VZV encephalitis
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Anthony Gallo, B.S. [2]
Synonyms and keywords: Varicella zoster virus encephalitis; Herpes zoster encephalitis; Varicella zoster encephalitis; Varicella encephalitis;
Overview
VZV encephalitis is a viral infection of the central nervous system. Based on the duration of symptoms, VZV encephalitis may be classified into either acute or chronic. The exact pathogenesis of VZV encephalitis is not fully understood. The immune system eliminates the virus from most locations upon initial infection, but it remains latent in the dorsal root ganglion and the trigeminal ganglion near the base of the skull. VZV encephalitis may be caused by either varicella (chickenpox) or herpes zoster (shingles). VZV encephalitis must be differentiated from other diseases that cause fever, headache, vomiting, and altered mental status. The incidence of VZV encephalitis is approximately 10 per 100,000 individuals affected with varicella, most often neonates and the elderly.[1] If left untreated, immunocompromised patients with VZV encephalitis may progress to mortality. Common complications include shock, hypoxemia, and meningitis. Signs of VZV encephalitis include fever, headache, ataxia, and aphasia. Laboratory findings consistent with the diagnosis of VZV encephalitis include leukocytosis and pleocytosis.[2] Magnetic resonance imaging is the imaging modality of choice for VZV encephalitis. Acyclovir is the drug of choice to treat VZV encephalitis.
Classification
Based on the duration of symptoms, VZV encephalitis may be classified into either acute or chronic.
Pathophysiology
The exact pathogenesis of VZV encephalitis is not fully understood. It is known that VZV encephalitis is the result of the varicella zoster virus, a double-stranded DNA virus within the Herpesviridae family of viruses.[2] The immune system eliminates the virus from most locations upon initial infection, but it remains latent in the dorsal root ganglion and the trigeminal ganglion near the base of the skull. Initial infection by VZV presents as chickenpox, often in children between 1-9. VZV reactivation, which presents as shingles in adults, is the result of a decline in the frequency of VZV-specific T cells.[3] The molecular basis of reactivation remains unknown.[2] Some histopathologic studies suggest of a postinfectious demyelinating process, while other findings cite direct viral cytopathology.[4][5][6]
Causes
VZV encephalitis may be caused by either varicella (chickenpox) or herpes zoster (shingles).
Differentiating VZV Encephalitis from Other Diseases
VZV encephalitis must be differentiated from other diseases that cause fever, headache, vomiting, and altered mental status, such as:[7][8][9]
| Disease | Findings |
|---|---|
| Other Viral encephalitis | Presents with acute inflammation of the brain, caused by a viral infection; it may complicate into severe brain damage as the inflamed brain pushes against the skull, potentially leading to mortality. |
| Bacterial encephalitis | Presents with acute inflammation of the brain, caused by a bacterial infection; it may complicate into severe brain damage as the inflamed brain pushes against the skull, potentially leading to mortality. |
| Encephalopathy | Presents with steady depression, generalized seizures. Generally absent are fever, headache, leukocytosis, and pleocytosis; MRI often appears normal. |
| Meningitis | Presents with headache, altered mental status, and inflammation of the meninges, which may develop in the setting of an infection, physical injury, cancer, or certain drugs; it may have an indolent evolution, resolving on its own, or may present as an rapidly evolving inflammation, causing neurologic damage and possible mortality. |
| Brain abscess | Presents with an abscess in the brain caused by the inflammation and accumulation of infected material from local or remote infectious areas of the body; the infectious agent may also be introduced as a result of head trauma or neurological procedures. |
| Acute disseminated encephalomyelitis | Presents with scattered foci of demyelination and perivenular inflammation; it can cause focal neurological signs and decreased ability to focus. |
Epidemiology and Demographics
Incidence
The incidence of VZV encephalitis is approximately 10 per 100,000 individuals affected with varicella.[1]
Age
VZV encephalitis most commonly affects infants or the elderly.[1]
Gender
Men and women are affected equally by VZV encephalitis.
Risk Factors
Common risk factors in the development of VZV encephalitis include:[10][11][8][12]
- Varicella zoster virus infection
- Immunosuppression
- HIV or AIDS
- Age extremes
- Stress
- Long-term use of corticosteroids
- Skin inflammation
- Pregnancy
- Living in tropical climate
- Working as a physician or other health care provider
- Absence of VZV immunization
Natural History, Complications, and Prognosis
Natural History
If left untreated, immunocompromised patients with VZV encephalitis may progress to mortality.
Complications
Common complications of VZV encephalitis include:[7]
- Shock
- Hypoxemia
- Hypotension
- Aphasia
- Seizures
- Meningitis
- Loss of motor skills
- Coma
- Mortality
Prognosis
Prognosis for VZV encephalitis is poor in immunocompromised individuals.
Diagnosis
History and Symptoms
If possible, a detailed and thorough history from the patient is necessary. Symptoms of VZV encephalitis include:[8]
- Fever
- Headache
- Loss of body control
- Inability to produce or comprehend language
- Seizures
- Cough
- Shortness of breath or labored breathing
- Coughing up blood
- Rash
- Lethargy
Physical Examination
Common physical examination findings of VZV encephalitis include:[8]
- Fever
- Aphasia
- Ataxia
- Nuchal rigidity
- Nystagmus
- Hypertonia or hypotonia
- Hyperreflexia or hyporeflexia
- Positive plantar reflexes
- Hemiparesis
If rash and ataxia are present simultaneously, the clinical presentation is sufficient to establish a diagnosis.
Laboratory Findings
Rapid diagnostic methods, which include polymerase chain reaction (PCR) and direct fluorescent antibody (DFA) assay, are the methods of choice. Polymerase chain reaction testing, the most sensitive test for VZV, can be used for detecting invasive disease, and detects VZV in vesicle fluid, serum, spinal fluid, and other tissues. Direct fluorescent antibody assay is performed on scrapings taken from the base of a skin lesion, and is a rapid and reliable method for diagnosing VZV disease.[13] Cerebrospinal fluid analysis is essential (unless contraindicated) in all patients with encephalitis.[12] Therefore, lumbar puncture is warranted. Laboratory findings consistent with the diagnosis of VZV encephalitis include leukocytosis and pleocytosis.[2]
CT
Computed tomography may be helpful in the diagnosis of VZV encephalitis. Findings on CT suggestive of VZV encephalitis include subtle low density within the anterior and medial temporal lobe and the insular cortex.[14] Subtleties become more apparent over time and may progress to hemorrhage, and may eventually spread to the other temporal lobe after 7-10 days.[15]
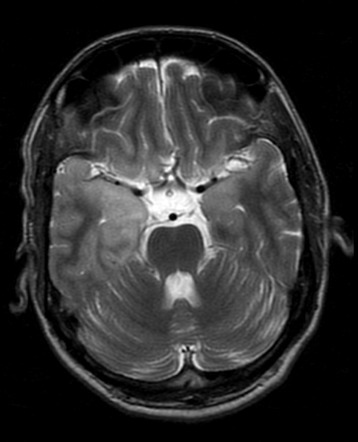
MRI
Magnetic resonance imaging is the imaging modality of choice for VZV encephalitis. Findings on MRI suggestive of VZV encephalitis include:[14][16]
- T1
- General edema in the affected region
- Hyperintense signal if complicated by subacute hemorrhage
- T1 C+ (Gd)
- Early, enhancement is generally absent
- Later, enhancement is variable and may appear as:
- Gyral enhancement
- Leptomeningeal enhancement
- Ring enhancement
- Diffuse enhancement
- T2
- Hyperintensity of affected white matter and cerebral cortex
- DWI/ADC
- GE/SWI
- May demonstrate blooming if hemorrhagic
Lumbar Puncture
Cerebrospinal fluid analysis is essential (unless contraindicated) in all patients with encephalitis.[12] Therefore, lumbar puncture may be helpful in the diagnosis of VZV encephalitis. Findings on lumbar puncture suggestive of VZV encephalitis include pleocytosis.[2]
Treatment
Medical Therapy
The mainstay of therapy for VZV encephalitis is antiviral therapy. Acyclovir is the drug of choice to treat VZV encephalitis. Ganciclovir and adjunctive coricosteriods can be considered as alternatives.[12]
Prevention
Effective measures for the primary prevention of VZV encephalitis include VZV vaccination with either varicella vaccine or zostavax.
References
- ↑ 1.0 1.1 1.2 Choo PW, Donahue JG, Manson JE, Platt R (1995). "The epidemiology of varicella and its complications". J Infect Dis. 172 (3): 706–12. PMID 7658062.
- ↑ 2.0 2.1 2.2 2.3 2.4 M.D. JE, Dolin R, Blaser MJ. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, Expert Consult Premium Edition. Saunders; 2014.
- ↑ Sadzot-Delvaux C, Kinchington PR, Debrus S, Rentier B, Arvin AM (1997). "Recognition of the latency-associated immediate early protein IE63 of varicella-zoster virus by human memory T lymphocytes". J Immunol. 159 (6): 2802–6. PMID 9300702.
- ↑ Bauman ML, Bergman I (1984). "Postvaricella encephalitis". Arch Neurol. 41 (5): 556–8. PMID 6326714.
- ↑ McCormick WF, Rodnitzky RL, Schochet SS, McKee AP (1969). "Varicella-Zoster encephalomyelitis. A morphologic and virologic study". Arch Neurol. 21 (6): 559–70. PMID 4311227.
- ↑ Takashima S, Becker LE (1979). "Neuropathology of fatal varicella". Arch Pathol Lab Med. 103 (5): 209–13. PMID 582251.
- ↑ 7.0 7.1 Kennedy PG (2004). "Viral encephalitis: causes, differential diagnosis, and management". J Neurol Neurosurg Psychiatry. 75 Suppl 1: i10–5. PMC 1765650. PMID 14978145.
- ↑ 8.0 8.1 8.2 8.3 Gnann JW (2002). "Varicella-zoster virus: atypical presentations and unusual complications". J Infect Dis. 186 Suppl 1: S91–8. doi:10.1086/342963. PMID 12353193.
- ↑ APPELBAUM E, RACHELSON MH, DOLGOPOL VB (1953). "Varicella encephalitis". Am J Med. 15 (2): 223–30. PMID 13065322.
- ↑ Mounsey AL, Matthew LG, & Slawson DC (2005). "Herpes zoster and postherpetic neuralgia: prevention and management". American Family Physician. 72 (6): 1075–1080. PMID 16190505. Retrieved 2007-06-15.
- ↑ {[cite journal|title=What does epidemiology tell us about risk factors for herpes zoster?|author=Thomas SL, Hall AJ|journal= Lancet Infect Dis.|date=2004|volume=4|issue=1|pages=26-33|pmid= 14720565}}
- ↑ 12.0 12.1 12.2 12.3 The Management of Encephalitis: Clinical Practice Guidelines by the Infectious Diseases Society of America. http://www.idsociety.org/uploadedFiles/IDSA/Guidelines-Patient_Care/PDF_Library/Encephalitis.pdf Accessed on February 16, 2016.
- ↑ Pergam SA, Limaye AP, AST Infectious Diseases Community of Practice (2009). "Varicella zoster virus (VZV) in solid organ transplant recipients". Am J Transplant. 9 Suppl 4: S108–15. doi:10.1111/j.1600-6143.2009.02901.x. PMC 2919834. PMID 20070670.
- ↑ 14.0 14.1 Herpes simplex encephalitis. Radiopaedia.org (2016). http://radiopaedia.org/articles/herpes-simplex-encephalitis Accessed on February 9, 2016.
- ↑ Whitley RJ, Gnann JW (2002). "Viral encephalitis: familiar infections and emerging pathogens". Lancet. 359 (9305): 507–13. PMID 11853816.
- ↑ Bulakbasi N, Kocaoglu M (2008). "Central nervous system infections of herpesvirus family". Neuroimaging Clin N Am. 18 (1): 53–84, viii. doi:10.1016/j.nic.2007.12.001. PMID 18319155.