Cytotoxic T cell
|
WikiDoc Resources for Cytotoxic T cell |
|
Articles |
|---|
|
Most recent articles on Cytotoxic T cell Most cited articles on Cytotoxic T cell |
|
Media |
|
Powerpoint slides on Cytotoxic T cell |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Cytotoxic T cell at Clinical Trials.gov Trial results on Cytotoxic T cell Clinical Trials on Cytotoxic T cell at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Cytotoxic T cell NICE Guidance on Cytotoxic T cell
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Cytotoxic T cell Discussion groups on Cytotoxic T cell Patient Handouts on Cytotoxic T cell Directions to Hospitals Treating Cytotoxic T cell Risk calculators and risk factors for Cytotoxic T cell
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Cytotoxic T cell |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
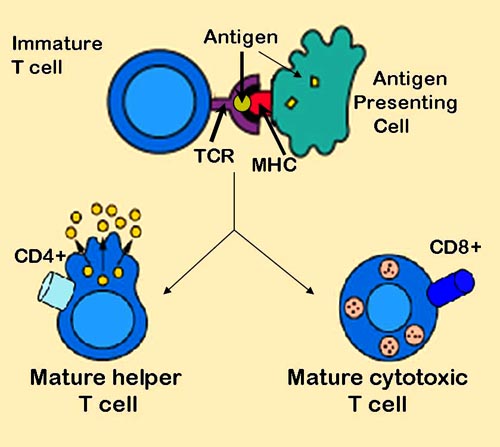
A cytotoxic T cell (also known as TC, CTL, T-Killer cell or killer T cell) belongs to a sub-group of T lymphocytes (a type of white blood cell) which are capable of inducing the death of infected somatic or tumor cells; they kill cells that are infected with viruses (or other pathogens), or are otherwise damaged or dysfunctional. Most cytotoxic T cells express T-cell receptors (TcRs) that can recognize a specific antigenic peptide bound to Class I MHC molecules, present on all nucleated cells, and a glycoprotein called CD8, which is attracted to non-variable portions of the Class I MHC molecule. The affinity between CD8 and the MHC molecule keeps the TC cell and the target cell bound closely together during antigen-specific activation. CD8+ T cells are recognized as TC cells once they become activated and are generally classified as having a pre-defined cytotoxic role within the immune system.
Cytotoxic T cell development
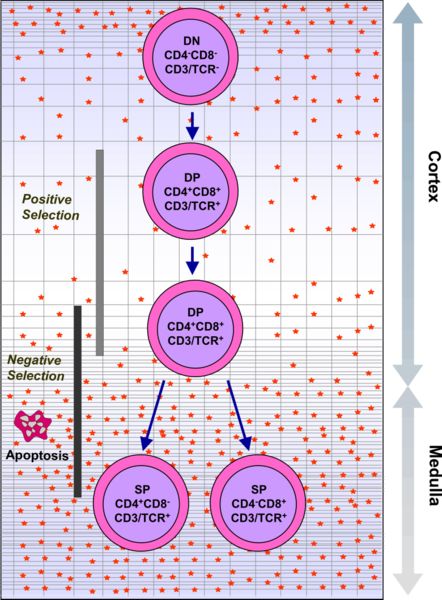
Hematopoetic stem cells in the bone marrow migrate into the thymus, where they undergo VDJ recombination of their beta-chain TcR DNA to form a developmental form of the TcR protein, known as pre-TcR. If that rearrangement is successful, the cells then rearrange their alpha-chain TcR DNA to create a functional alpha-beta TcR complex. This highly-variable genetic rearrangement product in the TcR genes helps create millions of different T cells with different TcRs, helping the body's immune system respond to virtually any protein of an invader. The vast majority of T cells express alpha-beta TcRs (αβ T cells), but some T cells in epithelial tissues (like the gut) express gamma-delta TcRs (γδ T cells), which recognize non-protein antigens.
T cells with functionally stable TcRs express both the CD4 and CD8 co-receptors and are therefore termed "double-positive" (DP) T cells (CD4+CD8+). The double-positive T cells are exposed to a wide variety of self-antigens in the thymus and undergo two selection criteria :
- (1) positive selection, in which those double-positive T cells that bind too weakly to MHC-presented self antigens undergo apoptosis because of their inability to recognize MHC-protein complexes.
- (2) negative selection, in which those double-positive T cells that bind too strongly to MHC-presented self antigens undergo apoptosis because their propensity to become autoreactive could lead to autoimmunity.
Only those T cells that bind to the MHC-self-antigen complexes weakly are positively selected. Those cells that survive positive and negative selection differentiate into single-positive T cells (either CD4+ or CD8+) dependent on whether their TcR recognizes an MHC class I presented antigen (CD8) or an MHC class II presented antigen (CD4). It is the CD8+ T-cells that will mature and go on to become cytotoxic T cells following their activation with a class I restricted antigen.
Cytotoxic T cell activation
With the exception of some cell types such as non-nucleated cells (including erythrocytes), Class I MHC is expressed by all host cells. When these cells are infected with a virus (or another intracellular pathogen), the cells degrade foreign proteins via antigen processing. These result in peptide fragments, some of which are presented by MHC Class I to the T cell antigen receptor (TcR) on CD8+ T cells.
The activation of cytotoxic T cells is dependent on several simultaneous interactions between molecules expressed on the surface of the T cell and molecules on the surface of the antigen presenting cell (APC). For instance, consider the two signal model for TC cell activation.
| Signal | T cell | APC | Description |
| first signal | TcR | peptide-bound MHC class I molecule | There is a second interaction between the CD8 coreceptor and the class I MHC molecule to stablize this signal. |
| second signal | CD28 molecule on the T cell | either CD80 or CD86 (also called B7-1 and B7-2) | CD80 and CD86 are known as costimulators for T cell activation. This second signal can be assisted (or replaced) by stimulating the TC cell with cytokines released from helper T cells. |
Once activated, the TC cell undergoes clonal expansion with the help of a cytokine called Interleukin-2 (IL-2) that is a growth and differentiation factor for T cells. This increases the number of cells specific for the target antigen that can then travel throughout the body in search of antigen-positive somatic cells.
Cytotoxic T cell effector functions
When exposed to infected/dysfunctional somatic cells, TC cells release the cytotoxins perforin and granulysin. These form pores in the target cell's plasma membrane causing ions and water to flow into the target cell that make the cell expand and eventually undergo lysis. TC also release granzyme, a serine protease, that can enter target cells via the perforin-formed pore and induce apoptosis (cell death) by activation of cellular enzymes called caspases. A second way to induce apoptosis is via cell-surface interactions between the TC and the infected cell. When a TC is activated it starts to express the surface protein FAS ligand (FasL), which can bind to Fas molecules expressed on the target cell. However, this Fas-Fas ligand interaction is thought to be more important to the disposal of unwanted T lymphocytes during their development or to the lytic activity of certain TH cells than it is to the cytolytic activity of TC effector cells.
Cytotoxic T cell role in disease pathogenesis
- Hepatitis B virus (HBV) infection
During HBV infection cytotoxic T cells play an important pathogenetic role. They contribute to nearly all of the liver injury associated with HBV infection and, by killing infected cells and by producing antiviral cytokines capable of purging HBV from viable hepatocytes, cytotoxic T cells also eliminate the virus.[1] Recently platelets have been shown to facilitate the accumulation of virus-specific cytotoxic T cells into the infected liver.[2]
References
- ↑ Iannacone M.; et al. (2006). "Pathogenetic and antiviral immune responses against hepatitis B virus". Future Virology. 1 (2): 189–196. External link in
|journal=(help) - ↑ Iannacone M.; et al. (2005). "Platelets mediate cytotoxic T lymphocyte-induced liver damage". Nat Med. 11: 1167–1169. External link in
|journal=(help)
de:Cytotoxische T-Zelle he:תא T ציטוטוקסי nl:Cytotoxische T-cel sv:Mördar-T-cell Template:WH Template:WS