Carpal tunnel syndrome: Difference between revisions
Farman Khan (talk | contribs) |
Farman Khan (talk | contribs) |
||
| Line 178: | Line 178: | ||
|-bgcolor="LightSteelBlue" | |-bgcolor="LightSteelBlue" | ||
| '''Renal/Electrolyte''' | | '''Renal/Electrolyte''' | ||
|bgcolor="Beige"| | |bgcolor="Beige"|[[Hemodialysis]], [[Chronic kidney failure ]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |-bgcolor="LightSteelBlue" | ||
Revision as of 23:13, 24 July 2013
For patient information click here
| Carpal tunnel syndrome | |
 | |
|---|---|
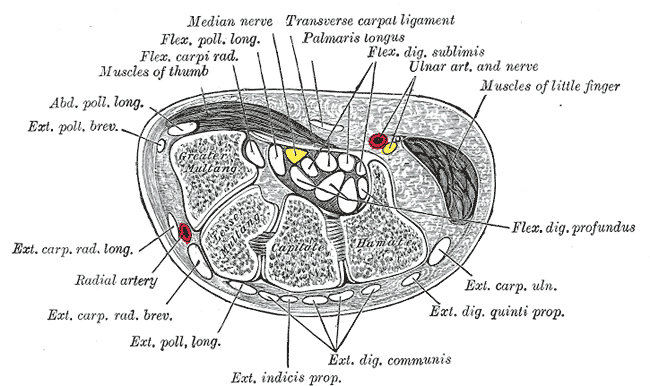
| Transverse section across the wrist and digits. (The median nerve is the yellow dot near the center. The carpal tunnel is not labeled, but the circular structure surrounding the median nerve is visible.) |
Editor(s)-In-Chief: C. Michael Gibson, M.S., M.D. [1] Phone:617-632-7753; Matthew I. Leibman, M.D.[2]; Mark R. Belsky, M.D.[3]; David E. Ruchelsman, M.D.[4];
Overview
Carpal tunnel syndrome (CTS) or Median Neuropathy at the Wrist is a medical condition in which the median nerve is compressed at the wrist, leading to pain, paresthesias, and muscle weakness in the forearm and hand.[1] A form of compressive neuropathy, CTS is more common in women than it is in men, and, though it can occur at any age, has a peak incidence around age 42.[2] The lifetime risk for CTS is around 10% of the adult population.[3].
Most cases of CTS are idiopathic, without known cause. Repetitive activities are often blamed for the development of CTS, along with several other possible causes. However, the correlation is often unclear.
It is a multi-faceted problem and can therefore be challenging to treat. Still, there is a multitude of possible treatments, e.g. treating any possible underlying disease or condition, immobilizing braces, physiotherapy, medication, prioritizing hand activities and ergonomics. Ultimately, carpal tunnel release surgery may be required. Outcomes are generally good.
The condition was first noted in the medical literature in the early 1900s.
History
Although the condition was first noted in the medical literature in the early 1900s, the first use of the term "carpal tunnel syndrome" was in 1938.[4] The pathology was identified by physician George Phalen of the Cleveland Clinic after working with a group of patients in the 1950s and 60s.[4] CTS became widely known to the general public in the 1990s as a result of the significant increase in chronic wrist pain due to the rapid expansion of office jobs.[5]
Anatomy
The median nerve passes through the carpal tunnel, a canal in the wrist that is surrounded by bone on three sides, and a fibrous sheath (the flexor retinaculum) on the fourth. Nine tendons — the flexor tendons of the hand—pass through this canal.[3] The median nerve can be compressed by a decrease in the size of the canal or an increase in the size of the contents (such as the swelling of the lubrication tissue around the flexor tendons), or both. Simply bending the wrist at 90 degrees will decrease the size of the canal.
Symptoms
Many people with carpal tunnel syndrome have gradually increasing symptoms over time. The first symptoms of CTS may appear when sleeping, and typically include numbness and paresthesia (a burning and tingling sensation) in the fingers, especially the thumb, index, and middle fingers.[3] These symptoms appear at night because many people sleep with bent wrists which further compresses the carpal tunnel. If the median nerve is already under stress, the increased compression of the bent wrist creates the numbness and tingling. Difficulty gripping and making a fist, dropping objects, and weakness are symptoms of progression. In early stages of CTS individuals often mistakenly blame the tingling and numbness on restricted blood circulation and they believe their hands are simply "falling asleep". In chronic cases, there may be wasting of the thenar muscles (the body of muscles which are connected to the thumb)
It is important to note that unless numbness or paresthesia are among the predominant symptoms, it is unlikely the symptoms are primarily caused by carpal tunnel syndrome. In effect, pain of any type, location, or severity with the absence of significant numbness or paresthesia is not likely to fall under this diagnosis.
Causes
Most cases of CTS are idiopathic, without known cause.[5] A common factor in developing carpal tunnel symptoms is increased hand use or activity. While repetitive activities are often blamed for the development of CTS, the correlation is often unclear. Physiology and family history may have a significant role in individual's susceptibility. Furthermore, stress, trauma and several other diseases are also possible causes of CTS.
The international debate regarding the relationship between CTS and repetitive motion and work is ongoing. The Occupational Safety and Health Administration (OSHA) has adopted rules and regulations regarding cumulative trauma disorders. Occupational risk factors of repetitive tasks, force, posture, and vibration have been cited. However, the American Society for Surgery of the Hand has issued a statement that the current literature does not support a causal relationship between specific work activities and the development of diseases such as CTS.
The relationship between work and CTS is controversial; in many locations workers injured at work are entitled to time off and compensation.[6] Many cases of carpal tunnel syndrome are provoked by repetitive grasping and manipulating activities, and the exposure can be cumulative. Symptoms are commonly exacerbated by forceful and repetitive use of the hand and wrists in industrial occupations.[7] Carpal tunnel syndrome results in billions of dollars of workers compensation claims every year.
Studies done by the National Institute for Occupational Safety and Health (NIOSH), indicated that job tasks involving highly repetitive manual acts or necessitating wrist bending or other stressful wrist postures were connected with incidents of CTS or related problems. However, it appears that the 30+ studies reviewed were concerned with the occupations of assembly line workers, meat packers, food processors, and the like, not general office work.
In addition, a 2005 study found that people who have discomfort at the base of the neck or in the shoulder or work with their shoulder in elevation (indicators of poor working postures) are more likely to develop a repetitive overuse injury.[8] These factors can affect the biomechanics of the upper limb or tissue tolerance to repetitive tasks resulting in injury, or both. Postural and spinal assessment along with ergonomic assessments should be included in the overall determination of the condition. Addressing these factors have been found to improve the status of work related upper limb injuries.[9]
Hypothyroidism, osteoarthritis and diabetes were most often associated with CTS-like symptoms, as were variables such as age, obesity and wrist dimension. In a 1998 study, only 35 of 297 subjects were aware of the underlying health condition which could account for their CTS-like symptoms.[10][11] Hence, these causes would be missed by doctors if they were relying on a patient's health history to rule out other causative factors. It is important that a doctor rule out other causes of CTS-like symptoms. If a patient does not have CTS, corrective surgery is destined to fail.
Studies have also related carpal tunnel and other upper extremity complaints with psychological and social factors. A large amount of psychological distress showed doubled risk of the report of pain, while job demands, poor support from colleagues, and work dissatisfaction also showed an increase in the report of pain, even after short term exposure.[12] A minority viewpoint holds that stress is the main cause, rather than a contributing factor, of a large fraction of pain symptoms usually attributed to carpal tunnel syndrome.
- Fractures of one of the arm bones, particularly a Colles' fracture.
- Dislocation of one of the carpal bones of the wrist.
- Strong blunt trauma to the wrist or lower forearm, incurred for example by using arm extremity to cushion a fall or protecting oneself from falling heavy objects.
- Hematoma forming inside the wrist, because of internal hemorrhaging.
- Deformities due to abnormal healing of old bone fractures.
Misalignment between carpal bones should be the most common cause of CTS, because by adjusting these bones' alignment, CTS dramatically decreases
Non-traumatic
Non-traumatic causes generally happen over a period of time, and are not triggered by one certain event. Many of these factors are manifestations of physiologic aging and should not be considered preventable. Examples include:
- Tenosynovitis, which is inflammation of the thin mucinous membrane around the tendons. Part of the process of inflammation is swelling, and this compresses the nerve. Swelling of this membrane is the final common pathway for most cases of carpal tunnel, whether caused idiopathically, through exposure, or medically.
- With pregnancy and hypothyroidism, fluid is retained in tissues, which swells the tenosynovium.
- Acromegaly, a disorder of growth hormones, compresses the nerve by the abnormal growth of bones around the hand and wrist.
- Tumors (usually begin), such as a ganglion or a lipoma, can protrude into the carpal tunnel, reducing the amount of space. This is exceedingly rare (less than 1%).
- Double crush syndrome, where there is compression or irritation of nerve branches contributing to the median nerve in the neck or anywhere above the wrist. This then increases the sensitivity of the nerve to compression in the wrist. This, while a possible factor, is also a rare contributor in most cases.
- Idiopathic causes are common.
- Common activities that have been identified as contributing to repetitive stress induced carpal tunnel syndrome include:
- Use of power tools
- Construction work such as handling many bricks, stone and/or lumber
Often people suffering from carpal tunnel syndrome can have multiple contributing factors which are aggravated by vigorous hand activities and repetitive stress trauma to the hand.
Proper attention to ergonomic considerations can reduce or eliminate these kinds of exposures.
While carpal tunnel syndrome is often called a "repetitive strain injury" (RSI) or "cumulative trauma disorder" (CTD), these labels are discouraged by physicians, particularly hand specialists. Carpal tunnel is a specific condition with specific symptoms that responds fairly reliably. Most of the time, carpal tunnel is not caused by a "strain" or "trauma" of any type. RSI and CTD are relatively non-specific terms with non-specific symptoms that respond variably to treatment.
Common Causes
- List the most common causes here.
Causes by Organ System
| Cardiovascular | No underlying causes |
| Chemical/Poisoning | No underlying causes |
| Dental | No underlying causes |
| Dermatologic | No underlying causes |
| Drug Side Effect | No underlying causes |
| Ear Nose Throat | No underlying causes |
| Endocrine | No underlying causes |
| Environmental | No underlying causes |
| Gastroenterologic | No underlying causes |
| Genetic | No underlying causes |
| Hematologic | No underlying causes |
| Iatrogenic | No underlying causes |
| Infectious Disease | No underlying causes |
| Musculoskeletal/Orthopedic | No underlying causes |
| Neurologic | No underlying causes |
| Nutritional/Metabolic | No underlying causes |
| Obstetric/Gynecologic | No underlying causes |
| Oncologic | No underlying causes |
| Ophthalmologic | No underlying causes |
| Overdose/Toxicity | No underlying causes |
| Psychiatric | No underlying causes |
| Pulmonary | No underlying causes |
| Renal/Electrolyte | Hemodialysis, Chronic kidney failure |
| Rheumatology/Immunology/Allergy | Wrist Arthritis, Urate crystal arthropathy, Still disease (juvenile-onset), Rheumatoid arthritis, Connective tissue diseases |
| Sexual | Female gender |
| Trauma | Wrist trauma, Repetitive strain injury wrist joint |
| Urologic | No underlying causes |
| Miscellaneous | No underlying causes |
Causes in Alphabetical Order
|
|
Diagnosis
Clinical assessment by history taking and physical examination can frequently diagnose CTS.
- Phalen's maneuver is performed by flexing the wrist gently as far as possible, then holding this position and awaiting symptoms.[13] A positive test is one that results in numbness in the median nerve distribution. The quicker the numbness starts, the more advanced the condition.
- Tinel's sign, a classic, though less specific test, is a way to detect irritated nerves. Tinel's is performed by lightly tapping (percussing) the area over the nerve to elicit a sensation of tingling or "pins and needles" in the nerve distribution.
- The carpal compression test, or applying firm pressure of the palm over the nerve to elicit symptoms has also been proposed.[14]
Other conditions may also be misdiagnosed as carpal tunnel syndrome. Thus, if, based on history and physical examination, a CTS diagnosis is suspected but not clear, patients will likely be tested electrodiagnostically with nerve conduction studies and electromyography; MRI or ultrasound imaging are also used.[15][16][17]
Complete Differential Diagnosis
- Acromegaly
- Amyloidosis
- Benign tumor
- Congestive Heart Failure
- Degenerative Arthritis
- Dermatomyositis
- Diabetes Mellitus
- Estrogens
- Fibrosis of flexor tendons
- Gout
- Hematoma
- Hypothyroidism
- Idiopathic
- Leprosy
- Mucopolysaccharidoses
- Paget's Disease
- Paraproteinemia
- Pregnancy
- Rheumatoid Arthritis
- Sarcoidosis
- Scleroderma
- Systemic Lupus Erythematosus
- Tenosynovitis of flexor tendons
- Trauma
- Tuberculosis
- Uremia
- Wrist ganglion
Prevention
The most effective way to prevent carpal tunnel syndrome is to take frequent breaks from repetitive movement such as computer keyboard usage. Free software programs such as Workrave and Xwrits are available to remind users to take breaks and stretch their wrists.
Treatment
There has been much discussion as to the most effective treatment for CTS.[18] CTS is a multi-faceted problem and can be challenging to treat from a clinician's perspective. Nevertheless, starting therapy early, when carpal tunnel is in a mild stage, is associated with improved long-term results. In summary, one has the choice of controlling the symptoms with any of the non-surgical options listed, or correcting the condition with surgery.[19] Treatments can be generally divided into six basic categories:
Reversible causes
Some causes of CTS are secondary to other conditions — metabolic disorders such as hypothyroidism, for example. Treatment of the primary disorder often resolves CTS symptoms.
Immobilizing braces

The importance of wrist braces and splints in the carpal tunnel syndrome therapy is known, but many people are unwilling to use braces. In 1993, The American Academy of Neurology recommend a non-invasive treatment for the CTS at the beginning (except for sensitive or motor deficit or grave report at EMG/ENG): a therapy using splints was indicated for light and moderate pathology.[20] Current recommendations generally don't suggest immobilizing braces, but instead activity modification and non-steroidal anti-inflammatory drugs as initial therapy, followed by more aggressive options or specialist referral if symptoms do not improve.[21] [22][23]
Many health professionals suggest that, for best results, one should wear braces at night and, if possible, during the activity primarily causing stress on the wrists.[24][25] Healing braces can sometimes exacerbate the cause of wrist pain and misalignment by continuing to prohibit proper functionality of the wrist.
Physiotherapy
Physiotherapy offers several ways to treat and control carpal tunnel syndrome. This procedure should be directed specifically towards the pattern of pain / symptoms and dysfunction assessed by the therapist. As such, it may include a range of modalities ranging from soft tissue massage, conservative stretches and exercises and techniques to directly mobilise the nerve tissue. It can also include the aforementioned immobilizing braces.
Clinically, sometimes a patient will present with a hand that is very inflamed and swollen with severe symptoms of pain, tingling and numbness and almost a fear of use due to the pain. In these cases a physiotherapist may focus on techniques to reduce the pain and inflammation, and exercises to encourage improved circulation. A comprehensive review of effectiveness of hand therapies in carpal tunnel management demonstrates that there is some valid scientific evidence for a range of therapeutic modalities.[26] For instance, Body Awareness Therapy such as the Feldenkrais method has positive effects in relation to fibromyalgia and chronic pain.[27] Structured exercise programs using these therapies to reduce wrist pain have been developed.
Localized steroid injections
Steroid injections can be quite effective for temporary relief from symptoms of CTS for a short time frame while a patient develops a longterm strategy that fits with his/her lifestyle.[28] In certain patients an injection may also be of diagnostic value. This treatment is not appropriate for extended periods, however. In general, medical professionals only prescribe to localized steroid injections until other treatment options can be identified. For most patients, permanent relief requires surgery.[29]
Prioritizing hand activities and ergonomics
Any forceful and repetitive use of the hands and wrists can cause upper extremity pain. More frequent rest can be useful if it can be orchestrated into one's schedule. It has been shown that taking multiple mini breaks during the stressful activity is more effective than taking occasional long breaks. There are computer applications that aid users in taking breaks. All of these applications have recommended defaults, following the most effective average break configuration, which is a 30 sec. pause every 3 to 5 minutes (the more severe the pain, the more often one should take this break). Before investing in these types of programs, it's best to consult with a doctor and research whether computer use is causing or contributing to the symptoms, as well as getting a formal diagnosis.
More pro-active ways to reducing the stress on the wrists which will alleviate wrist pain and strain involve adopting a more ergonomic work and life environment. Switching from a QWERTY computer keyboard layout to the Dvorak Simplified Keyboard layout was commonly cited as beneficial in early CTS studies, however meta-analyses of these studies report significant flaws in the research and question the usefulness of such keyboards.[30][31]
It is also important that one's body be aligned properly with the keyboard. This is most easily accomplished by bending ones elbows to a 90 degree angle and making sure the keyboard is at the same height as the elbows. Also it is important not to put physical stress on the wrists by hanging the wrist on the edge of a desk, or exposing the wrists to strong vibrations (e.g. manual lawn mowing). Position the computer monitor directly in front of your seat, so the neck is not twisted to either side when viewing the screen.
Exercises that relax and strengthen the muscles of the upper back can reduce the risk of a double crush of the median nerve.
Medication
Using an over-the-counter anti-inflammatory such as aspirin, ibuprofen or naproxen can be effective as well for controlling symptoms. Pain relievers like Tylenol will only mask the pain, and only an anti-inflammatory will affect inflammation. Non-steroidal inflammatory medications theoretically can treat the root swelling and thus the source of the problem. Oral steroids (prednisone) do the same, but are generally not used for this purpose due to significant side effects. The most common complications associated with long-term use of anti-inflammatory medications are gastrointestinal irritation and bleeding. Also, some anti-inflammatory medication have been linked to heart complications. Use of anti-inflammatory medication for chronic, long-term pain should be done with doctor supervision.
A more aggressive pharmaceutical option is an injection of cortisone, to reduce swelling and nerve pressure within the carpal tunnel.
Mecobalamin/Methylcobalamin has been helpful in some cases of CTS. [32]
Carpal tunnel release surgery
When visiting a hand surgeon, the first step would be examination of the hands and a review of the symptoms. If CTS is suspected, depending on the severity and the situation, the surgeon may first prescribe non-operative treatment with splinting and anti-inflammatory drugs. Nerve conduction tests will positively determine the level of compression, if any.
Indications
If symptoms resolve with non-surgical interventions, surgery can frequently be avoided. If not, then the "carpal tunnel release" surgery is recommended.[33] In general, milder cases can be controlled for months to years, but severe cases are unrelenting symptomatically and likely will come to surgical treatment.[34]
Procedure
In carpal tunnel release surgery, the goal is to divide the transverse carpal ligament in two. This is a wide ligament that runs across the hand, from the base of the thumb to the base of the fifth finger. It also forms the top of the carpal tunnel, and when the surgeon cuts across it (i.e., in a line with the middle finger) it no longer presses down on the nerves inside, relieving the pressure.[35]
There are several carpal tunnel release surgery variations: each surgeon has differences of preference based on their personal beliefs and experience. All techniques have several things in common, involving brief outpatient procedures; palm or wrist incision(s); and cutting of the transverse carpal ligament.
The two major types of surgery are open-hand surgery and endoscopic surgery. Most surgeons perform open surgery, widely considered to be the gold standard. However, many surgeons are now performing endoscopic techniques. Open surgery involves a small incision somewhere on the palm about an inch or two in length. Through this the ligament can be directly visualized and divided with relative safety. Endoscopic techniques involve one or two smaller incisions (less than half inch each) through which instrumentation is introduced including probes, knives and the scope used to visualize the operative field.
All of the surgical options typically have relatively rapid recovery profiles (days to weeks depending on the activity and technique), and all usually leave a cosmetically insignificant scar.
Efficacy
Surgery to correct carpal tunnel syndrome has a 90% or higher success rate, especially using endoscopic surgery techniques.[36][37][38] In general, endoscopic techniques are as effective as traditional open carpal surgeries,[39][40] though the faster recovery time typically noted in endoscopic procedures may be offset by higher complication rates.[41][42] Success is greatest in patients with the most typical symptoms. The most common cause of failure is incorrect diagnosis, and it should be noted that this surgery will only fix carpal tunnel syndrome, and will not relieve symptoms with alternate causes. Recurrence is rare, and apparent recurrence usually results from a misdiagnosis of another problem. Complications can occur, but serious ones are infrequent to rare.
Carpal tunnel surgery is usually performed by a hand surgeon, orthopaedic or plastic surgeon; some neurosurgeons and general surgeons also perform the procedure.
Long term recovery
Most people who find relief of their carpal tunnel symptoms with conservative or surgical management find minimal residual or "nerve damage".[43] Long-term chronic carpal tunnel syndrome (typically seen in the elderly) can result in permanent "nerve damage", i.e. symptoms of numbness, muscle wasting and weakness.
While outcomes are generally good, certain factors can contribute to poorer results that have little to do with nerves, anatomy, or surgery type. One study showed that mental status parameters, alcohol use, yield much poorer overall results of treatment.[44]
Many mild carpal tunnel syndrome sufferers either change their hand use pattern or posture at work or find a conservative, non-surgical treatment that allows them to return to full activity without hand numbness or pain, and without sleep disruption. Other people end up prioritizing their activities and possibly avoiding certain hand activities so that they can minimize pain and perform the essential tasks.
Changing jobs is also commonly done to avoid continued repetitive stress tasks. Others find success by adjusting their repetitive movements, the frequency with which they do the movements, and the amount of time they rest between periods of performing the movements.
While recurrence after surgery is a possibility, true recurrences are uncommon to rare.[45] Such recurrence can also be non-CTS hand pain. Such hand pain may have existed prior to the surgery, which is one reason it is very important to get a proper diagnosis.
In Media
In the Comedy Central prime time show South Park, season 10,episode 147, entitled Make Love, Not Warcraft, Kyle gets a severe case of carpal tunnel syndrome from playing World of Warcraft for extensive periods of time. This dilemna is quickly resolved with the application of an unknown cream.
See also
References
- ↑ Michelsen H, Posner M (2002). "Medical history of carpal tunnel syndrome". Hand Clin. 18 (2): 257–68. PMID 12371028.
- ↑ Treaster DE, Burr D (2004). "Gender differences in prevalence of upper extremity musculoskeletal disorders". Ergonomicdsvss. 47 (5): 495–526. PMID 15204301.
- ↑ 3.0 3.1 3.2 EMERG/83 at eMedicine
- ↑ 4.0 4.1 Kao SY (2003). "Carpal tunnel syndrome as an occupational disease". The Journal of the American Board of Family Practice / American Board of Family Practice. 16 (6): 533–42. PMID 14963080.
- ↑ 5.0 5.1 Sternbach G (1999). "The carpal tunnel syndrome". J Emerg Med. 17 (3): 519–23. PMID 10338251.
- ↑ Derebery J (2006). "Work-related carpal tunnel syndrome: the facts and the myths". Clin Occup Environ Med. 5 (2): 353–67, viii. PMID 16647653.
- ↑ Werner R (2006). "Evaluation of work-related carpal tunnel syndrome". J Occup Rehabil. 16 (2): 207–22. PMID 16705490.
- ↑ Werner R, Franzblau A, Gell N, Ulin S, Armstrong T (2005). "A longitudinal study of industrial and clerical workers: predictors of upper extremity tendonitis". J Occup Rehabil. 15 (1): 37–46. PMID 15794495.
- ↑ Cole D, Hogg-Johnson S, Manno M, Ibrahim S, Wells R, Ferrier S (2006). "Reducing musculoskeletal burden through ergonomic program implementation in a large newspaper". Int Arch Occup Environ Health. 80 (2): 98–108. PMID 16736193.
- ↑ Atcheson SG, Ward JR, Lowe W (1998). "Concurrent medical disease in work-related carpal tunnel syndrome". Arch Intern Med. 158 (14): 1506–12. PMID 9679791.
- ↑ Atcheson SG (1999). "Carpal tunnel syndrome: is it work-related?". Hosp Pract (Minneap). 34 (3): 49–56, quiz 147. PMID 10089926.
- ↑ Nahit ES, Pritchard CM, Cherry NM, Silman AJ, Macfarlane GJ (2001). "The influence of work related psychosocial factors and psychological distress on regional musculoskeletal pain: a study of newly employed workers". J Rheumatol. 28 (6): 1378–84. PMID 11409134.
- ↑ Cush JJ, Lipsky PE (2004). Approach to articular and musculoskeletal disorders, In: Harrison's Principles of Internal Medicine (16th ed.). McGraw-Hill Professional. pp. p. 2035. ISBN 0071402357.
- ↑ Gonzalez del Pino J, Delgado-Martinez AD, Gonzalez Gonzalez I, Lovic A (1997). "Value of the carpal compression test in the diagnosis of carpal tunnel syndrome". J Hand Surg [Br]. 22 (1): 38–41. PMID 9061521.
- ↑ Wilder-Smith E, Seet R, Lim E (2006). "Diagnosing carpal tunnel syndrome--clinical criteria and ancillary tests". Nat Clin Pract Neurol. 2 (7): 366–74. PMID 16932587.
- ↑ Bland J (2005). "Carpal tunnel syndrome". Curr Opin Neurol. 18 (5): 581–5. PMID 16155444.
- ↑ Jarvik J, Yuen E, Kliot M (2004). "Diagnosis of carpal tunnel syndrome: electrodiagnostic and MR imaging evaluation". Neuroimaging Clin N Am. 14 (1): 93–102, viii. PMID 15177259.
- ↑ Wilson JK, Sevier TL (2003). "A review of treatment for carpal tunnel syndrome". Disabil Rehabil. 25 (3): 113–9. PMID 12648000.
- ↑ Gerritsen AA, de Vet HC, Scholten RJ, Bertelsmann FW, de Krom MC, Bouter LM (2002). "Splinting vs surgery in the treatment of carpal tunnel syndrome: a randomized controlled trial". JAMA. 288 (10): 1245–51. PMID 12215131.
- ↑ American Academy of Neurology (2006). "Quality Standards Subcommittee: Practice parameter for carpal tunnel syndrome". Eura Medicophys. Neurology (43): 2406–2409. PMID 16557211.
- ↑ American Academy of Orthopaedic Surgeons (1996). "Clinical Guideline on wrist pain. National Guideline clearinghouse". Text " journal " ignored (help)
- ↑ Katz JN, Simmons BP (2002). "Carpal tunnel syndrome". NEJM. 346: 1807–1812. PMID 12050342.
- ↑ Harris JS (1998). "ed. Occupational Medicine Practice Guidelines: evaluation and management of common health problems and functional recovery in workers". Beverly Farms, Mass.: OEM Press. ISBN 978-1883595265.
- ↑ Premoselli S, Sioli P, Grossi A, Cerri C (2006). "Neutral wrist splinting in carpal tunnel syndrome: a 3- and 6-months clinical and neurophysiologic follow-up evaluation of night-only splint therapy". Eura Medicophys. PMID 16557211.
- ↑ Michlovitz SL (2004). "Conservative interventions for carpal tunnel syndrome". J Orthop Sports Phys Ther. 34 (10): 589–600. PMID 15552705.
- ↑ Muller M, Tsui D, Schnurr R, Biddulph-Deisroth L, Hard J, MacDermid J (2004). "Effectiveness of hand therapy interventions in primary management of carpal tunnel syndrome: a systematic review". J Hand Ther. 17 (2): 210–28. PMID 15162107.
- ↑ Gard G (2005). "Body awareness therapy for patients with fibromyalgia and chronic pain". Disabil Rehabil. 27 (12): 725–8. PMID 16012065.
- ↑ Marshall S, Tardif G, Ashworth N (2007). "Local corticosteroid injection for carpal tunnel syndrome". Cochrane database of systematic reviews (Online) (2): CD001554. doi:10.1002/14651858.CD001554.pub2. PMID 17443508.
- ↑ Hui AC, Wong S, Leung CH, Tong P, Mok V, Poon D, Li-Tsang CW, Wong LK, Boet R (2005). "A randomized controlled trial of surgery vs steroid injection for carpal tunnel syndrome". Neurology. 64 (12): 2074–8. PMID 15985575.
- ↑ Lincoln A, Vernick J, Ogaitis S, Smith G, Mitchell C, Agnew J (2000). "Interventions for the primary prevention of work-related carpal tunnel syndrome". Am J Prev Med. 18 (4 Suppl): 37–50. PMID 10793280.
- ↑ Verhagen A, Karels C, Bierma-Zeinstra S, Burdorf L, Feleus A, Dahaghin S, de Vet H, Koes B (2006). "Ergonomic and physiotherapeutic interventions for treating work-related complaints of the arm, neck or shoulder in adults". Cochrane Database Syst Rev. 3: CD003471. PMID 16856010.
- ↑ Sato Y, Honda Y, Iwamoto J, Kanoko T, Satoh K (2005). "Amelioration by mecobalamin of subclinical carpal tunnel syndrome involving unaffected limbs in stroke patients". J Neurol Sci. 231 (1–2): 13–8. PMID 15792815.
- ↑ Hui AC, Wong SM, Tang A, Mok V, Hung LK, Wong KS (2004). "Long-term outcome of carpal tunnel syndrome after conservative treatment". Int J Clin Pract. 58 (4): 337–9. PMID 15161116.
- ↑ Kouyoumdjian JA, Morita MP, Molina AF, Zanetta DM, Sato AK, Rocha CE, Fasanella CC (2003). "Long-term outcomes of symptomatic electrodiagnosed carpal tunnel syndrome". Arq Neuropsiquiatr. 61 (2A): 194–8. PMID 12806496.
- ↑ A patient's guide to endoscopic carpal tunnel release
- ↑ Schmelzer RE, Della Rocca GJ, Caplin DA (2006). "Endoscopic carpal tunnel release: a review of 753 cases in 486 patients". Plast Reconstr Surg. 117 (1): 177–85. PMID 16404264.
- ↑ Quaglietta P, Corriero G (2005). "Endoscopic carpal tunnel release surgery: retrospective study of 390 consecutive cases". Acta Neurochir Suppl. 92: 41–5. PMID 15830966.
- ↑ Park SH, Cho BH, Ryu KS, Cho BM, Oh SM, Park DS (2004). "Surgical outcome of endoscopic carpal tunnel release in 100 patients with carpal tunnel syndrome". Minim Invasive Neurosurg. 47 (5): 261–5. PMID 15578337.
- ↑ Scholten RJ, Gerritsen AA, Uitdehaag BM, van Geldere D, de Vet HC, Bouter LM (2004). "Surgical treatment options for carpal tunnel syndrome". Cochrane Database Syst Rev (4): CD003905. PMID 15495070.
- ↑ McNally SA, Hales PF (2003). "Results of 1245 endoscopic carpal tunnel decompressions". Hand Surg. 8 (1): 111–6. PMID 12923945.
- ↑ Thoma A, Veltri K, Haines T, Duku E (2004). "A meta-analysis of randomized controlled trials comparing endoscopic and open carpal tunnel decompression". Plast Reconstr Surg. 114 (5): 1137–46. PMID 15457025.
- ↑ Chow JC, Hantes ME (2002). "Endoscopic carpal tunnel release: thirteen years' experience with the Chow technique". J Hand Surg [Am]. 27 (6): 1011–8. PMID 12457351.
- ↑ Olsen KM, Knudson DV (2001). "Change in strength and dexterity after open carpal tunnel release". Int J Sports Med. 22 (4): 301–3. PMID 11414675.
- ↑ Katz JN, Losina E, Amick BC 3rd, Fossel AH, Bessette L, Keller RB (2001). "Predictors of outcomes of carpal tunnel release". Arthritis Rheum. 44 (5): 1184–93. PMID 11352253.
- ↑ Ruch DS, Seal CN, Bliss MS, Smith BP (2002). "Carpal tunnel release: efficacy and recurrence rate after a limited incision release". J South Orthop Assoc. 11 (3): 144–7. PMID 12539938.
External links
General information
- Carpal Tunnel Syndrome Fact Sheet from National Institute of Neurological Disorders and Stroke
- Musculoskeletal Disorders from European Agency for Safety and Health at Work (EU-OSHA)
- Carpal Tunnel Syndrome Guide from the Mayo Clinic
- American Academy of Orthopaedic Surgeons: Patient Education on Carpal Tunnel Syndrome
- ICPA Carpal Tunnel Syndrome (Summary of double crush syndrome, with additional references.)
- Carpal Tunnel Syndrome Facts and Treatment Options from the Miami Hand Center
Patient education
Template:PNS diseases of the nervous system
ca:Síndrome del túnel carpià cs:Syndrom karpálního tunelu de:Karpaltunnelsyndrom it:Sindrome del tunnel carpale nl:Carpale-tunnelsyndroom fi:Rannekanavaoireyhtymä sv:Karpaltunnelsyndrom th:คาร์พัลทันเนลซินโดรม