Seborrheic dermatitis
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Jesus Rosario Hernandez, M.D. [2]; Aysha Anwar, M.B.B.S[3]
Synonyms and keywords: Seborrheic eczema
Overview
Seborrheic eczema (also known as Seborrheic dermatitis AmE, seborrhea) is a skin disorder affecting the scalp, face, and trunk. Seborrheic dermatitis causes flaky, itchy, red skin and temporary hair loss. It particularly affects the sebum-gland rich areas of skin. Causes of seborrheic dermatitis include Malassezia furfur (formerly known as Pityrosporum ovale), as well as genetic, environmental, hormonal, and immune-system factors. Medical therapy for seborrheic dermatitis includes antifungal agents, corticosteroids, and lithium salts.
Historical Perspective
Seborrheic dermatitis was first described by Unna in 1887. In 1894, a hypothesis was made by Unna and Sabouraud that causative agents responsible for seborrheic dermatitis include yeast Malessezia, bacteria, or both as they were obtained in high quantities in cultures obtained from the affected patients. In 1984, Shuster studied the disease and discovered seborrheic dermatitis can be treated with oral ketoconazole which was further supported by numerous studies.[1]There have been several terms used for seborrheic dermatitis such as seborrheic eczema, dermatitis seborrhoides, seborrhea oleosa (Von Hebra), steatorrhagia, seborrhagia, and flux sebacea (Rayer). Terms in the past have included morbus Unna, hyperhidrosis oleasa (Unna; increased sweat and oil), crusta lactea in infants (milk crust, cradle cap), napkin dermatitis, and eczema flannelairepityriasis sicca (dandruff, seborrhea/pityriasis capitis), pityriasis amiantacea (thick scalp involvement), and seborrhea blepharitis (seborrheic blepharitis, marginal blepharitis of the eyelids).[2]
Classification
There is no established classification system for seborrheic dermatitis.However, it may be classified according to the site involved, age group, symptoms, etiology and severity into 5 subtypes[3][4][5][6][7]
Classification by Anatomy
There is no established classification system for seborrheic dermatitis. However, seborrheic dermatitis can be classified on the basis of following factors:[8][3][9][10]
Localised
- Scalp: In infants its called Cradle Cap. Its the most common presentation in infants and appear as red yellow plaques coated by thick greasy scales, commonly appearing in first three months of age. In adults, presentation of disease is mild desquamation to honey coloured crusts which can extend to involve forehead called "corona seborrheica"
- Face: It most commonly involves eyelids, eyebrows and nasolabial folds. Eyes are involved resulting in blephritis.
- Retroauricular: lt invloves crusting, oozing and fissuring in the affected area. It may also involve external ear resulting in otitis externa.
- Body folds: It usually affects axilla, breast folds, inguinal area and genital area. May progress to fissuring and secondary infection.
- Upper Chest: It is mostly seen in adults. Affected areas may present with one of the following presentation.
- Pityriasiform: It is usually in the form oval macules and patches ranging from 5-15mm in size which tend to involve intertriginous areas.
- Petaloid type: It appears as small papules with oily scales which enlarges to become patches giving it an appearance of petals of flower, hence the name.
- Trunk: common in infants and most common site of involvement is lower abdomen.
Generalized: mostly seen in infants associated with leiner's disease and children with severe immunodeficiency. It usually is associated with diarrhea and failure to thrive and may resolve in few weeks.[11]
Classification by Age
- Infantile: seen in first three months of life. It is mostly a self limited disease in children.
- Adults: occurs most commonly between 30-60 years of age. In adults, it usually appears as chronic relapsing condition involving various parts of the body.
Classification by Symptomic Presentation
- Non pruritic: This type is most commonly seen in infants.
- Pruritic: This type is seen in older children and adults. This type is common with scalp involvement.
Classification by Etiology
Exact cause of seborrheic dermatitis is unknown. However, following causes may be related to pathogenesis of seborrheic dermatitis.
- Idiopathic : No known cause
- Infectious: Caused by fungus named Malassezia based on its response to antifungal agents.
- Autoimmune/Inflammatory: One hypothesis suggests it as a primary inflammatory dermatoses resulting in increased apoptosis, scaling and inflammation in epidermis.
Classification by Severity
- Mild to moderate disease: seen in immunocompetent individuals.
- Severe disease: Immunocomprised patients have more extensive disease which is mostly unresponsive to treatment.
Pathophysiology
Despite high prevalence of seborrheic dermatitis, there remains controversy between different pathological mechanisms causing seborrheic dermatitis. Following proposed mechanisms may play a role in pathogenesis of seborrheic dermatitis.However, patients with seborrheic dermatitis may have normal sebum production and in some individuals increased sebum production does not cause seborrheic dermatitis.[12] [13][14][15][11]
Pathogenesis
- Complete pathogenesis of seborrheic dermatitis is not fully understood. However, studies have demonstrated strong correlation between presence of fungal yeast named Malassezia and response to antifungals in patients with seborrheic dermatitis.[16]
- Malassezia is a lipophilic yeast found on the skin of both healthy individuals and seborrheic dermatitis patients. The exact mechanism of disease process in individuals having seborrheic dermatitis is not established but it is thought that host reaction to Malassezia or its metabolites causing inflammatory reaction may have a significant role in the process. Two species of Malassezia named Malassezia globosa and Malassezia restricta may have a stronger association with the development of seborrheic dermatitis.[13].
- Another proposed mechanism for seborrheic dermatitis may indicate that lipid layer of fungus Malassezia when disrupted leads to an inflammatory response resulting in increased production of pro inflammatory cytokines such as IL-6 and IL-7 and decreased production of IL-10. [7]
- Another hypothesis states that host immune response to Malassezia is not responsible for causing the disease.[17] The main cause for seborrheic dermatitis may be irritant rather than immune response, due to production of certain metabolites such as nitrates, reactive oxygen species and lipases.[14]Malasseziais seen to have lipase activity, which when act on human triglycerides causes release of unsaturated fatty acids such as arachidonic acid. These metabolites causes abnormal proliferation and differentiation of stratum corneum leading to signs and symptoms of seborrheic dermatitis.[18]
Genetics
Accordig to some studies, there is no genetic predisposition for seborrheic dermatitis.[19]. However, certain studies may show genetic causation to seborrheic dermatitis resulting from mutations in certain genes coding zinc finger proteins which is normally expressed in keratinocytes.[20]
Associated factors
Some other associated factors implicated in pathogenesis of seborrheic dermatitis include following
- Sabaceous gland activity
It is stated that sebum gland activity may correlate with seborrheic dermatitis but increased sebum production does not have a role in seborrheic dermatitis. It is supported by the fact that there is increased incidence of seborrheic dermatitis after birth in infants, teens at puberty and during third and fourth decades, all related to increased sebum gland activity at these times.[15]However, patients with seborrheic dermatitis may have normal sebum production and in some individuals increased sebum production does not cause seborrheic dermatitis.[21]
- Immune response
Seborrheic dermatitis is strongly related to immunosuppression and HIV/AIDS. Elevated levels of certain HLA antigens such as HLA-AW30, HLA-AW31, HLA-A32, HLA-B12 and HLA-B18 and increased levels of total serum IgA and IgG antibodies have been detected in SD patient implying an immune mediated pathological mechanism.[14][22][23]
- Epidermal barrier dysfunction
Abnormalities in stratum corneum such as corneocyte shape and corneodesmosomes, and disrupted lipid lamellar structure causing disruption of epidermal barrier permeability may cause alteration in intercellular lipids and desquamation process leading to increased flaking and itching.[24]
- Neurogenic and other factors
Seborrheic dermatitis in patients of parkinsonism is under neuro-endocrinological rather than pure neurological regulation supported by the fact that patients with unilateral parkinsonism present with bilateral seborrheic dermatitis. One possible explanation for this may be increase in levels of α-melanocyte stimulating hormone (α-MSH) levels. seborrheic dermatitis in these patients respond to L-dopa treatment.[23]
Gross Pathology
Superficial flaking and redness are characteristic findings of seborrheic dermatitis. Flakes usually occur in patches on scalp and tend to move about scalp over time.[25]
-
Seborrheic dermatitis showing erythema on face
-
Scalp showing redness and crusting
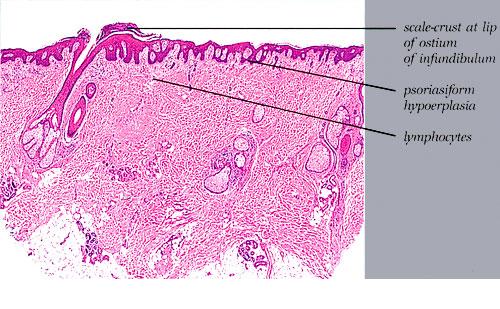
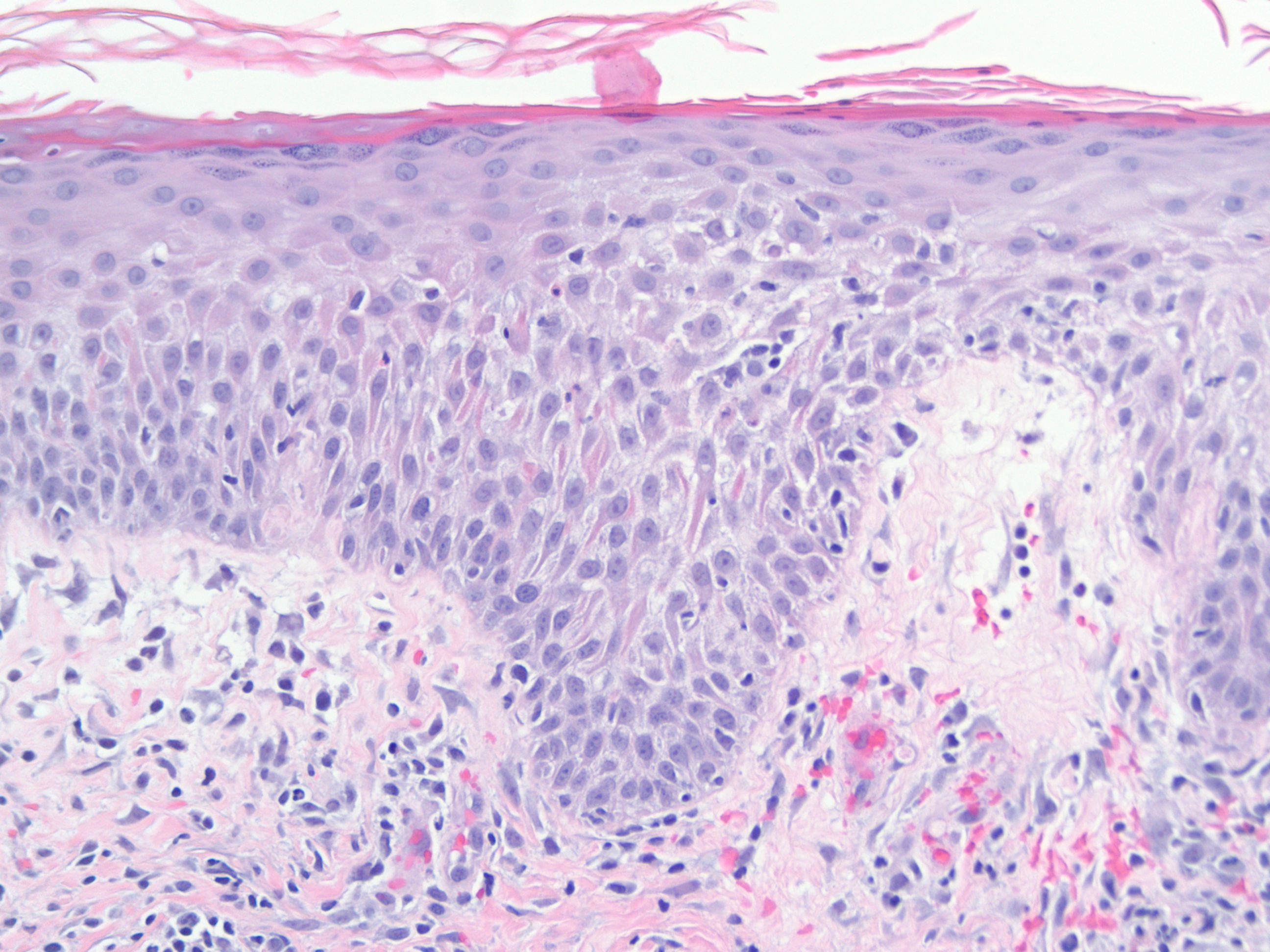
Microscopic Histopathology
Histopathological findings of seborrheic dermatitis can be divided into three types based on the following types, [22][26]
- Acute
Focal mild spongiosis with superficial crust containing neutrophils centered on a follicle, mild edema of papillary dermis, dilatatiuon of blood vessels in superficial vascular plexus with mild infiltration of lymphocytes, histiocytes and occasional neutrophils are characteristic findings of seborrheic dermatitis.
- Subacute
In addition to findings mentioned above, there is also some psoriasiform hyperplasia in subacute form of seborrheic dermatitis. This type may show presence of yeast like organisms in the surface keratin.
- Chronic
Extensive psoriasiform hyperplasia and minimal spongiosis are characteristic findings seen in this type. This type resembles psoriasis and might be difficult to differentiate from psoriasis but presence of follicular crusting favours seborrheic dermatitis.
-
Chronic Seborrheic dermatitis.
-
Acute dematitis showing papillary edema with neutrophil infiltration.
Causes
The cause of seborrhoeic dermatitis remains unknown, although many factors have been implicated.
- The widely present yeast, Malassezia furfur (formerly known as Pityrosporum ovale), is involved,[27][28] as well as genetic, environmental, hormonal, and immune-system factors.[29][30]
- A suggestion that seborrhoeic dermatitis is an inflammatory response to this yeast has yet to be proven.[31] Those afflicted with seborrhoeic dermatitis have an unfavourable epidermic response to the infection, with the skin becoming inflamed and flaking.
- In children, excessive vitamin A intake can cause seborrhoeic dermatitis.[32] Lack of biotin,[33] pyridoxine (vitamin B6)[33][34] and riboflavin (vitamin B2)[33] may also be a cause.
Differentiating Seborrheic dermatitis from Other Diseases
Differential diagnosis of seborrheic dermatitis can be classified into two types by age group[35][36][37][18][38][39][26]
Differential diagnosis in Infants
- Atopic dermatitis
- Candidiasis
- Dermatophytosis
- Diaper dermatitis
- Langerhans cell histiocytosis
- Psoriasis
- Pityriasis amiantacea
- Rosacea
- Tinea capitis
- zinc deficiency
- Vitamin B deficiency
Differential diagnosis in Adults
- Systemic lupus erythematosus
- candidiasis
- Erythrasma
- Contact dermatitis
- Psoriasis
- Tinea versicolor
- Tinea corporis
- Secondary syphilis
- Pemphigous foliaceous
- Rosacea
Epidemiology and Demographics
Epidemiology
Seborrheic dermatitis is one of the most common skin disorders in general population but prevalence estimate of the condition is difficult due to lack of diagnostic criteria and grading system for severity.[40]
Prevalence
Worldwide, the prevalence of seborrheic dermatitis is estimated to be 11000 cases per 100,000.[19] Prevalance rate varies among individuals based on the following factors:
- The prevalence rate of disease increases when mild cases are also involved.
- The prevalence of seborrheic dermatitis is higher in patients with HIV with 35000 per 100,000 in early diagnosis and 85000 per 100,000 with full blown AIDS.[41]The cause of increased prevalance in patients with seborrheic dermatitis is resistant to treatment.
- Regarding exposure to solar UV radiation, there is higher prevalence seen among those directly exposed to UV radiation which includes large percentage of mountain guides among general population.[42]
Incidence
Seborrheic dermatitis has a biphasic incidence, which involves occurence in infants between age range of 2-12 weeks and second incidence peak occuring later in life during adulthood between age groups of 40 to 60 years of life.[43]. Incidence of seborrheic dermatitis is affected by the following factors:
- The incidence of seborrheic dermatitis is higher in patients with HIV with 35000 per 100,000 in early diagnosis and 85000 per 100,000 with full blown AIDS.[41][44]
Demographics
Following demographic factors may significantly affect the incidence and prevalence of seborrheic dermatitis:
Age
Seborrheic dermatitis commonly affects three age groups.[44][45][22]
- First incidence peak is seen in infants around three to four months of age, which usually resolves in 12 months
- Second incidence peak seen around puberty.
- Third incidence peak is seen after age 50 with highest prevalence seen among age group ranging 33-44 years of age.[46]
- Age groups showing lowest prevalence of clinical disease is seen in individuals younger than 12 years.[47]
Gender
Males are more commonly affected with seborrheic dermatitis than females.[48]
Race
There may be racial predilection for seborrheic dermatitis as only few cases are seen in African Americans. If seborrheic dermatitis is seen in this population, it leads to high suspicion of HIV in affected individuals.[49]
Risk Factors
Most common risk factors for Seborrheic dermatitis are[50][18]
- Immunocompromised patients such as organ transplant recipients, patients with HIV, Hep C, chronic alcoholic pancreatitis and various malignancies such as lymphoma[51][52][53]
- Neurologic and psychiatric cases such as patients with parkinsonism, patients with depressive mood disorder, tardive dyskinesia, traumatic brain injury, epilepsy, facial nerve palsy, spinal cord injury
- Genetic disorders such as patients with downs syndrome, hailey hailey disease, cardiofaciocutaneous syndrome, mutation in (ZNF750) which codes for a zinc finger protein (C2H2) may be related to cause seborrhea like dermatitis
Other risk factors include
- Stress[54]
- Patients treated with psoralene and ultravoilet light A for psoriasis are seen to have a predisposition for seborrheic dermatitis.
- Male population is more prone to develop seborrheic dermatitis as compared to females.[55]
- Obesity, diabetes Mellitus and other endocrine disorders causing alteration in glucose metabolism.[56]
- Seasonal changes such as low temperature and decreased humditiy may have a significant role in seborrheic dermatitis flare ups[57]
- Drugs such as haloperidol deconate, lithium and chlorpromazine are associated with increased risk of disease in some patients.
Screening
There are no screening guidelines for seborrheic dermatitis.[58]
Natural History, Complications, and Prognosis
Natural History
Complications
Common complications of Seborrheic dermatitis include the following[59][44][60][61][62][11]
- Side effects to inflammation may include temporary hair loss. If severe outbreaks go untreated for long periods of time, permanent hair loss may result due to damaged hair follicles.
- Secondary bacterial infection may occur aggravating erythema, exudate and increase in local discomfort.
- Blephritis involving meibomian glands can cause abcess formation.
- Otitis Externa can result from involvement of external ear due to maceration of skin due to extcessive itching.
- Severe seborrheic dermatitis or generalised seborrheic erythroderma can occur with immunosuppression including HIV or cardiac failure.
Prognosis
- Prognosis of Seborrheic dermatitis is excellent in infants as it is a self limited disease and usually resolves in few months after birth. However, in adults it is a recurrent condition with no permanant cure. In conditions where patient is immunocompromised such as HIV or malignancy it is refractory to treatment.[63][64]
Diagnosis
There are no definitive diagnostic criteria for seborrheic dermatitis. Diagnosis of seborrheic dermatitis is primarily clinical based on history and physical examination findings.[65]
History
Obtaining complete history is important in making diagnosis of seborrheic dermatitis as it will give an insight into cause and associated risk factors for the disease. In addition to symptoms of seborrheic dermatitis presence of any of the following conditions are suggestive of below mentioned etiologies[66][67][68][18] [69][70][71]
- Parkinsons disease
- Epilepsy
- Depressive mood disorder
- Traumatic brain injury
- Spinal cord injury
- HIV
- Lymphoma
- Downs Syndrome
- Hailey Hailey Disease
- Diabetes Mellitus
Symptoms
Symtoms can be divided into following categories based on age[19][72]
Infants
Infants usually present in the first few months of life with following symptoms. Symptoms can be divided into following types depending on extent of involvement.
- Localised
- Redness and flaking are the main presenting complaints of infantile seborrheic dermatitis.
- It may involve scalp and face which are the most common sites to get involved. Other sites involved include retroauricular area, nasolabial folds, cheeks, eyebrows and eyelids.
- Pruritis is usually mild in infants having localised seborrheic dermatitis.
- Areas involving neck, axilla or body folds may present with redness without flaking giving it a glistening look.
- Napkin or diaper area involvement is not rare in infants.
- Generalised
- Few cases may present with generalised involvement such as lower abdomen, groin and pubic area. Generalised and more severe forms may raise the suspicion for underlying immunosupressive condition.
- Seborrheic dermatitis self resolves in few months and rarely presents after 12 months. In cases where it is suspected after 12 months should raise the suspicion for an alternative diagnosis.
Adults
Symptoms of seborrheic dermatitis may overlap with other skin conditions such as psoriasis, candidiasis, contact dermatitis, atopic dermatitis but most common symptoms of seborrheic dermatitis are divided into two types based on extent of involvement.[19]
- Localised
- It involves macules, thin plaques, or red patches involving scalp, face, nasolabial folds, anterior hairline, eyebrows, glabella region of the forehead, melolabial folds, ears (including the external canals, anterior auricular region, retroauricular region), central chest (sternum area), and genital region
- Pruritis is usually present in adult form and depends on severity of disease.
- Mild disease may present with fine scales with no itching.
- More severe disease presents with visible signs of inflammation such as redness and yellow to white crusting or scaling.
- Involvement of eyes is common causing redness, itching and yellow crusting of eye lashes (Blephritis).
- In cases where ears are involved, repeated itching leads to skin trauma causing secondary bacterial infection resulting in fever and ear pain.
- Generalised
Physical Examination
General Appearance
Infants look generally healthy with good apatite and sleep.
Skin
- Thick greasy scales involving scalp, forehead and vertex.
- Involvement of face may present with scaly, salmon coloured plaques.
- Areas involving neck, axilla or body folds may present with non scaly, moist look and usually tend to appear as confluent skin lesions.
- Diaper area involovement presents as erythema and maceration of skin with edema of surrounding area. Secondary bacterial and candidal infection is common in theses cases[75]
Head
Head involvement involves fine scaling in mild cases and erythematous patches with marked crusting showing signs of inflammation in severe cases.
-
SD of scalp
-
SD of scalp
Ear
Neck
Trunk
Extremities
Genitals
Adults
Imaging Findings
Other Diagnostic Studies
Treatment
Medical Therapy
The mainstay of treatment for seborrheic dermatitis is supportive. Depending on age, it can be divided into following types:
Infantile
In infants seborrheic dermatitis(Cradle Cap) is self limited disease in most cases and resolves in few months. The mainstay of treatment is supportive and divided into two types depending on severity of disease.[76]
- Mild
- Education and reassurance of parents
- Use of simple skin measures such as application of emollients such as baby oil or mineral oil to loosen scales and frequent shampooing using non-medicated shampoos and removing scales frequently.
- Severe and persistant
Adults
There is no curative treatment for seborrheic dermatitis as it is a chronic recurring condition. The mainstay of treatment is supportive to control the acute flares of disease. Supportive treatment includes use of topical and oral glucorticoids, zinc pyrithione, selenium sulfide (1%–2.5%), imidazoles (1%–2% ketoconazole shampoo, creams, lotions, or foams), ciclopirox (cream, gel, and shampoo), salicylic acid (shampoos, creams), coal tar (creams, shampoos), or mild detergents.[79][80][81]
Depending on severity of disease, treatment can be divided into following types:
- Mild
- Treatment modality for mild cases of scalp disease is topical antifungals such as azoles, zinc pyrithione, selenium sulfide (1%–2.5%), imidazoles (1%–2% ketoconazole shampoo, creams, lotions, or foams), ciclopirox (cream, gel, and shampoo), salicylic acid (shampoos, creams), coal tar (creams, shampoos. Topical use of (low, moderate and high potency) corticosteroids requiring overnight application, Baker's P&S solution, tar shampoo, or salicylic acid (ointment or shampoo, is usually reserved for thick and severe scaling.[82]
- Other effective treatments include coconut oil compound (ointment combination of coal tar, salicylic acid and sulfur).
- Moderate to Severe
- Treatment modalities for severe seborrheic dermatitis involving scalp may include systemic use of glucocorticoids((prednisolone 0.5 mg/kg body weight/day) for 7 days.
- Seborrheic dermatitis involving face, trunk and ears may require short courses of low potency topical corticosteroids to suppress initial inflammation.[82]
- Long term use of corticosteroids is discouraged due to potential adverse effects.
- Topical use of calcineurin inhibitors(pimecrolimus and tacrolimus) have both antifungals and antinflammatory properties and can be used safely.[83]
- Topical antifungals(ketoconazole, miconazole, fluconazole, itraconazole, econazole, bifonazole, climbazole, ciclopirox, and ciclopiroxolamine) have shown favourable outcomes in controlling the acute flares of seborrheic dermatitis.[84]
- Oral antifungals and oral turbinafine are reserved for severe and refractory conditions not responding to topical treatment.[85][86]
- Aluminium acetate solution may have a role in seborrheic dermatitis externa as a maintainence therapy.
- The mainstay of treatment for seborrheic blephritis is use of warm to hot compresses followed by washing with non medicated baby shampoos and debridement of thick scales by using cotton tip.
- Severe cases respond to ophthalmic ointment soultion containing sodium sulfacetamide. Fluconazole may have a role in patients with seborrheic dermatitis.[87]
- Other treatment modalities which may have a role in severe and refractory disease include isotretinoin in low doses for 3-5 months and use phototherapy with narrowband ultraviolet B or psoralen plus ultraviolet A. Phototherapy treatment is not effective in patients with thick hair.[88][89]
- Lithium succinate or gluconate topical preparations may have a role in seborrheic dermatitis involving areas other than the scalp, probably due to their antiinflammatory properties.[90][91][92]
Following are the preffered treatment regimens for treatment of seborrheic dermatitis:[93]
- 1. Antifungal agents
- Preferred regimen (1): Ketoconazole 2% in shampoo, foam, gel, or cream
- Scalp: Twice/week for clearance THEN once/week or every other week for maintenance
- Other areas: From bid to twice/week for clearance THEN from twice/week to once every other week for maintenance
- Preferred regimen (2): Bifonazole 1% in shampoo or cream
- Scalp: 3 times/week for clearance
- Other areas: qd for clearance
- Preferred regimen (3): Ciclopirox olamine (also called ciclopirox) 1.0% or 1.5% in shampoo or cream
- Scalp: Twice to 3 times/week for clearance THEN once/week or every 2 week for maintenance
- Other areas: Twice daily for clearance THEN qd for maintenance
- 2. Corticosteroids
- Preferred regimen (1): Hydrocortisone 1% in cream areas other than scalp qd or bid
- Preferred regimen (2): Betamethasone dipropionate 0.05% in lotion scalp and other areas qd or bid
- Preferred regimen (3): Clobetasol 17- butyrate 0.05% in cream areas other than scalp qd or bid
- Preferred regimen (4): Clobetasol dipro- pionate 0.05% in shampoo
- Scalp: Twice weekly in a short- contact fashion (up to 10 min application, then washing)
- Preferred regimen (5): Desonide 0.05% lotion bid on scalp and other areas
- 3. Lithium salts
- Preferred regimen: Lithium succinate AND Zinc sulfate Oin
Plant-based treatments
The World Health Organization mentions Aloe vera gel as a yet to be scientifically proven traditional medicine treatment for Seborrhoeic dermatitis.[94]
- Arctium lappa (Burdock) oil[95]
- Chelidonium majus (Celandine)[95]
- Glycyrrhiza glabra (Licorice)[95]
- Melaleuca (Tea tree) species[95]
- Plantago (Plantain) species[95]
- Symphytum officinale (Comfrey)[95]
- Zingiber officinale (Ginger) root juice[95]tment containing 8% Lithium succinate AND 0.05% Zinc sulfate
- Preferred regimen: Lithium gluconate 8% in gel bid on areas other than scalp
Surgery
Surgical intervention is not recommended for the management of seborrrheic dermatitis.
Prevention
Related Chapter
External Links
- Seborrhoeic Dermatitis at DermNet
- Seborrheic Dermatitis: An Overview - July 1, 2006 -- American Family Physician
References
- ↑ Shuster S (1984). "The aetiology of dandruff and the mode of action of therapeutic agents". Br J Dermatol. 111 (2): 235–42. PMID 6235835.
- ↑ Low, R. Cranston, and H. W. Barber. "Discussion on the etiology of seborrhoea and seborrhoeic dermatitis." The British Medical Journal (1922): 752-757.
- ↑ 3.0 3.1 Dessinioti C, Katsambas A (2013). "Seborrheic dermatitis: etiology, risk factors, and treatments: facts and controversies". Clin Dermatol. 31 (4): 343–51. doi:10.1016/j.clindermatol.2013.01.001. PMID 23806151.
- ↑ Dessinioti, Clio, and Andreas Katsambas. "Seborrheic dermatitis: Etiology, risk factors, and treatments:: Facts and controversies." Clinics in dermatology 31.4 (2013): 343-351.
- ↑ ===Classification by Anatomical Location===Peyri, J., and M. Lleonart. "Clinical and therapeutic profile and quality of life of patients with seborrheic dermatitis." Actas Dermo-Sifiliográficas (English Edition) 98.7 (2007): 476-482.
- ↑ name="pmid6220754">Burton JL, Pye RJ (1983). "Seborrhoea is not a feature of seborrhoeic dermatitis". Br Med J (Clin Res Ed). 286 (6372): 1169–70. PMC 1547390. PMID 6220754.
- ↑ 7.0 7.1 {{cite journal| author=Thomas DS, Ingham E, Bojar RA, Holland KT| title=In vitro modulation of human keratinocyte pro- and anti-inflammatory cytokine production by the capsule of Malassezia species. | journal=FEMS Immunol Med Microbiol | year= 2008 | volume= 54 | issue= 2 | pages= 203-14 | pmid=: 18752620 | doi=10.1111/j.1574-695X.2008.00468.x | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?
- ↑ Schwartz RA, Janusz CA, Janniger CK (2006). "Seborrheic dermatitis: an overview". Am Fam Physician. 74 (1): 125–30. PMID 16848386.
- ↑ Dessinioti, Clio, and Andreas Katsambas. "Seborrheic dermatitis: Etiology, risk factors, and treatments:: Facts and controversies." Clinics in dermatology 31.4 (2013): 343-351.
- ↑ ===Classification by Anatomical Location===Peyri, J., and M. Lleonart. "Clinical and therapeutic profile and quality of life of patients with seborrheic dermatitis." Actas Dermo-Sifiliográficas (English Edition) 98.7 (2007): 476-482.
- ↑ 11.0 11.1 11.2 Hampshire J, Violaris N (1988). "Oral and oropharyngeal malignancies: the case for early detection". Practitioner. 232 (1452): 766. PMID 3255962.
- ↑ name="pmid6220754">Burton JL, Pye RJ (1983). "Seborrhoea is not a feature of seborrhoeic dermatitis". Br Med J (Clin Res Ed). 286 (6372): 1169–70. PMC 1547390. PMID 6220754.
- ↑ 13.0 13.1 {{cite journal| author=Tajima M| title=[Malassezia species in patients with seborrheic dermatitis and atopic dermatitis]. | journal=Nihon Ishinkin Gakkai Zasshi | year= 2005 | volume= 46 | issue= 3 | pages= 163-7 | pmid=16094289 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?
- ↑ 14.0 14.1 14.2 Faergemann J, Bergbrant IM, Dohsé M, Scott A, Westgate G (2001). "Seborrhoeic dermatitis and Pityrosporum (Malassezia) folliculitis: characterization of inflammatory cells and mediators in the skin by immunohistochemistry". Br J Dermatol. 144 (3): 549–56. PMID 11260013.
- ↑ 15.0 15.1 Niemann C, Horsley V (2012). "Development and homeostasis of the sebaceous gland". Semin Cell Dev Biol. 23 (8): 928–36. doi:10.1016/j.semcdb.2012.08.010. PMID 22960253.
- ↑ Soares RC, Zani MB, Arruda AC, Arruda LH, Paulino LC (2015). "Malassezia intra-specific diversity and potentially new species in the skin microbiota from Brazilian healthy subjects and seborrheic dermatitis patients". PLoS One. 10 (2): e0117921. doi:10.1371/journal.pone.0117921. PMC 4335070. PMID 25695430.
- ↑ Parry ME, Sharpe GR (1998). "Seborrhoeic dermatitis is not caused by an altered immune response to Malassezia yeast". Br J Dermatol. 139 (2): 254–63. PMID 9767239.
- ↑ 18.0 18.1 18.2 18.3 Lewak N (1974). "Letter: Mythology and SIDS". N Engl J Med. 291 (14): 740–1. doi:10.1056/NEJM197410032911423. PMID 4852869.
- ↑ 19.0 19.1 19.2 19.3 Dill FJ, Schertzer M, Sandercock J, Tischler B, Wood S (1987). "Inverted tandem duplication generates a duplication deficiency of chromosome 8p". Clin Genet. 32 (2): 109–13. PMID 2888552.
- ↑ Birnbaum RY, Zvulunov A, Hallel-Halevy D, Cagnano E, Finer G, Ofir R; et al. (2006). "Seborrhea-like dermatitis with psoriasiform elements caused by a mutation in ZNF750, encoding a putative C2H2 zinc finger protein". Nat Genet. 38 (7): 749–51. doi:10.1038/ng1813. PMID 16751772.
- ↑ Burton JL, Pye RJ (1983). "Seborrhoea is not a feature of seborrhoeic dermatitis". Br Med J (Clin Res Ed). 286 (6372): 1169–70. PMC 1547390. PMID 6220754.
- ↑ 22.0 22.1 22.2 Sampaio AL, Mameri AC, Vargas TJ, Ramos-e-Silva M, Nunes AP, Carneiro SC (2011). "Seborrheic dermatitis". An Bras Dermatol. 86 (6): 1061–71, quiz 1072-4. PMID 22281892.
- ↑ 23.0 23.1 Burton JL, Shuster S (1970). "Effect of L-dopa on seborrhoea of parkinsonism". Lancet. 2 (7662): 19–20. PMID 4193751.
- ↑ Simon M, Tazi-Ahnini R, Jonca N, Caubet C, Cork MJ, Serre G (2008). "Alterations in the desquamation-related proteolytic cleavage of corneodesmosin and other corneodesmosomal proteins in psoriatic lesional epidermis". Br J Dermatol. 159 (1): 77–85. doi:10.1111/j.1365-2133.2008.08578.x. PMID 18460028.
- ↑ Warner, Ronald R., et al. "Dandruff has an altered stratum corneum ultrastructure that is improved with zinc pyrithione shampoo." Journal of the American Academy of Dermatology 45.6 (2001): 897-903.
- ↑ 26.0 26.1 Druet P, Burtin P (1967). "[On the detection in renal cancers of an antigen not found in normal human kidney]". Eur J Cancer. 3 (3): 237–8. PMID 4318061.
- ↑ Hay R, Graham-Brown R (1997). "Dandruff and seborrheic dermatitis: causes and management". Clin Exp Dermatol. 22 (1): 3–6. doi:10.1046/j.1365-2230.1997.d01-231.x. PMID 9330043.
- ↑ Nowicki R (2006). "[Modern management of dandruff]". Pol Merkur Lekarski. 20 (115): 121–4. PMID 16617752.
- ↑ Am Fam Physician 2000;61:2703-10,2713-4
- ↑ Janniger C, Schwartz R (1995). "Seborrheic dermatitis". Am Fam Physician. 52 (1): 149–55, 159–60. PMID 7604759.
- ↑ Parry M, Sharpe G (1998). "Seborrheic dermatitis is not caused by an altered immune response to Malassezia yeast". Br J Dermatol. 139 (2): 254–63. doi:10.1046/j.1365-2133.1998.02362.x. PMID 9767239.
- ↑ "MedlinePlus Medical Encyclopedia: Hypervitaminosis A". www.nlm.nih.gov. Retrieved 2008-03-19.
- ↑ 33.0 33.1 33.2 "Seborrheic Dermatitis: An Overview - July 1, 2006 -- American Family Physician". www.aafp.org. Retrieved 2008-03-19.
- ↑ "eMedicine - Nutritional Neuropathy : Article by R Andrew Sewell". www.emedicine.com. Retrieved 2008-03-19.
- ↑ Naldi, Luigi, and Alfredo Rebora. "Seborrheic dermatitis." New England Journal of Medicine 360.4 (2009): 387-396.
- ↑ Braun-Falco O, Heilgemeir GP, Lincke-Plewig H (1979). "[Histological differential diagnosis of psoriasis vulgaris and seborrheic eczema of the scalp]". Hautarzt. 30 (9): 478–83. PMID 161301.
- ↑ Rosina P, Zamperetti MR, Giovannini A, Girolomoni G (2007). "Videocapillaroscopy in the differential diagnosis between psoriasis and seborrheic dermatitis of the scalp". Dermatology. 214 (1): 21–4. doi:10.1159/000096908. PMID 17191043.
- ↑ Schwartz, Robert A., Christopher A. Janusz, and Camila K. Janniger. "Seborrheic dermatitis: an overview." Am Fam Physician 74.1 (2006): 125-130.
- ↑ Clark GW, Pope SM, Jaboori KA (2015). "Diagnosis and treatment of seborrheic dermatitis". Am Fam Physician. 91 (3): 185–90. PMID 25822272.
- ↑ Naldi, Luigi, and Alfredo Rebora. "Seborrheic dermatitis." New England Journal of Medicine 360.4 (2009): 387-396
- ↑ 41.0 41.1 Gupta AK, Bluhm R (2004). "Seborrheic dermatitis". J Eur Acad Dermatol Venereol. 18 (1): 13–26, quiz 19-20. PMID 14678527.
- ↑ Moehrle M, Dennenmoser B, Schlagenhauff B, Thomma S, Garbe C (2000). "High prevalence of seborrhoeic dermatitis on the face and scalp in mountain guides". Dermatology. 201 (2): 146–7. doi:18458 Check
|doi=value (help). PMID 11053918. - ↑ Denton, C. P., et al. "Scleroderma (systemic sclerosis)." Fitzpatrick’s Dermatology in General Medicine. 7th ed. New York, NY: McGraw-Hill Medical Publishing Division (2008): 1553-1562
- ↑ 44.0 44.1 44.2 Okochi T, Seike H, Saeki K, Sumikawa K, Yamamoto T, Higashino K (1987). "A novel alkaline phosphatase isozyme in human adipose tissue". Clin Chim Acta. 162 (1): 19–27. PMID 3100109.
- ↑ Sachdeva M, Kaur S, Nagpal M, Dewan SP (2002). "Cutaneous lesions in new born". Indian J Dermatol Venereol Leprol. 68 (6): 334–7. PMID 17656992.
- ↑ Naldi, Luigi, and Alfredo Rebora. "Seborrheic dermatitis." New England Journal of Medicine 360.4 (2009): 387-396.
- ↑ Naldi, Luigi, and Alfredo Rebora. "Seborrheic dermatitis." New England Journal of Medicine 360.4 (2009): 387-396.
- ↑ name="pmid12956195">Gupta AK, Bluhm R, Cooper EA, Summerbell RC, Batra R (2003). "Seborrheic dermatitis". Dermatol Clin. 21 (3): 401–12. PMID 12956195.
- ↑ Mahé, Antoine, et al. "Predictive value of seborrheic dermatitis and other common dermatoses for HIV infection in Bamako, Mali." Journal of the American Academy of Dermatology 34.6 (1996):
- ↑ Hastings GB, Leathar DS, Scott AC (1988). "Scottish attitudes to AIDS". Br Med J (Clin Res Ed). 296 (6627): 991–2. PMC 2545449. PMID 3129121.
- ↑ Dunic I, Vesic S, Jevtovic DJ (2004). "Oral candidiasis and seborrheic dermatitis in HIV-infected patients on highly active antiretroviral therapy". HIV Med. 5 (1): 50–4. PMID 14731170.
- ↑ Soldatov IuN, Glushko AV (1974). "[Spontaneous rupture of the epigastric arteries simulating acute abdomen]". Klin Khir (11): 61–2. PMID 4280471.
- ↑ Özcan D, Seçkin D, Ada S, Haberal M (2013). "Mucocutaneous disorders in renal transplant recipients receiving sirolimus-based immunosuppressive therapy: a prospective, case-control study". Clin Transplant. 27 (5): 742–8. doi:10.1111/ctr.12215. PMID 23991694 : 23991694 Check
|pmid=value (help). - ↑ Misery L, Touboul S, Vinçot C, Dutray S, Rolland-Jacob G, Consoli SG; et al. (2007). "[Stress and seborrheic dermatitis]". Ann Dermatol Venereol. 134 (11): 833–7. PMID 18033062.
- ↑ Baran, Robert, and Howard Maibach, eds. Textbook of cosmetic dermatology. CRC Press, 2010.
- ↑ Dowlati, Bijan, et al. "Insulin quantification in patients with seborrheic dermatitis." Archives of dermatology 134.8 (1998): 1043-1045.
- ↑ Banerjee S, Gangopadhyay DN, Jana S, Chanda M (2010). "Seasonal variation in pediatric dermatoses". Indian J Dermatol. 55 (1): 44–6. doi:10.4103/0019-5154.60351. PMC 2856373. PMID 20418977.
- ↑ US preventive service task force.seborrheic dermatitis. http://www.uspreventiveservicestaskforce.org/accessed on August16, 2016
- ↑ Gorman CR, White SW (2005). "Rosaceiform dermatitis as a complication of treatment of facial seborrheic dermatitis with 1% pimecrolimus cream". Arch Dermatol. 141 (9): 1168. doi:10.1001/archderm.141.9.1168. PMID 16172323.
- ↑ Guin JD (2004). "Eyelid dermatitis: a report of 215 patients". Contact Dermatitis. 50 (2): 87–90. doi:10.1111/j.0105-1873.2004.00311.x. PMID 15128319.
- ↑ Ooi ET, Tidman MJ (2014). "Improving the management of seborrhoeic dermatitis". Practitioner. 258 (1768): 23–6, 3. PMID 24689165.
- ↑ Ross, Elizabeth K., Colombina Vincenzi, and Antonella Tosti. "Videodermoscopy in the evaluation of hair and scalp disorders." Journal of the American Academy of Dermatology 55.5 (2006): 799-806.
- ↑ Foley P, Zuo Y, Plunkett A, Merlin K, Marks R (2003). "The frequency of common skin conditions in preschool-aged children in Australia: seborrheic dermatitis and pityriasis capitis (cradle cap)". Arch Dermatol. 139 (3): 318–22. PMID 12622623.
- ↑ Forrestel AK, Kovarik CL, Mosam A, Gupta D, Maurer TA, Micheletti RG (2016). "Diffuse HIV-associated seborrheic dermatitis - a case series". Int J STD AIDS. doi:10.1177/0956462416641816. PMID 27013615.
- ↑ Schwartz, Robert A., Christopher A. Janusz, and Camila K. Janniger. "Seborrheic dermatitis: an overview." Am Fam Physician 74.1 (2006): 125-130
- ↑ Tsao BP, Aldo-Benson MA (1985). "Macrophage-derived soluble factors mediate suppression induced by 2,4-dinitrophenyl-conjugated mouse IgG in hybridoma cells". Cell Immunol. 91 (2): 362–74. PMID 3995588.
- ↑ Rola-Pleszczynski M (1985). "Differential effects of leukotriene B4 on T4+ and T8+ lymphocyte phenotype and immunoregulatory functions". J Immunol. 135 (2): 1357–60. PMID 2861228.
- ↑ Borda LJ, Wikramanayake TC. Seborrheic Dermatitis and Dandruff: A Comprehensive Review. Journal of clinical and investigative dermatology. 2015;3(2):10.13188/2373-1044.1000019.
- ↑ Muñoz-Pérez MA, Rodriguez-Pichardo A, Camacho F, Colmenero MA (1998). "Dermatological findings correlated with CD4 lymphocyte counts in a prospective 3 year study of 1161 patients with human immunodeficiency virus disease predominantly acquired through intravenous drug abuse". Br J Dermatol. 139 (1): 33–9. PMID 9764146.
- ↑ Bilgili SG, Akdeniz N, Karadag AS, Akbayram S, Calka O, Ozkol HU (2011). "Mucocutaneous disorders in children with down syndrome: case-controlled study". Genet Couns. 22 (4): 385–92. PMID 22303799.
- ↑ Baş Y, Seçkin HY, Kalkan G, Takci Z, Çitil R, Önder Y; et al. (2016). "Prevalence and related factors of psoriasis and seborrheic dermatitis: a community-based study". Turk J Med Sci. 46 (2): 303–9. doi:10.3906/sag-1406-51. PMID 27511489.
- ↑ Sarkar R, Garg VK (2010). "Erythroderma in children". Indian J Dermatol Venereol Leprol. 76 (4): 341–7. doi:10.4103/0378-6323.66576. PMID 20657113.
- ↑ Soeprono FF, Schinella RA, Cockerell CJ, Comite SL (1986). "Seborrheic-like dermatitis of acquired immunodeficiency syndrome. A clinicopathologic study". J Am Acad Dermatol. 14 (2 Pt 1): 242–8. PMID 2936776.
- ↑ Mathes BM, Douglass MC (1985). "Seborrheic dermatitis in patients with acquired immunodeficiency syndrome". J Am Acad Dermatol. 13 (6): 947–51. PMID 2934444.
- ↑ Tüzün Y, Wolf R, Bağlam S, Engin B (2015). "Diaper (napkin) dermatitis: A fold (intertriginous) dermatosis". Clin Dermatol. 33 (4): 477–82. doi:10.1016/j.clindermatol.2015.04.012. PMID 26051065.
- ↑ Foley, Peter, et al. "The frequency of common skin conditions in preschool-age children in Australia: atopic dermatitis." Archives of dermatology 137.3 (2001): 293-300.
- ↑ Yasuda G, Sun L, Umemura S, Pettinger WA, Jeffries WB (1991). "Characterization of prazosin-sensitive alpha 2 B-adrenoceptors expressed by cultured rat IMCD cells". Am J Physiol. 261 (5 Pt 2): F760–6. PMID 1719824.
- ↑ Wannanukul S, Chiabunkana J (2004). "Comparative study of 2% ketoconazole cream and 1% hydrocortisone cream in the treatment of infantile seborrheic dermatitis". J Med Assoc Thai. 87 Suppl 2: S68–71. PMID 16083165.
- ↑ Reygagne P, Poncet M, Sidou F, Soto P (2007). "Clobetasol propionate shampoo 0.05% in the treatment of seborrheic dermatitis of the scalp: results of a pilot study". Cutis. 79 (5): 397–403. PMID 17569404.
- ↑ Peter RU, Richarz-Barthauer U (1995). "Successful treatment and prophylaxis of scalp seborrhoeic dermatitis and dandruff with 2% ketoconazole shampoo: results of a multicentre, double-blind, placebo-controlled trial". Br J Dermatol. 132 (3): 441–5. PMID 7718463.
- ↑ Shuster S, Meynadier J, Kerl H, Nolting S (2005). "Treatment and prophylaxis of seborrheic dermatitis of the scalp with antipityrosporal 1% ciclopirox shampoo". Arch Dermatol. 141 (1): 47–52. doi:10.1001/archderm.141.1.47. PMID 15655141.
- ↑ 82.0 82.1 Kastarinen H, Oksanen T, Okokon EO, Kiviniemi VV, Airola K, Jyrkkä J; et al. (2014). "Topical anti-inflammatory agents for seborrhoeic dermatitis of the face or scalp". Cochrane Database Syst Rev (5): CD009446. doi:10.1002/14651858.CD009446.pub2. PMID 24838779.
- ↑ Shin, Hyoseung, et al. "Clinical efficacies of topical agents for the treatment of seborrheic dermatitis of the scalp: a comparative study." The Journal of dermatology 36.3 (2009): 131-137.
- ↑ Faergemann, J. "Pharmacology and Treatment Seborrhoeic dermatitis and Pityrosporumorbiculare: treatment of seborrhoeic dermatitis of the scalp with miconazole‐hydrocortisone (Daktacort), miconazole and hydrocortisone." British journal of dermatology 114.6 (1986): 695-700.
- ↑ Young Jr, A. W. "Seborrhea in the geriatric patient: incidence, implication, management." Geriatrics 24.3 (1969): 144-150.
- ↑ Gupta, Aditya K., Karyn Nicol, and Roma Batra. "Role of antifungal agents in the treatment of seborrheic dermatitis." American journal of clinical dermatology 5.6 (2004): 417-422.
- ↑ Zisova LG (2009). "Treatment of Malassezia species associated seborrheic blepharitis with fluconazole". Folia Med (Plovdiv). 51 (3): 57–9. PMID 19957565.
- ↑ Collins, Chris D., and Chad Hivnor. "Seborrheic dermatitis." management 41 (1988): 182-186.
- ↑ Geißler, Sabine E., Silke Michelsen, and Gerd Plewig. "Very low dose isotretinoin is effective in controlling seborrhea." JDDG: Journal der Deutschen Dermatologischen Gesellschaft 1.12 (2003): 952-958.
- ↑ Ballanger F, Tenaud I, Volteau C, Khammari A, Dréno B (2008). "Anti-inflammatory effects of lithium gluconate on keratinocytes: a possible explanation for efficiency in seborrhoeic dermatitis". Arch Dermatol Res. 300 (5): 215–23. doi:10.1007/s00403-007-0824-z. PMID 18330588.
- ↑ Dreno B, Moyse D (2002). "Lithium gluconate in the treatment of seborrhoeic dermatitis: a multicenter, randomised, double-blind study versus placebo". Eur J Dermatol. 12 (6): 549–52. PMID 12459525.
- ↑ "A double-blind, placebo-controlled, multicenter trial of lithium succinate ointment in the treatment of seborrheic dermatitis. Efalith Multicenter Trial Group". J Am Acad Dermatol. 26 (3 Pt 2): 452–7. 1992. PMID 1532964.
- ↑ Stevens DL, Bisno AL, Chambers HF, Dellinger EP, Goldstein EJ, Gorbach SL; et al. (2014). "Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the infectious diseases society of America". Clin Infect Dis. 59 (2): 147–59. doi:10.1093/cid/ciu296. PMID 24947530.
- ↑ "WHO Monographs on Selected Medicinal Plants - Volume 1: Aloe Vera Gel". www.who.int. Retrieved 2008-03-18.
- ↑ 95.0 95.1 95.2 95.3 95.4 95.5 95.6 "The Green Pharmacy: New Discoveries ... - Google Book Search". books.google.com. Retrieved 2008-03-19.