. Possible pathogenesis may include:
- Ascending infection from the urethra and the chemical damage secondary to the reflux of urine through the prostatic and ejaculatory ducts.[2]
- Virulence factors are exhibited in abundance in the stains of pathogens that cause prostatitis as compared to cystitis or pyelonephritis.[5][6]
Chronic Bacterial Prostatitis
- The pathogenesis of chronic bacterial prostatitis is not very clear but an ascending infection from the distal urethra to the prostate is considered a possibility.[1]
- Greater ability to form biofilm and virulence factors may be associated with chronic bacterial prostatitis.[7]
- Seeding from the blood or lymphatics or the bowel may also cause chronic bacterial prostatitis[8]
- Anatomical abnormality in the intra-prostatic ducts may also account for their increased ability for retrograde spread of infection.[9][10]
Chronic prostatitis/chronic pelvic pain syndrome
- The symptoms of chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) are related to association between physiological factors and dysfunction in the immune, neurological and endocrine systems. Possible mechanisms include hypothalamic-pituitary-adrenal axis dysfunction and abnormalities in adrenocortical hormone, neurogenic inflammation, or myofascial pain syndrome. Abnormal functioning of the local nervous system which may be due to previous trauma, infection, or an anxious disposition and chronic albeit unconscious pelvic tensing may lead to inflammation that is mediated by nerve cells nerve cell related substances (e.g substance P). The prostate (and remaining genitourinary tract: bladder, urethra, testicles) can be inflamed by the chronic activation of pelvic nerves on the mast cells at the end of the nerve pathways.[3][4]
- Another important theory about non bacterial prostatitis includes the increased content of creatinine, urate and white blood cells due to reflux into the prostatic ducts. These agents can act as chemical agents leading to an inflammatory response.[11]
- Autoimmune phenomenon has also been proposed in some studies. Infiltration of the stroma and surroundings of the prostatic gland by lymphocytes is seen in such cases.[12][13]
Asymptomatic Prostatitis
Asymptomatic prostatitis is characterised by incidental finding of inflammation after a biopsy of prostate done for another reason. It can also be diagnosed by the presence of leukocytes on analysis of semen without the presence of symptoms of prostatic inflammation.[1]
Genetics
- Type 3 or chronic inflammatory or non inflammatory prostatitis is associated with polymorphism of IL-10 gene.[14]
- A genotype that favours decreased IL-10 production and thus a decreased anti-inflammatory effect leading to immunosupression leads to development of prostatitis.[15]
Associated Conditions
The following conditions are associated with the development of prostatitis:[1][16][17][18]
- Recurrent urinary tract infections
- Epididymitis
- Benign prostatic hyperplasia
- Urethritis
- Prostatic carcinoma
- Diabetes
- Immunocompromised status
- Urethral strictures
- Bladder neck hypertrophy
- Tuberculosis
Gross Pathology
The gross pathology in case of prostatitis may yield the following findings:[19]
Acute Prostatitis
- Peripheral zone inflammation can be demonstrated.
Chronic prostatitis
- Focal Atrophy (uniform or bilateral atrophy shows effects of hormones or age)
Microscopic Pathology
Acute Prostatitis
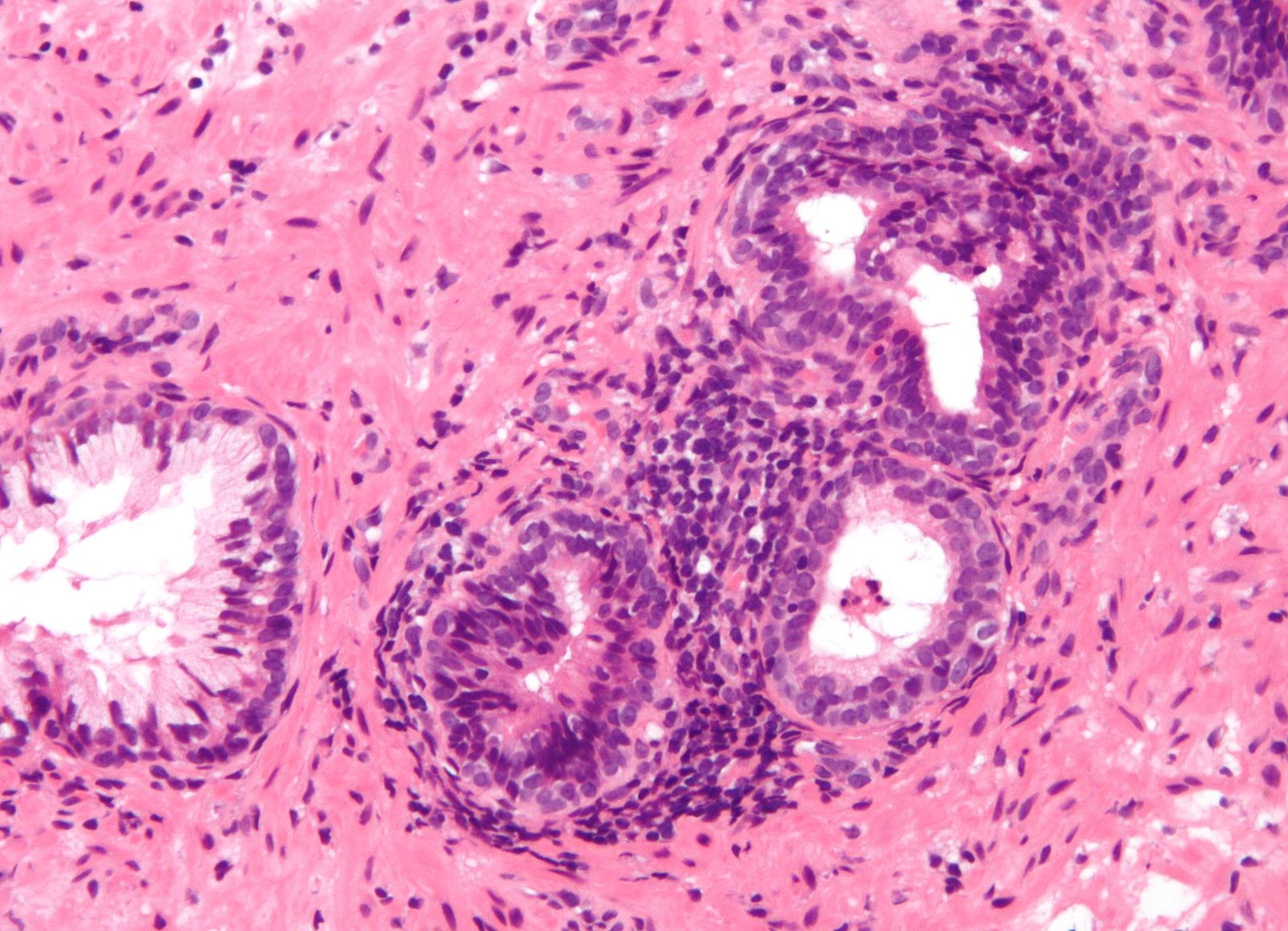
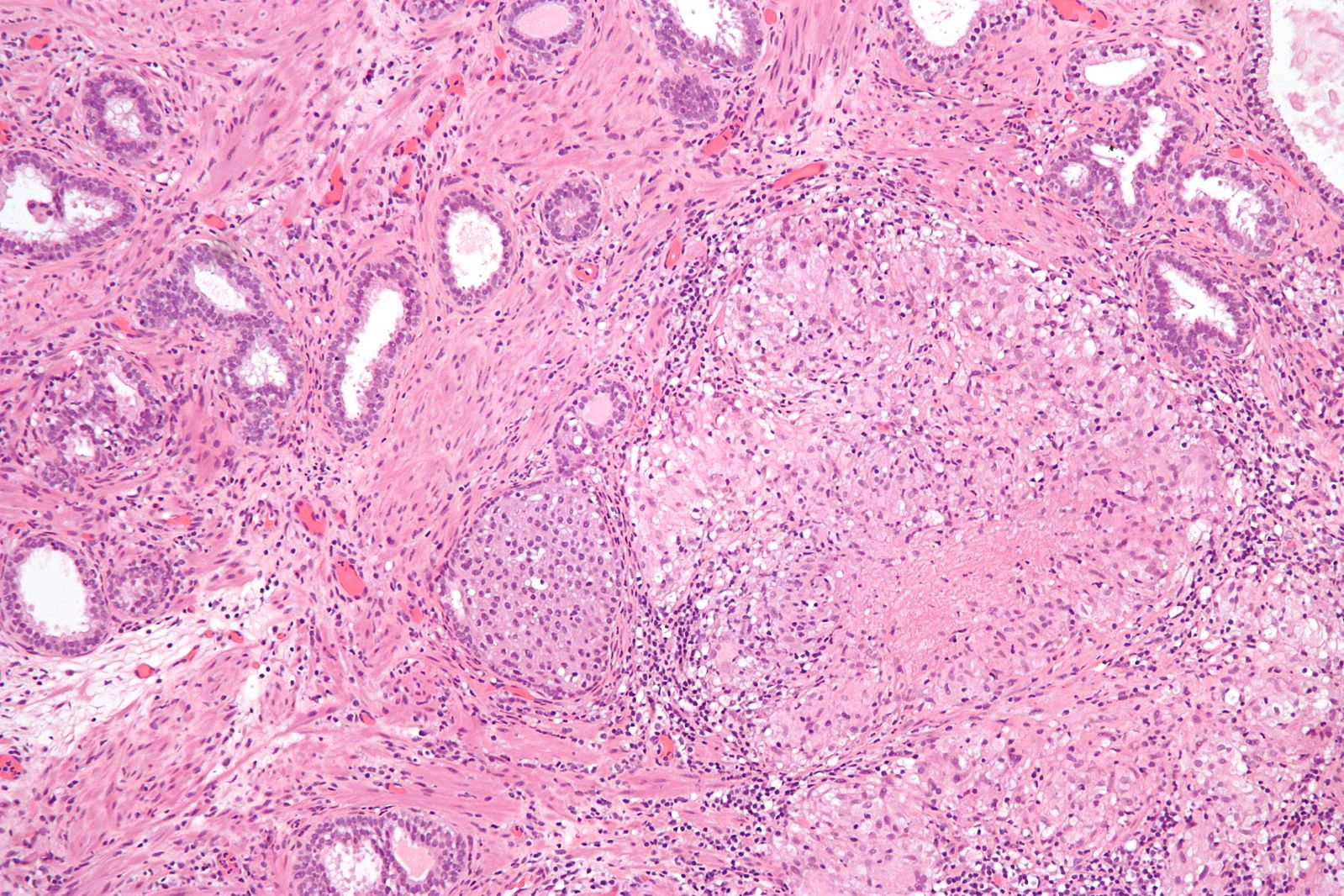
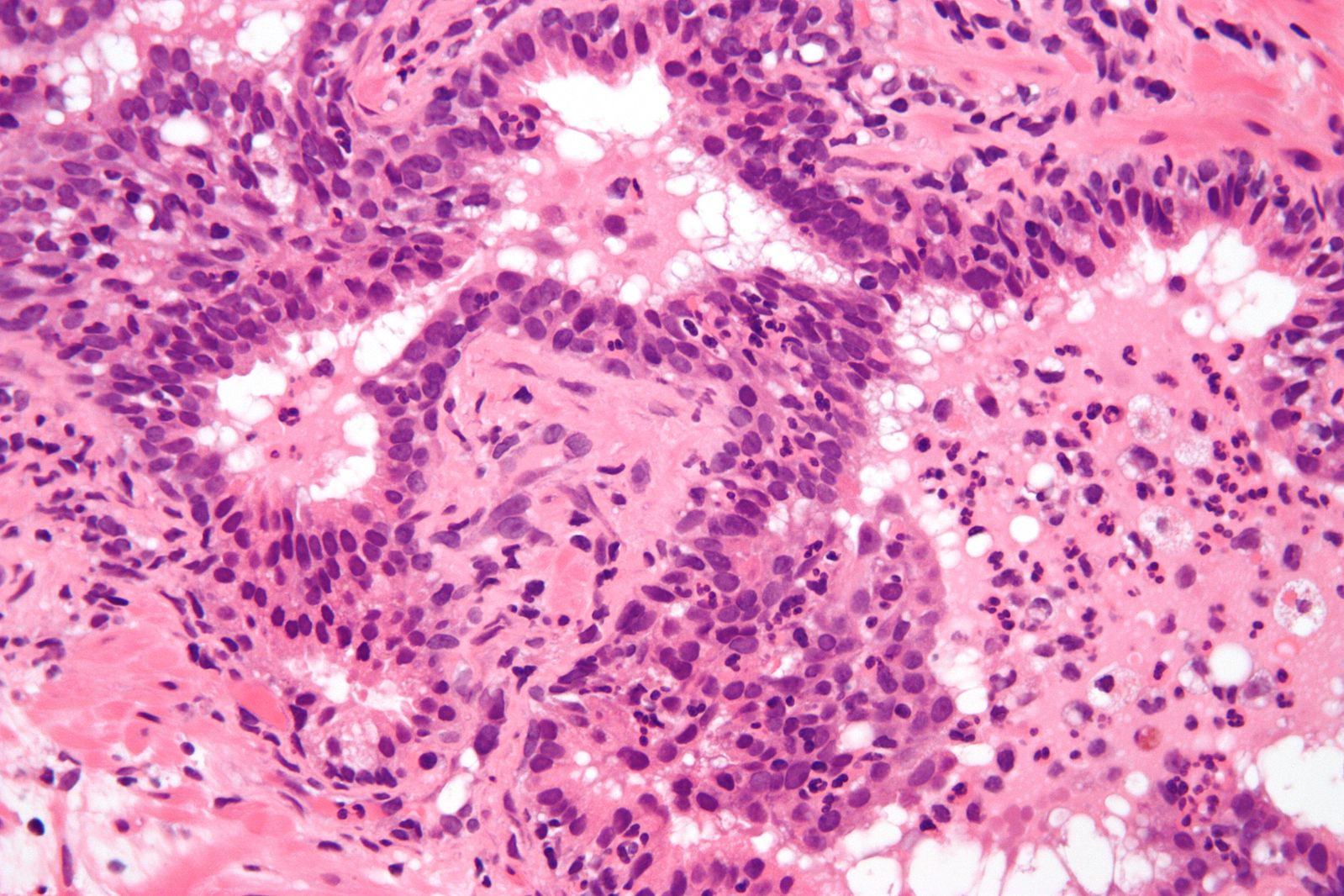
- On microscopic histopathologic exam, acute prostatitis may demonstrate glands containing neutrophils , between the epithelial cells or inside the stroma.[3][20]
Chronic Prostatitis
- On microscopic histopathologic exam, chronic prostatitis may shows glands containing lymphocytes, between the epithelial cells or inside the stroma.[4][20]
Granulomatous Prostatitis
- Granulomatous prostatitis a category of chronic prostatitis and on histopathological examination it can show areas of granulomatous changes.[20]
References
- ↑ 1.0 1.1 1.2 1.3 Sharp VJ, Takacs EB, Powell CR (2010). "Prostatitis: diagnosis and treatment". Am Fam Physician. 82 (4): 397–406. PMID 20704171.
- ↑ 2.0 2.1 Stevermer JJ, Easley SK (2000). "Treatment of prostatitis". Am Fam Physician. 61 (10): 3015–22, 3025–6. PMID 10839552.
- ↑ 3.0 3.1 3.2 Prostate Gland.Libre Pathology. http://librepathology.org/wiki/Prostate_gland#Acute_inflammation_of_the_prostate_gland. Accessed on March 2, 2016
- ↑ 4.0 4.1 4.2 Prostate Gland.Libre Pathology. http://librepathology.org/wiki/Prostate_gland#Chronic_inflammation_not_otherwise_specified. Accessed on March 2, 2016
- ↑ James R. Johnson, Michael A. Kuskowski, Abby Gajewski, Sara Soto, Juan Pablo Horcajada, M. Teresa Jimenez de Anta & Jordi Vila (2005). "Extended virulence genotypes and phylogenetic background of Escherichia coli isolates from patients with cystitis, pyelonephritis, or prostatitis". The Journal of infectious diseases. 191 (1): 46–50. doi:10.1086/426450. PMID 15593002. Unknown parameter
|month=ignored (help) - ↑ John N. Krieger, Ulrich Dobrindt, Donald E. Riley & Eric Oswald (2011). "Acute Escherichia coli prostatitis in previously health young men: bacterial virulence factors, antimicrobial resistance, and clinical outcomes". Urology. 77 (6): 1420–1425. doi:10.1016/j.urology.2010.12.059. PMID 21459419. Unknown parameter
|month=ignored (help) - ↑ Nickel, J Curtis (1999). Textbook of Prostatitis. Harvard Medical School: Isis Medical Media. ISBN 1901865045.
- ↑ A. Terai, S. Ishitoya, K. Mitsumori & O. Ogawa (2000). "Molecular epidemiological evidence for ascending urethral infection in acute bacterial prostatitis". The Journal of urology. 164 (6): 1945–1947. PMID 11061888. Unknown parameter
|month=ignored (help) - ↑ R. S. Kirby, D. Lowe, M. I. Bultitude & K. E. Shuttleworth (1982). "Intra-prostatic urinary reflux: an aetiological factor in abacterial prostatitis". British journal of urology. 54 (6): 729–731. PMID 7150931. Unknown parameter
|month=ignored (help) - ↑ N. J. Blacklock (1991). "The anatomy of the prostate: relationship with prostatic infection". Infection. 19 Suppl 3: S111–S114. PMID 2055644.
- ↑ B. E. Persson & G. Ronquist (1996). "Evidence for a mechanistic association between nonbacterial prostatitis and levels of urate and creatinine in expressed prostatic secretion". The Journal of urology. 155 (3): 958–960. PMID 8583617. Unknown parameter
|month=ignored (help) - ↑ P. J. Benson & C. S. Smith (1992). "Cytomegalovirus prostatitis". Urology. 40 (2): 165–167. PMID 1323895. Unknown parameter
|month=ignored (help) - ↑ D. W. Keetch, P. Humphrey & T. L. Ratliff (1994). "Development of a mouse model for nonbacterial prostatitis". The Journal of urology. 152 (1): 247–250. PMID 8201676. Unknown parameter
|month=ignored (help) - ↑ Feng-Hua Peng, Jin-Rui Yang, Long-Kai Peng & Xu-Biao Xie (2008). "[Association of gene polymorphisms of cytokine and cytokine receptor with type III prostatitis]". Zhonghua nan ke xue = National journal of andrology. 14 (12): 1069–1071. PMID 19157224. Unknown parameter
|month=ignored (help) - ↑ Daniel A. Shoskes, Qussay Albakri, Kim Thomas & Daniel Cook (2002). "Cytokine polymorphisms in men with chronic prostatitis/chronic pelvic pain syndrome: association with diagnosis and treatment response". The Journal of urology. 168 (1): 331–335. PMID 12050565. Unknown parameter
|month=ignored (help) - ↑ Prostatitis: Inflammation of the Prostate. NIDDK 2016. http://www.niddk.nih.gov/health-information/health-topics/urologic-disease/prostatitis-disorders-of-the-prostate/Pages/facts.aspx#sec3. Accessed on February 29, 2016
- ↑ Z. Zhang, Z. Li, Q. Yu, C. Wu, Z. Lu, F. Zhu, H. Zhang, M. Liao, T. Li, W. Chen, X. Xian, A. Tan & Z. Mo (2015). "The prevalence of and risk factors for prostatitis-like symptoms and its relation to erectile dysfunction in Chinese men". Andrology. 3 (6): 1119–1124. doi:10.1111/andr.12104. PMID 26769668. Unknown parameter
|month=ignored (help) - ↑ Upasana Joneja, William R. Short & Amity L. Roberts (2016). "Disseminated tuberculosis with prostatic abscesses in an immunocompromised patient-A case report and review of literature". IDCases. 5: 15–20. doi:10.1016/j.idcr.2016.06.002. PMID 27413691.
- ↑ last=McNeal|first=John |date= 2016 Feb 8 |title=Regional Morphology and Pathology of The Prostate |url= |journal=American Journal of Clinical Pathology|volume=49 |issue=03 |pages= |doi=https://doi.org/10.1093/ajcp/49.3.347 |pmc= |pmid=|access-date=Feb 9 2017 | name-list-format=vanc }}
- ↑ 20.0 20.1 20.2 20.3 Libre Pathology https://librepathology.org/wiki/File:Acute_inflammation_of_prostate.jpg Accessed on Feb 09, 2017