Sandbox: hyperthyroid: Difference between revisions
Ahmed Younes (talk | contribs) No edit summary |
Ahmed Younes (talk | contribs) |
||
| Line 5: | Line 5: | ||
==Overview== | ==Overview== | ||
[[Hormones|Thyroid hormones]] are responsible for regulating the [[basal metabolic rate]] of the body. Over secretion of thyroid hormones can lead to a wide variety of syndromes depending on the cause of the hyperthyroidism. Hyperthyroidism can be due to hyperactivity of the [[thyroid gland]] itself (primary hyperthyroidism) or due to abnormalities in the [[pituitary gland]] or the [[hypothalamus]] causing irregularities in the upper control of the gland. Hyperthyroidism can also be classified according to the results of iodine uptake study into high uptake, low uptake, and high or normal uptake. | [[Hormones|Thyroid hormones]] are responsible for regulating the [[basal metabolic rate]] of the body. Over secretion of thyroid hormones can lead to a wide variety of syndromes depending on the cause of the hyperthyroidism. Hyperthyroidism can be due to hyperactivity of the [[thyroid gland]] itself (primary hyperthyroidism) or due to abnormalities in the [[pituitary gland]] or the [[hypothalamus]] causing irregularities in the upper control of the gland. Hyperthyroidism can also be classified according to the results of iodine uptake study into high uptake, low uptake, and high or normal uptake. | ||
==Classification== | ==Classification== | ||
Revision as of 18:39, 8 August 2017
|
Sandbox: hyperthyroid Microchapters |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Ahmed Younes M.B.B.CH [2]
Overview
Thyroid hormones are responsible for regulating the basal metabolic rate of the body. Over secretion of thyroid hormones can lead to a wide variety of syndromes depending on the cause of the hyperthyroidism. Hyperthyroidism can be due to hyperactivity of the thyroid gland itself (primary hyperthyroidism) or due to abnormalities in the pituitary gland or the hypothalamus causing irregularities in the upper control of the gland. Hyperthyroidism can also be classified according to the results of iodine uptake study into high uptake, low uptake, and high or normal uptake.
Classification
According to the origin of the abnormality
Hyperthyroidism is classified according to the origin of the lesion into[1]
Primary hyperthyroidism:
Excess thyroid production from thyroid gland
Secondary hyperthyroidism:
Excess thyroid production due to disorders of the pituitary:
Tertiary hyperthyroidism:
- Excess thyroxin production due to disorders of the hypothalamus which may be due to intracranial tumors or masses.
According to iodine uptake
Hyperthyroidism can be classified according to the results of iodine uptake test into[2]
High iodine uptake
High or normal uptake:
- Iodine caused hyperthyroidism
- Hashitoxicosis
- Germ cell tumors (choriocarcinoma in males and testicular germ cell tumors)
- Pituitary TSH producing adenoma
Low uptake:
- Subacute thyroiditis
- Hyperthyroidosim due to ectopic thyroid tissue
Pathophysiology
 |
- Thyroid hormones (T3 and T4) are regulating basal metabolic rate, influence oxygen consumption by tissues. They are crucial for normal development of the brain and growth of the body, especially in prepubertal period.[3]
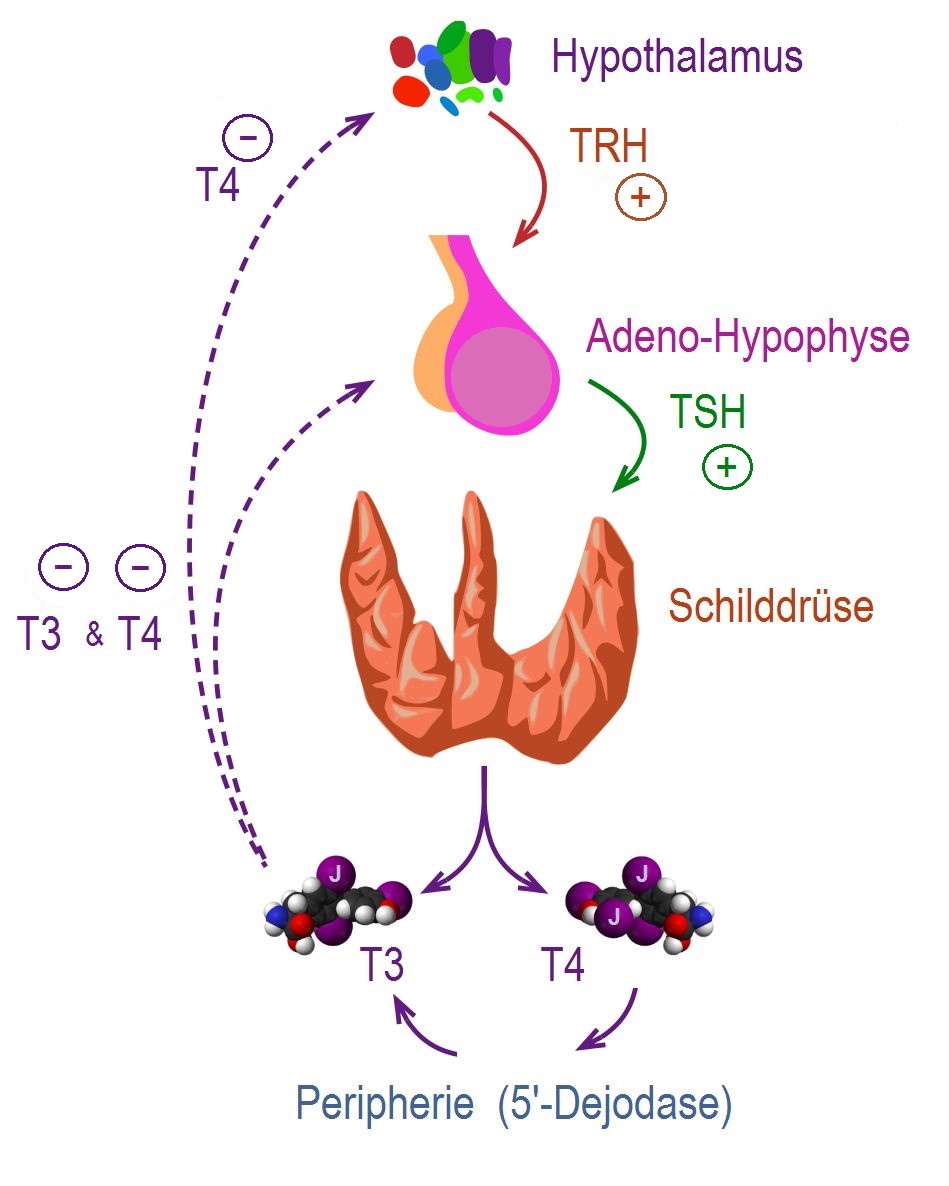
- Secretion of thyroid hormones follows upper control from the hypothalamus and the pituitary. Thyroid releasing hormone (TRH) acts on thyrotropes releasing cells in the pituitary causing them to release thyroid stimulating hormone (TSH).
- TSH acts on thyroid gland by binding to specific membrane receptors and activating an intracellular pathway involving cAMP that ends in formation and secretion of thyroid hormones.
- Iodine is essential for the synthesis of thyroid hormones. The daily iodide need is about 100mcg / day. Iodide is uptaken through a special Na/I transporter found in the membrane of thyroid follicular cell. After uptaking iodide, it goes through a series of organic reactions ending in the formation of the two forms of thyroid hormones: T3 and T4. T3 and T4 remain stored in the thyroglobulin of the follicles and are released in response to further stimulation by TSH to the thyroid follicles.
- While T3 is 3 to 5 times more potent than T4, it represents only one fourth of the total hormone secretion. T3 is thought to be the biologically active form of the of the two forms of the hormone. Most of the circulating T3 is due to peripheral conversion of T4 in the liver and peripheral tissues while only a small percentage is secreted directly from the thyroid gland itself.
- T3 and T4 act on nuclear receptors (DNA binding proteins) and cause the regulate the transcription of many proteins to regulate the metabolic rate of the body.
- The higher regulation of thyroxin secretion follows the negative feedback role, meaning that high levels of T3 and T4 will suppress TRH and TSH secretion and vice versa (Low levels of thyroxins will stimulate TRH and TSH secretion). This is useful in diagnosing the cause of hyperthyroidism (in secondary hyperthyroidism where the pituitary or the hypothalamus are the sources of the disease. TSH will be high, while in primary hyperthyroidism where the gland is the source of the excess hormones, TSH will be low).
- In graves' disease, the most common cause of hyperthyroidism. The disorder lies in the secretion of thyroid stimulating antibodies (TSI) that work on thyroid follicular cells causing an excessive uncontrolled release of the thyroxins. TSI responsible for many other aspects of the disease such as ophthalmopathy and the skin manifestations. This is thought to be due to the epitopic similarity between antigens on the surface of these cells and the thyroid receptors.[4]
- Toxic nodular goiter involves the growth of a various number of nodules (ranging from one to tens). These nodules either bleed and undergo degeneration and fibrosis followed by calcification or they might have autonomous activity producing excess thyroxin.
- The majority of circulating T3 and T4 are bound to plasma proteins and thus not active (T4 is mostly bound to thyroxine binding globulin and T3 is mostly bound to transthyretin). Conditions that impair the production of thyroid binding globulins (such as pregnancy, liver failure, and certain drug administration) cause a change in the total serum thyroxins but the free T3 and T4 remain normal and the patient remains euthyroid (this carries only laboratory significance).[5]
References
- ↑ Monaco F (2003). "Classification of thyroid diseases: suggestions for a revision". J. Clin. Endocrinol. Metab. 88 (4): 1428–32. doi:10.1210/jc.2002-021260. PMID 12679417.
- ↑ [+http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(05)72981-0/abstract "Thyroid disease classification - The Lancet"] Check
|url=value (help). - ↑ Kirsten D (2000). "The thyroid gland: physiology and pathophysiology". Neonatal Netw. 19 (8): 11–26. doi:10.1891/0730-0832.19.8.11. PMID 11949270.
- ↑ ADAMS DD (1965). "PATHOGENESIS OF THE HYPERTHYROIDISM OF GRAVES'S DISEASE". Br Med J. 1 (5441): 1015–9. PMC 2166943. PMID 14262190.
- ↑ Chopra IJ, Solomon DH (1983). "Pathogenesis of hyperthyroidism". Annu. Rev. Med. 34: 267–81. doi:10.1146/annurev.me.34.020183.001411. PMID 6134495.