Acute renal failure: Difference between revisions
| Line 147: | Line 147: | ||
<youtube v=sfWkq6gJsmw/> | <youtube v=sfWkq6gJsmw/> | ||
===Acute Renal Failure 1=== | |||
===Acute Renal Failure 2=== | |||
===Acute Renal Failure 3=== | |||
<youtube v=8IU0ABdvCQA/> | |||
==See also== | ==See also== | ||
Revision as of 23:07, 24 January 2009
| Acute renal failure | |
 | |
|---|---|
| ICD-10 | N17 |
| ICD-9 | 584 |
| DiseasesDB | 11263 |
| MedlinePlus | 000501 |
| eMedicine | med/1595 |
| MeSH | D007675 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Acute renal failure (ARF), also known as acute kidney failure, is a rapid loss of renal function due to damage to the kidneys, resulting in retention of nitrogenous (urea and creatinine) and non-nitrogenous waste products that are normally excreted by the kidney. Depending on the severity and duration of the renal dysfunction, this accumulation is accompanied by metabolic disturbances, such as metabolic acidosis (acidification of the blood) and hyperkalaemia (elevated potassium levels), changes in body fluid balance, and effects on many other organ systems. It can be characterised by oliguria or anuria (decrease or cessation of urine production), although nonoliguric ARF may occur. It is a serious disease and treated as a medical emergency.
Complete Differential Diagnosis of Acute Renal Failure
Common Causes
Acute renal failure is usually categorised (as in the flowchart below) according to pre-renal, renal and post-renal causes.
| Acute Renal Failure | |||||||||||||||||||||||||||||||||
| Pre-renal | Renal | Post-renal | |||||||||||||||||||||||||||||||
- Pre-renal (causes in the blood supply):
- hypovolemia (decreased blood volume), usually from shock or dehydration and fluid loss or excessive diuretics use.
- hepatorenal syndrome in which renal perfusion is compromised in liver failure
- vascular problems, such as atheroembolic disease and renal vein thrombosis (which can occur as a complication of the nephrotic syndrome)
- Renal (damage to the kidney itself):
- infection usually sepsis (systemic inflammation due to infection),rarely of the kidney itself, termed pyelonephritis
- toxins or medication (e.g. some NSAIDs, aminoglycoside antibiotics, iodinated contrast, lithium)
- rhabdomyolysis (breakdown of muscle tissue) - the resultant release of myoglobin in the blood affects the kidney; it can be caused by injury (especially crush injury and extensive blunt trauma), statins, stimulants and some other drugs
- hemolysis (breakdown of red blood cells) - the hemoglobin damages the tubules; it may be caused by various conditions such as sickle-cell disease, and lupus erythematosus
- multiple myeloma, either due to hypercalcemia or "cast nephropathy" (multiple myeloma can also cause chronic renal failure by a different mechanism)
- acute glomerulonephritis which may be due to a variety of causes, such as anti glomerular basement membrane disease/Goodpasture's syndrome, Wegener's granulomatosis or acute lupus nephritis with systemic lupus erythematosus
- Post-renal (obstructive causes in the urinary tract) due to:
- medication interfering with normal bladder emptying.
- benign prostatic hypertrophy or prostate cancer.
- kidney stones.
- due to abdominal malignancy (e.g. ovarian cancer, colorectal cancer).
- obstructed urinary catheter.
Prerenal Causes
- Acute pancreatitis
- Aortic aneurysm
- Cirrhosis
- Dehydration
- Drugs such as diuretics
- Gastrointestinal bleeding
- Hemolysis
- Hepatorenal syndrome
- Hypovolemia
- Metrorrhagia
- Nephrotic syndrome
- Peritonitis
- Pre-eclampsia
- Rhabdomyolysis
- Renal artery stenosis
- Renal vein thrombosis
- Severe sodium and chloride loss
- Shock of various orgins
- Surgery
- Therapy with ACE inhibitors
- Trauma
- Water / electrolyte loss
Renal Causes
- Arteriosclerosis of the renal arteries
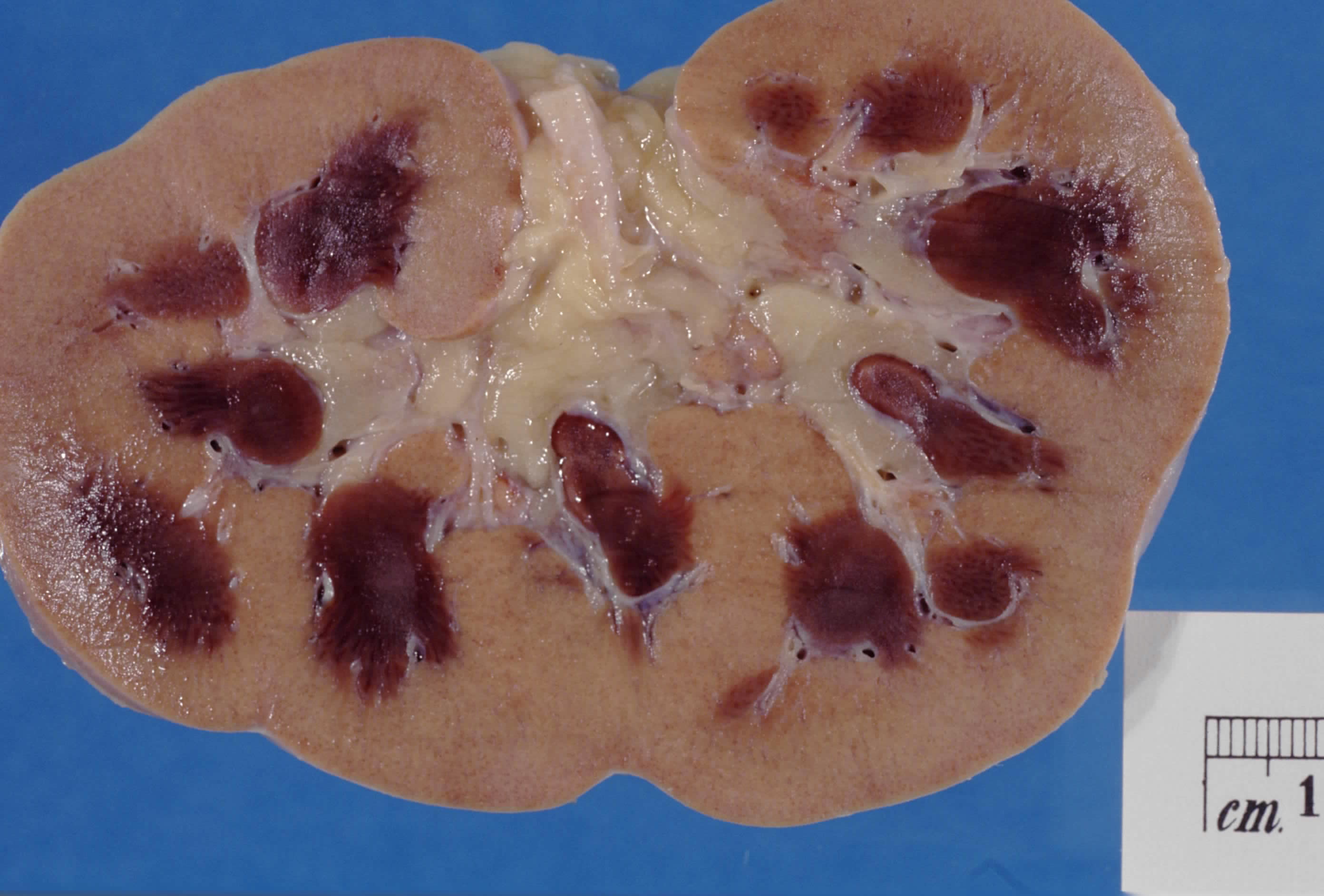
- Bilateral renal cortical necrosis
- Glomerulonephritis
- Hemolytic-Uremic Syndrome
- Kidney transplant rejection
- Interstitial nephritis
- Malignant hypertension
- Occlusion of the renal arteries
- Polyarteritis nodosa PAN
- Pyelonephritis
- Scleroderma
- Thrombotic thrombocytopenic purpura
- Tubulointerstitial renal failure
- Vasculitis
Postrenal Causes
- Bladder stone
- Bladder carcinoma
- Bladder infection
- Bladder neuropathy
- Colorectal cancer
- Multiple sclerosis
- Neurosyphillis
- Ovarian cancer
- Phimosis
- Prostatic hypertrophy
- Prostatitis
- Ruptured ureter
- Spinal cord stenosis
- Syringomyelia
- Tabes dorsalis
- Trabeculated bladder
- Urethral atresia
- Urethral trauma
- Urethral stricture
Diagnosis
Renal failure is generally diagnosed either when creatinine or blood urea nitrogen tests are markedly elevated in an ill patient, especially when oliguria is present. Previous measurements of renal function may offer comparison, which is especially important if a patient is known to have chronic renal failure as well. If the cause is not apparent, a large amount of blood tests and examination of a urine specimen is typically performed to elucidate the cause of acute renal failure, medical ultrasonography of the renal tract is essential to rule out obstruction of the urinary tract.
Consensus criteria[1][2] for the diagnosis of ARF are:
- Risk: serum creatinine increased 1.5 times OR urine production of <0.5 ml/kg body weight for 6 hours
- Injury: creatinine 2.0 times OR urine production <0.5 ml/kg for 12 h
- Failure: creatinine 3.0 times OR creatinine >355 μmol/l (with a rise of >44) or urine output below 0.3 ml/kg for 24 h
- Loss: persistent ARF or more than four weeks complete loss of kidney function
Kidney biopsy may be performed in the setting of acute renal failure, to provide a definitive diagnosis and sometimes an idea of the prognosis, unless the cause is clear and appropriate screening investigations are reassuringly negative.
Treatment
Acute renal failure may be reversible if treated promptly and appropriately. Resuscitation to normotension and a normal cardiac output is key. The main interventions are monitoring fluid intake and output as closely as possible; insertion of a urinary catheter is useful for monitoring urine output as well as relieving possible bladder outlet obstruction, such as with an enlarged prostate. In the absence of fluid overload, administering intravenous fluids is typically the first step to improve renal function. Fluid administration may be monitored with the use of a central venous catheter to avoid over- or under-replacement of fluid. If the cause is obstruction of the urinary tract, relief of the obstruction (with a nephrostomy or urinary catheter) may be necessary. Metabolic acidosis and hyperkalemia, the two most serious biochemical manifestations of acute renal failure, may require medical treatment with sodium bicarbonate administration and antihyperkalemic measures, unless dialysis is required.
Should hypotension prove a persistent problem in the fluid replete patient, inotropes such as norepinephrine and/or dobutamine may be given to improve cardiac output and hence renal perfusion. While a useful pressor, there is no evidence to suggest that dopamine is of any specific benefit,[3] and at least a suggestion of possible harm. A Swan-Ganz catheter may be used, to measure pulmonary artery occlusion pressure to provide a guide to left atrial pressure (and thus left heart function) as a target for inotropic support.
The use of diuretics such as furosemide, while widespread and sometimes convenient in ameliorating fluid overload, does not reduce the risk of complications and death.[4] In practice, diuretics may simply mask things, making it more difficult to judge the adequacy of resuscitation.
Lack of improvement with fluid resuscitation, therapy-resistant hyperkalemia, metabolic acidosis, or fluid overload may necessitate artificial support in the form of dialysis or hemofiltration. Depending on the cause, a proportion of patients will never regain full renal function, thus having end stage renal failure requiring lifelong dialysis or a kidney transplant.
History
Before the advancement of modern medicine, acute renal failure might be referred to as uremic poisoning. Uremia was the term used to describe the contamination of the blood with urine. Starting around 1847 this term was used to describe reduced urine output, now known as oliguria, which was thought to be caused by the urine's mixing with the blood instead of being voided through the urethra.
Acute renal failure due to acute tubular necrosis (ATN) was recognised in the 1940s in the United Kingdom, where crush victims during the Battle of Britain developed patchy necrosis of renal tubules, leading to a sudden decrease in renal function.[5] During the Korean and Vietnam wars, the incidence of ARF decreased due to better acute management and intravenous infusion of fluids.[6]
Acute Renal Failure Videos
<youtube v=sfWkq6gJsmw/>
Acute Renal Failure 1
Acute Renal Failure 2
Acute Renal Failure 3
<youtube v=8IU0ABdvCQA/>
See also
References
- ↑ Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P; Acute Dialysis Quality Initiative workgroup. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004 Aug;8(4):R204-12. Epub 2004 May 24. PMID 15312219 Full Text. Criteria for ARF (Figure).
- ↑ Lameire N, Van Biesen W, Vanholder R. Acute renal failure. Lancet 2005;365:417-30. PMID 15680458.
- ↑ Holmes CL, Walley KR (2003). "Bad medicine: low-dose dopamine in the ICU". Chest. 123 (4): 1266–75. doi:10.1378/chest.123.4.1266. PMID 12684320.
- ↑ Uchino S, Doig GS, Bellomo R; et al. (2004). "Diuretics and mortality in acute renal failure". Crit. Care Med. 32 (8): 1669–77. doi:10.1097/01.CCM.0000132892.51063.2F. PMID 15286542.
- ↑ Bywaters EG, Beall D (1941). "Crush injuries with impairment of renal function". Br Med J (1): 427–32. PMID 9527411.
- ↑ Schrier RW, Wang W, Poole B, Mitra A (2004). "Acute renal failure: definitions, diagnosis, pathogenesis, and therapy". J. Clin. Invest. 114 (1): 5–14. doi:10.1172/JCI22353. PMC 437979. PMID 15232604.
Template:Kidney Template:Organ failure Template:Nephrology Template:SIB