Staphylococcus aureus
To review the wikidoc page on staphylococcus aureus infection page, click here.
| Staphylococcus aureus | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | ||||||||||||||||
| Scientific classification | ||||||||||||||||
| ||||||||||||||||
| Binomial name | ||||||||||||||||
| Staphylococcus aureus Rosenbach 1884 |
|
Staphylococcus aureus infection Main page |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Staphylococcus aureus (Template:PronEng, literally "Golden Cluster Seed" and also known as golden staph, is the most common cause of staph infections. It is a spherical bacterium, frequently living on the skin or in the nose of a person. Approximately 20–30% of the general population are "staph carriers".[1] Staphylococcus aureus can cause a range of illnesses from minor skin infections, such as pimples, impetigo (may also be caused by Streptococcus pyogenes), boils, cellulitis folliculitis, furuncles, carbuncles, scalded skin syndrome and abscesses, to life-threatening diseases, such as pneumonia, meningitis, osteomyelitis endocarditis, Toxic shock syndrome (TSS), and septicemia. Its incidence is from skin, soft tissue, respiratory, bone, joint, endovascular to wound infections. It is still one of the four most common causes of nosocomial infections, often causing postsurgical wound infections. Abbreviated to S. aureus or Staph aureus in medical literature, S. aureus should not be confused with the similarly named (and also medically relevant) species of the genus Streptococcus.
S. aureus was discovered in Aberdeen, Scotland in 1880 by the surgeon Sir Alexander Ogston in pus from surgical abscesses.[2] Each year some 500,000 patients in American hospitals contract a staphylococcal infection.[3]
Microbiology
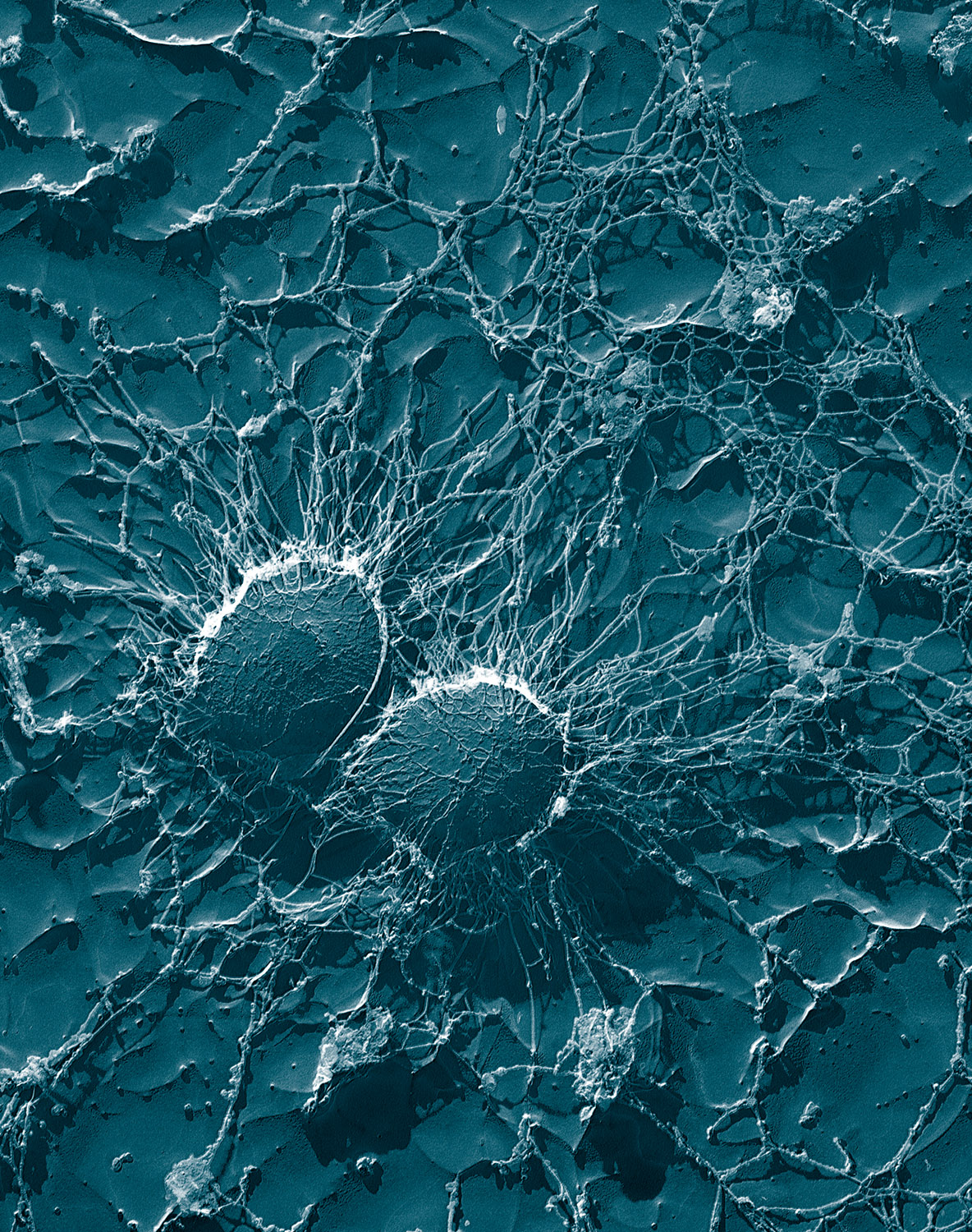
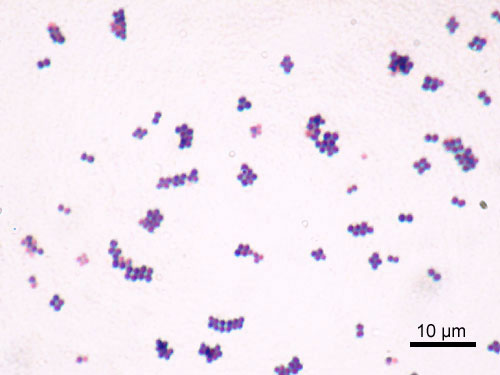
S. aureus is a Gram-positive coccus, which appears as grape-like clusters when viewed through a microscope and has large, round, golden-yellow colonies, often with hemolysis, when grown on blood agar plates.[4] The golden appearance is the etymological root of the bacteria's name: aureus means "golden" in Latin.
S. aureus is a facultative anaerobe and opportunistic pathogen.
S. aureus is catalase positive (meaning that it can produce the enzyme "catalase") and able to convert hydrogen peroxide (H2O2) to water and oxygen, which makes the catalase test useful to distinguish staphylococci from enterococci and streptococci. A large percentage of S. aureus can be differentiated from most other staphylococci by the coagulase test: S. aureus is primarily coagulase-positive (meaning that it can produce the enzyme "coagulase" that causes clot formation) while most other Staphylococcus species are coagulase-negative.[4] However, while the majority of S. aureus are coagulase-positive, some may be atypical in that they do not produce coagulase. Incorrect identification of an isolate can impact implementation of effective treatment and/or control measures.[5] It is medically important to identify S.aureus correctly as S.aureus is much more aggressive and likely to be antibiotic-resistant.
Role in disease
S. aureus may occur as a commensal on human skin; it also occurs in the nose frequently (in about a third of the population)[6] and throat less commonly. The occurrence of S. aureus under these circumstances does not always indicate infection and therefore does not always require treatment (indeed, treatment may be ineffective and re-colonisation may occur). It can survive on domesticated animals such as dogs, cats and horses, and can cause bumblefoot in chickens. It can survive for some hours on dry environmental surfaces, but the importance of the environment in spread of S. aureus is currently debated. It can host phages, such as the Panton-Valentine leukocidin, that increase its virulence.
S. aureus can infect other tissues when normal barriers have been breached (e.g., skin or mucosal lining). This leads to furuncles (boils) and carbuncles (a collection of furuncles). In infants S. aureus infection can cause a severe disease Staphylococcal scalded skin syndrome (SSSS).[7]
S. aureus infections can be spread through contact with pus from an infected wound, skin-to-skin contact with an infected person by producing hyaluronidase that destroy tissues, and contact with objects such as towels, sheets, clothing, or athletic equipment used by an infected person.
Deeply situated S. aureus infections can be very severe. Prosthetic joints put a person at particular risk for septic arthritis, and staphylococcal endocarditis (infection of the heart valves) and pneumonia, which may be rapidly spread.
Atopic dermatitis
S. aureus is extremely prevalent in atopic dermatitis patients, who are less resistant to it than other people. It often causes complications. The disease is most likely found in fertile active places including, the armpits, hair and scalp. Large pimples in those areas, when popped will cause the worst of the infection.
Toxic shock syndrome
Some strains of S. aureus produce toxic shock syndrome toxin, which are the causative agent for toxic shock syndrome. Some strains that produce an enterotoxin are the cause of staphylococcal food poisoning.
Mastitis in cows
S. aureus is one of the causal agents of mastitis in dairy cows. Its large capsule protects the organism from attack by the cow's immunological defenses.[8]
Virulence factors
Toxins
Depending on the strain, S. aureus is capable of secreting several toxins, which can be categorized into three groups. Many of these toxins are associated with specific diseases.
Pyrogenic toxin superantigens (PTSAgs) have superantigen activities that induce toxic shock syndrome (TSS). This group includes the toxin TSST-1, which causes TSS associated with tampon use. The staphylococcal enterotoxins, which cause a form of food poisoning, are included in this group.
Exfoliative toxins are implicated in the disease staphylococcal scalded-skin syndrome (SSSS), which occurs most commonly in infants and young children. It also may occur as epidemics in hospital nuseries. The protease activity of the exfoliative toxins causes peeling of the skin observed with SSSS.
Staphylococccal toxins that act on cell membranes include alpha-toxin, beta-toxin, delta-toxin, and several bicomponent toxins. The bicomponent toxin Panton-Valentine leukocidin (PVL) is associated with severe necrotizing pneumonia in children. The genes encoding the components of PVL are encoded on a bacteriophage found in community-associated MRSA strains.
Role of pigment in virulence
The vivid yellow pigmentation of S. aureus may be a factor in its virulence. When comparing a normal strain of S. aureus with a strain modified to lack the yellow coloration, the pigmented strain was more likely to survive dousing with an oxidizing chemical such as hydrogen peroxide than the mutant strain was.
Colonies of the two strains were also exposed to human neutrophils. The mutant colonies quickly succumbed while many of the pigmented colonies survived. Wounds on mice were swiped with the two strains. The pigmented strains created lingering abscesses. Wounds with the unpigmented strains healed quickly.
These tests suggest that the yellow pigment may be key to the ability of S. aureus to survive immune system attacks. Drugs that inhibit the bacterium's production of the carotenoids responsible for the yellow coloration may weaken it and renew its susceptibility to antibiotics.[9]
References
- ↑ Heyman, D. Control of Communicable Diseases Manual (2004) 18th Edition. Washington DC: American Public Health Assocation.
- ↑ Ogston A (1984). ""On Abscesses". Classics in Infectious Diseases". Rev Infect Dis. 6 (1): 122–28. PMID 6369479.
- ↑ Bowersox, John (1999-05-27). "Experimental Staph Vaccine Broadly Protective in Animal Studies". NIH. Retrieved 2007-07-28. Check date values in:
|date=(help) - ↑ 4.0 4.1 Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed. ed.). McGraw Hill. ISBN 0-8385-8529-9.
- ↑ Matthews KR, Roberson J, Gillespie BE, Luther DA, Oliver SP (1997). "Identification and Differentiation of Coagulase-Negative Staphylococcus aureus by Polymerase Chain Reaction". Journal of Food Protection. 60 (6): 686–8.
- ↑ Whitt, Dixie D. "14". Bacterial Pathogenesis: A Molecular Approach (2nd edition ed.). USA: ASM Press. ISBN 1-55581-171-X. Unknown parameter
|coauthors=ignored (help) - ↑ Curran JP, Al-Salihi FL (1980). "Neonatal staphylococcal scalded skin syndrome: massive outbreak due to an unusual phage type". Pediatrics. 66 (2): 285–90. PMID 6447271.
- ↑ Staphylococcus aureus. Electron Microscopy Unit, Beltsville Agricultural Research Center. U.S. Department of Agriculture. URL accessed 2006-07-22.M
- ↑ Liu GY, Essex A, Buchanan JT, Datta V, Hoffman HM, Bastian JF, Fierer J, Nizet V (2005). "Staphylococcus aureus golden pigment impairs neutrophil killing and promotes virulence through its antioxidant activity". J Exp Med. 202 (2): 209–15. PMID 16009720.