ST elevation myocardial infarction histopathology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Infobox_Disease | | {{Infobox_Disease | | ||
Name = Myocardial infarction| | Name = Myocardial infarction| | ||
| Line 11: | Line 12: | ||
MeshID = | | MeshID = | | ||
}} | }} | ||
{{ST elevation myocardial infarction}} | |||
{{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} | |||
{{ | |||
{{CMG}} | |||
'''Associate Editor-In-Chief:''' {{CZ}} | |||
==Overview== | ==Overview== | ||
| Line 335: | Line 331: | ||
{{STEMI}} | {{STEMI}} | ||
[[Category:Disease]] | |||
[[Category:Cardiology]] | |||
[[Category:Ischemic heart diseases]] | |||
[[Category:Intensive care medicine]] | |||
[[Category:Emergency medicine]] | |||
[[Category:Mature chapter]] | |||
[[Category:Pathology]] | [[Category:Pathology]] | ||
Revision as of 21:09, 7 October 2012
| Myocardial infarction | |
 | |
|---|---|
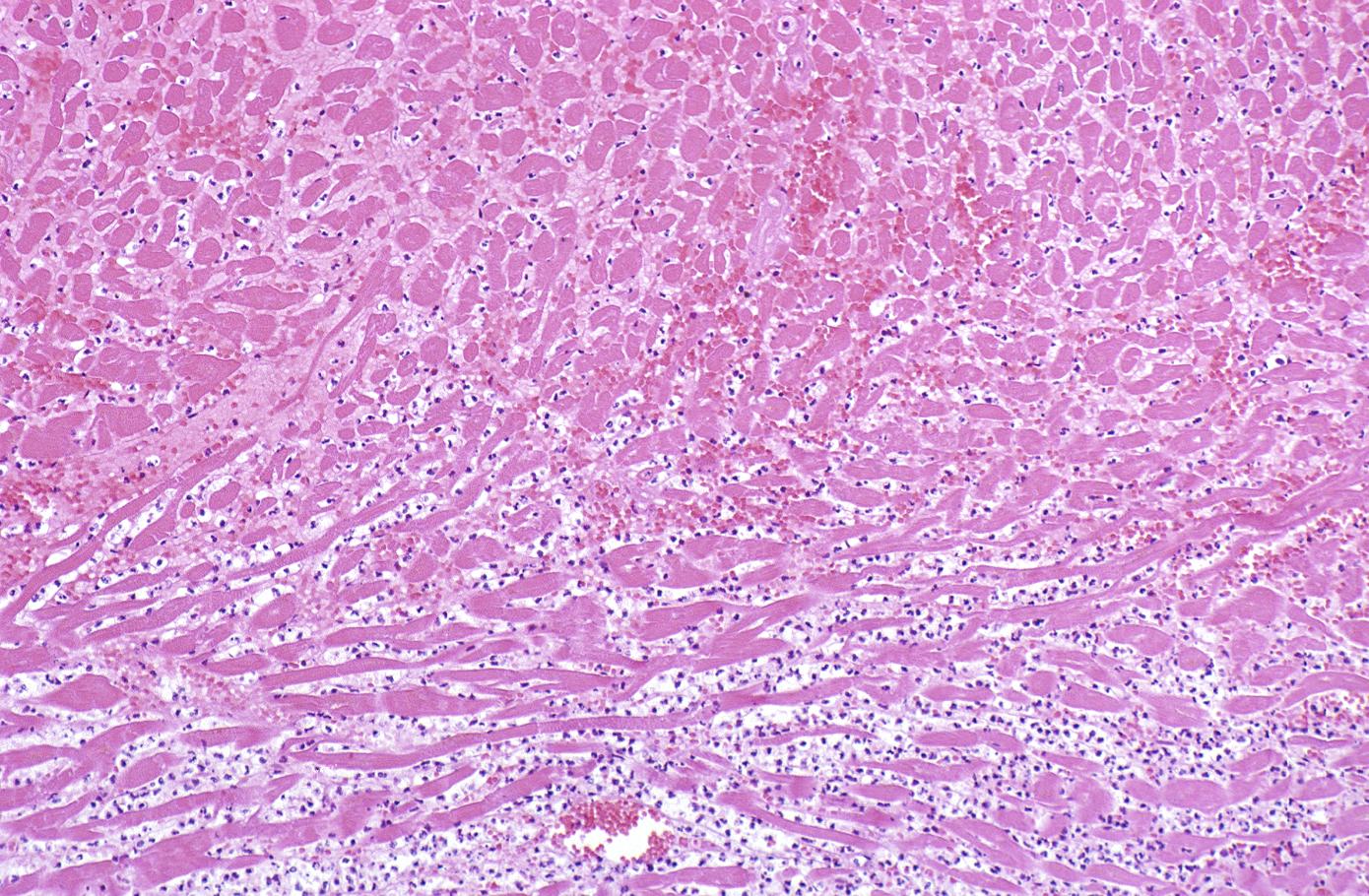
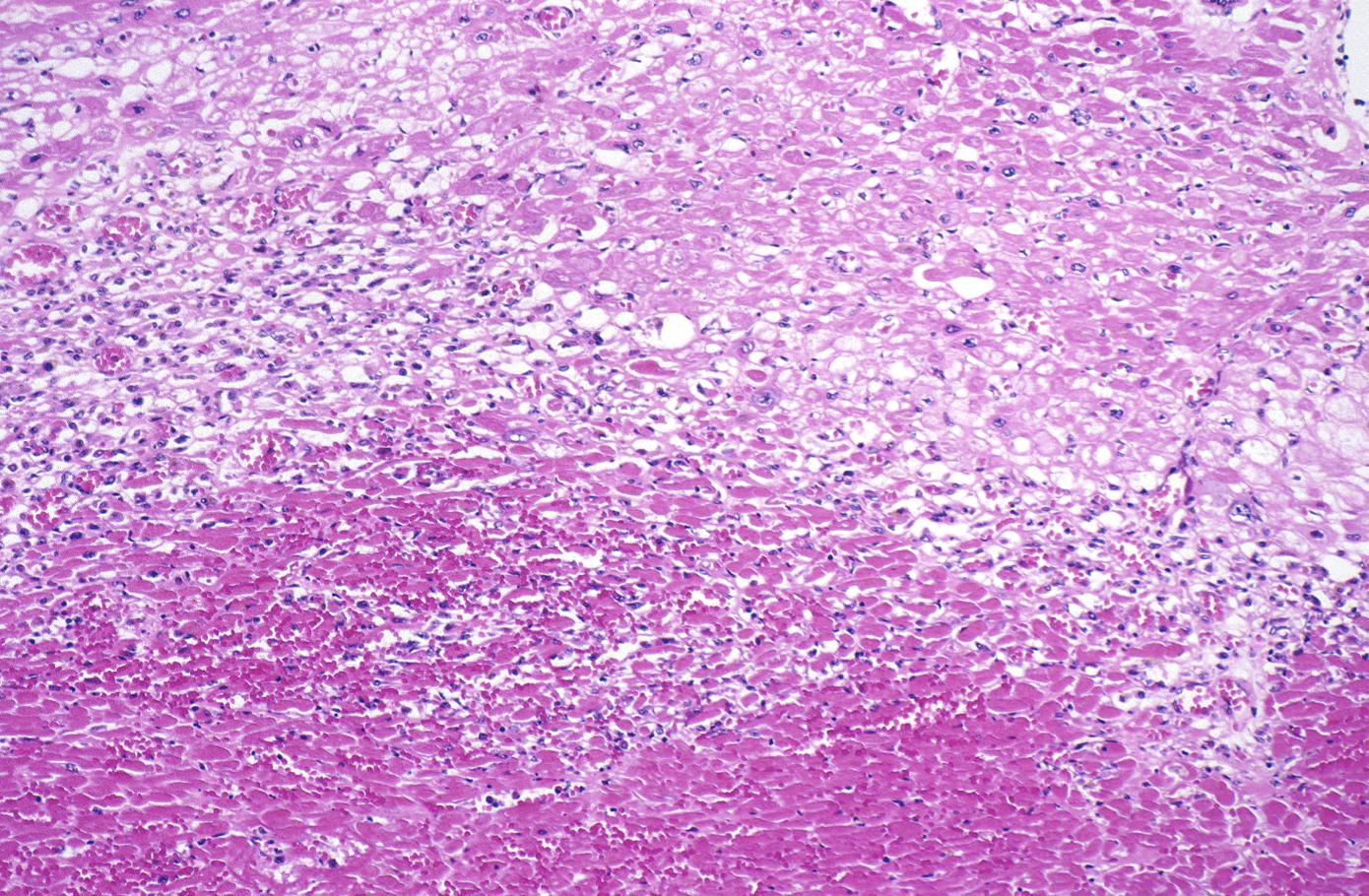
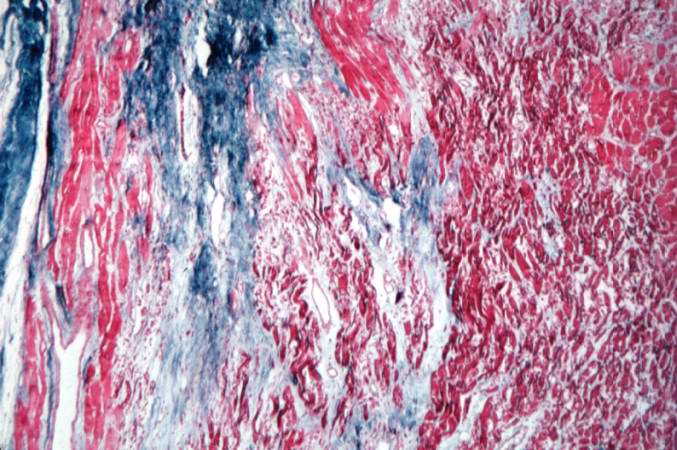
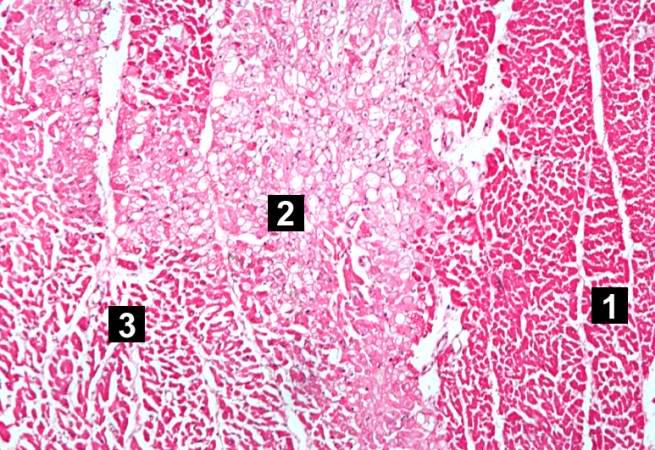
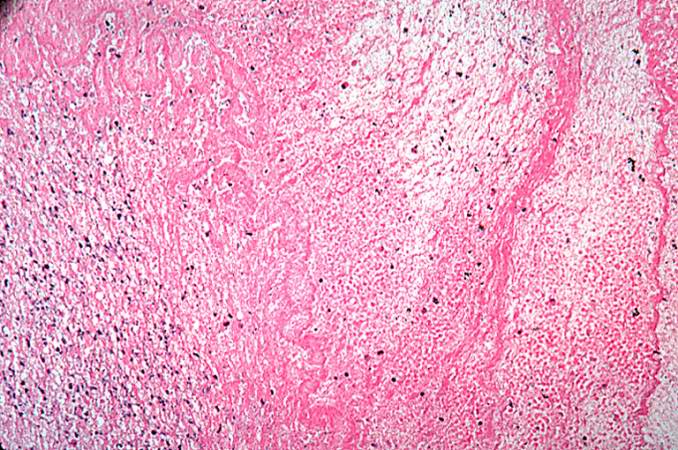
| Histopathology of myonecrosis in the emmolition phase. | |
| ICD-10 | I21-I22 |
| ICD-9 | 410 |
| DiseasesDB | 8664 |
| MedlinePlus | 000195 |
|
ST Elevation Myocardial Infarction Microchapters |
|
Differentiating ST elevation myocardial infarction from other Diseases |
|
Diagnosis |
|
Treatment |
|
|
Case Studies |
|
ST elevation myocardial infarction histopathology On the Web |
|
ST elevation myocardial infarction histopathology in the news |
|
Directions to Hospitals Treating ST elevation myocardial infarction |
|
Risk calculators and risk factors for ST elevation myocardial infarction histopathology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
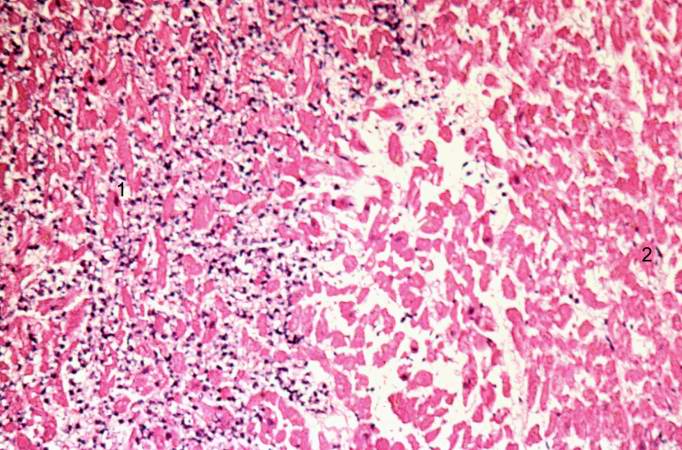
Histopathological examination of the heart may reveal infarction at autopsy. Under the microscope, myocardial infarction presents as a circumscribed area of ischemic, coagulative necrosis (cell death). On gross examination, the infarct is not identifiable within the first 12 hours.[1]
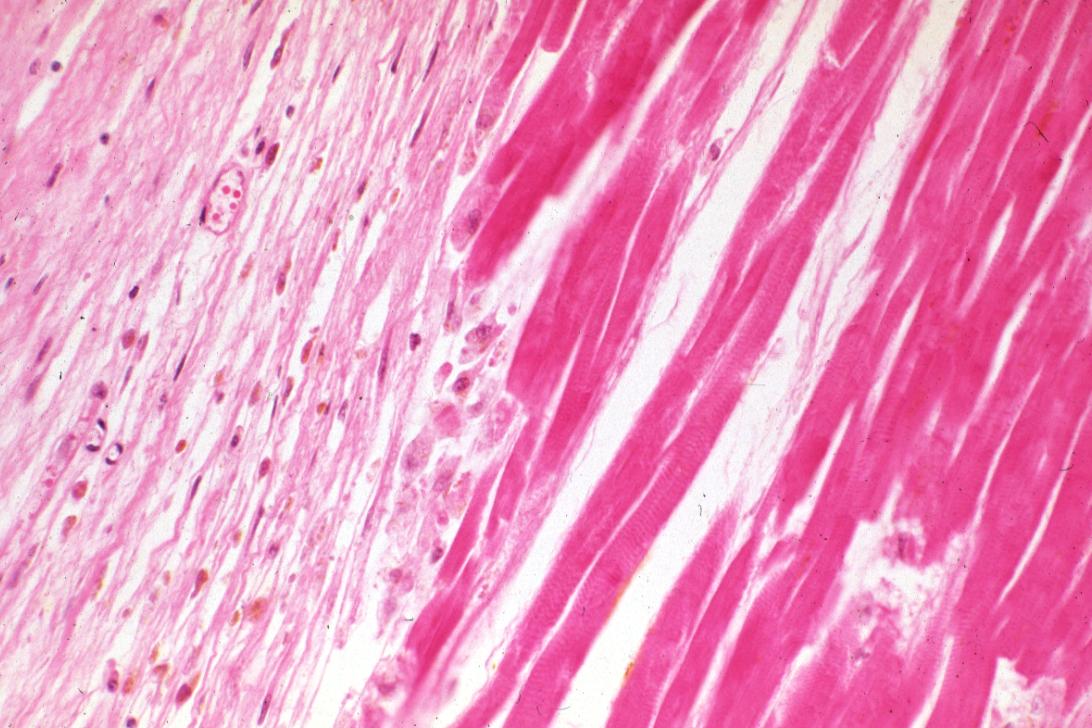
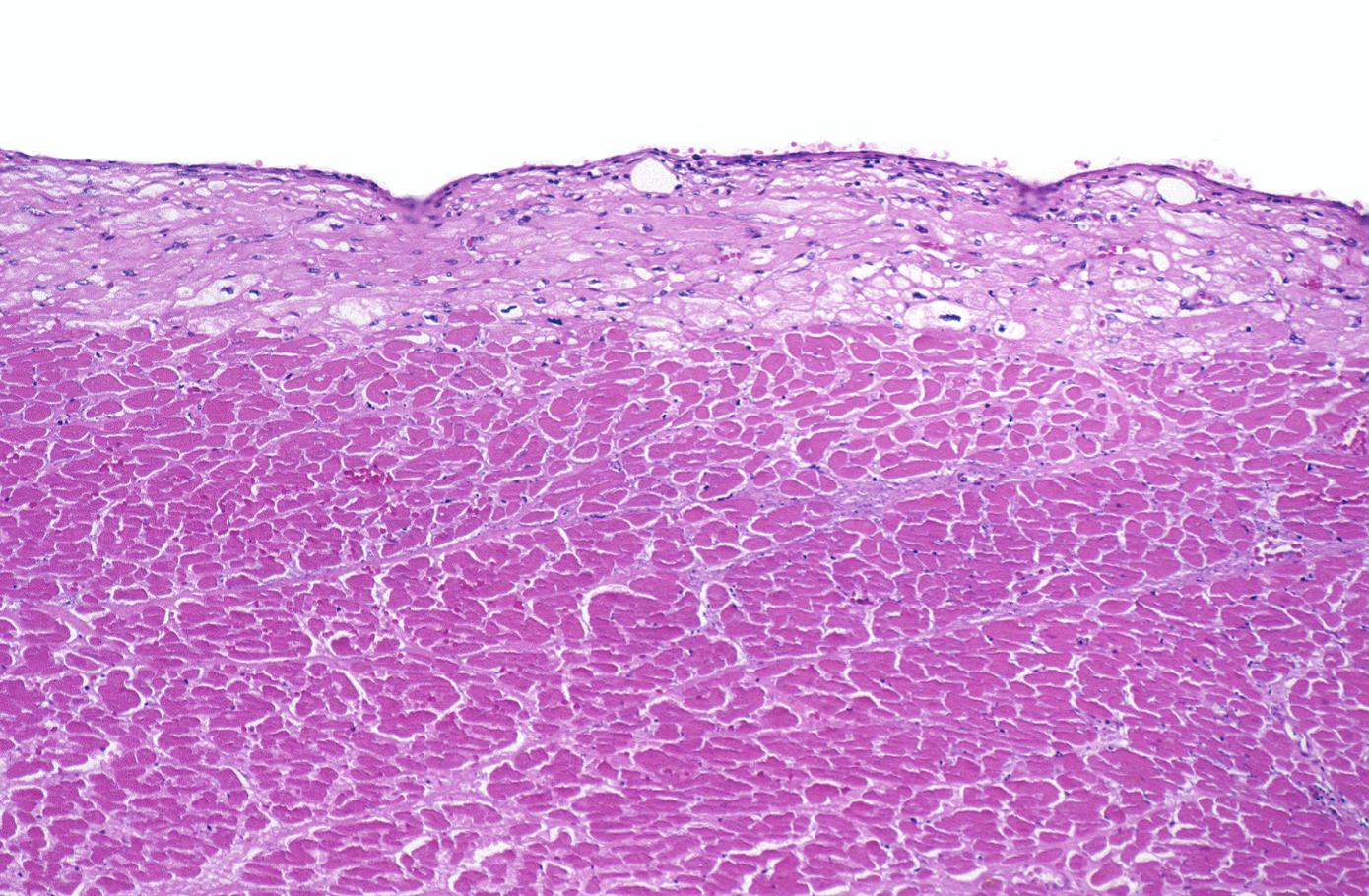
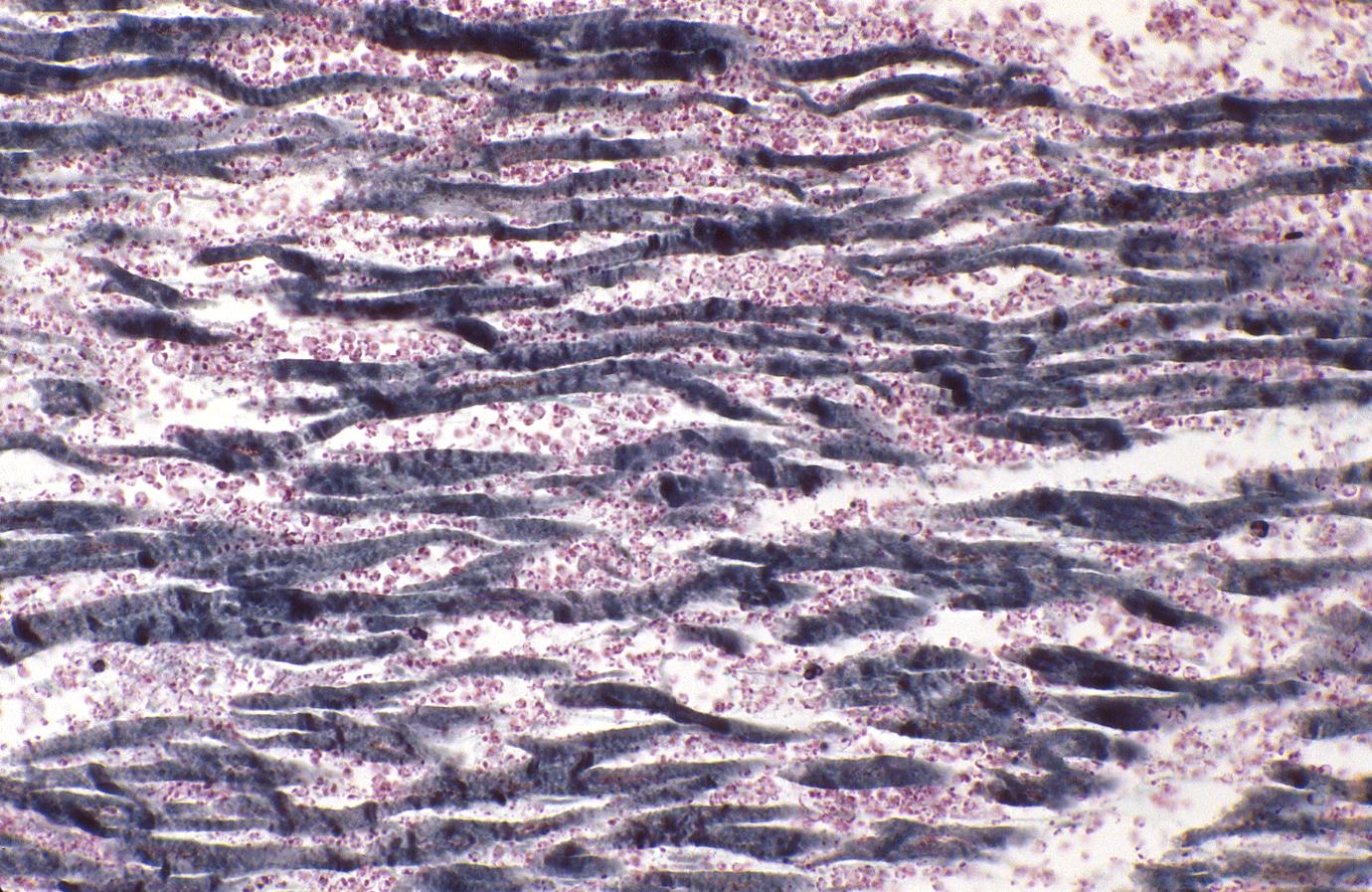
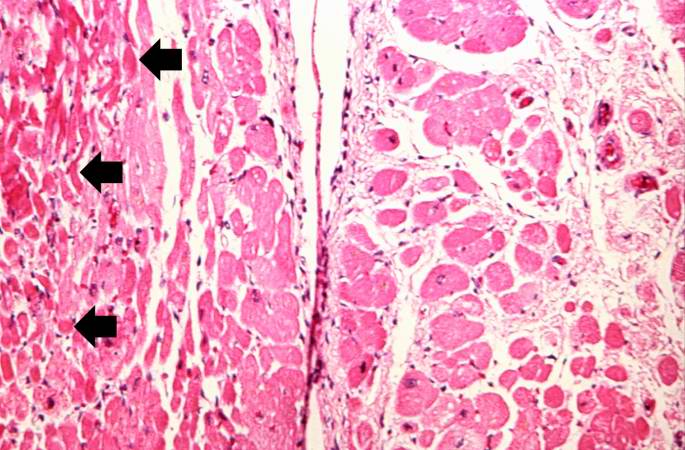
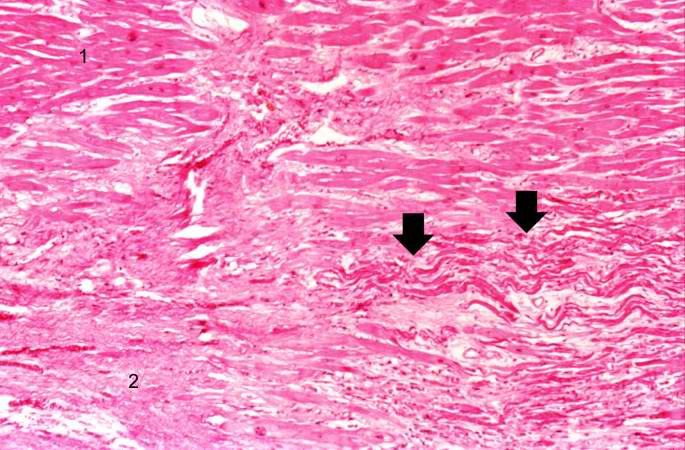
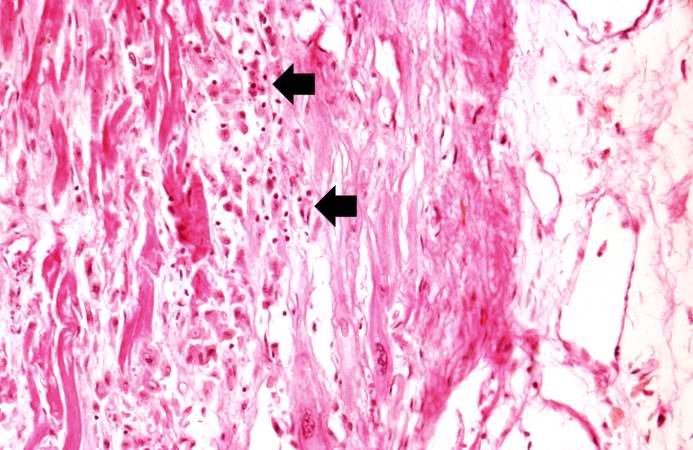
Wavy Fiber Phase
Although earlier changes can be discerned using electron microscopy, one of the earliest changes under a normal microscope are so-called wavy fibers.[2]Thin wavy myocytes are (the earliest light microscopic finding of acute myocardial infarction) visible as early as one hour following the onset of infarction. [3]
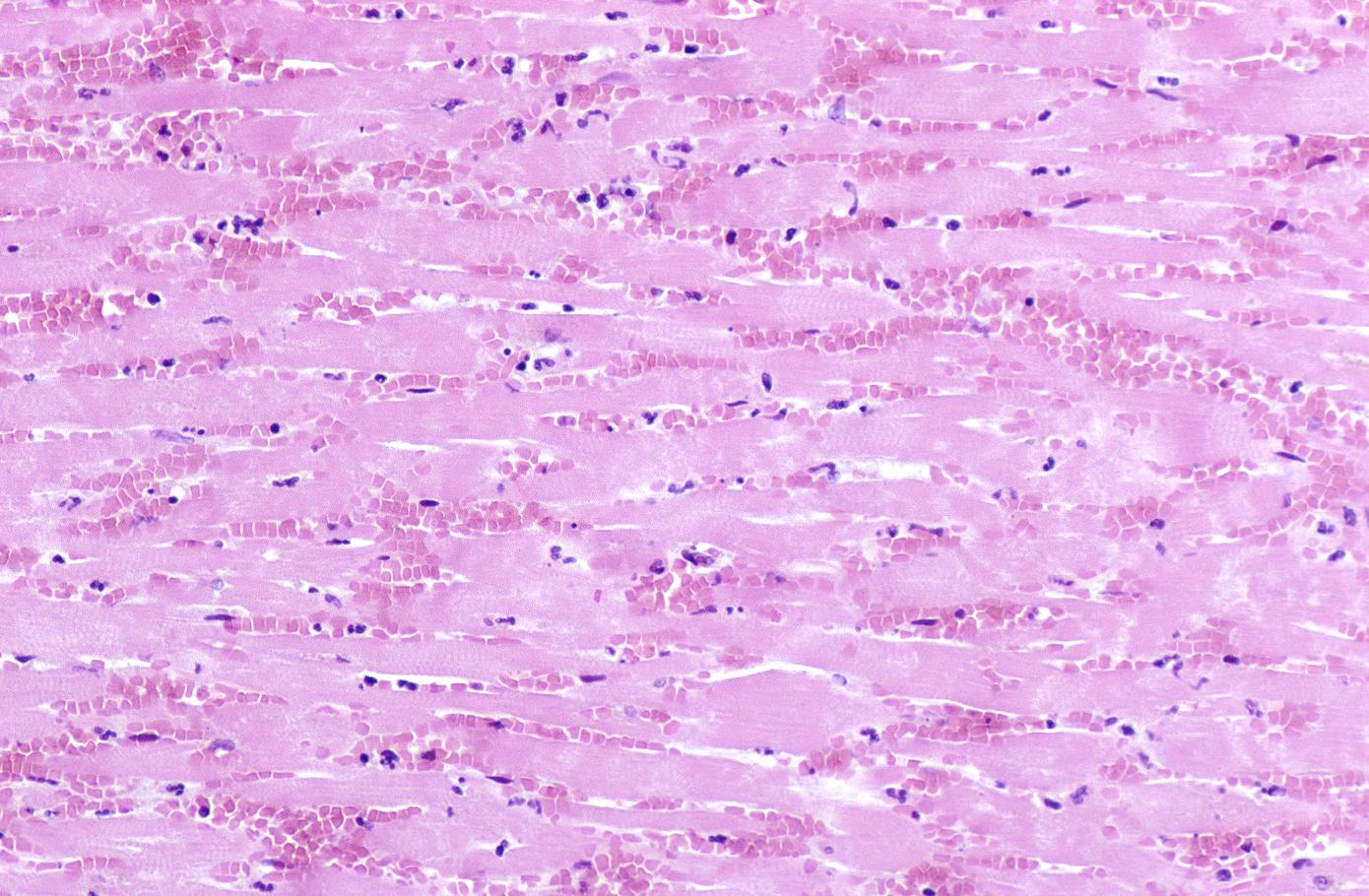
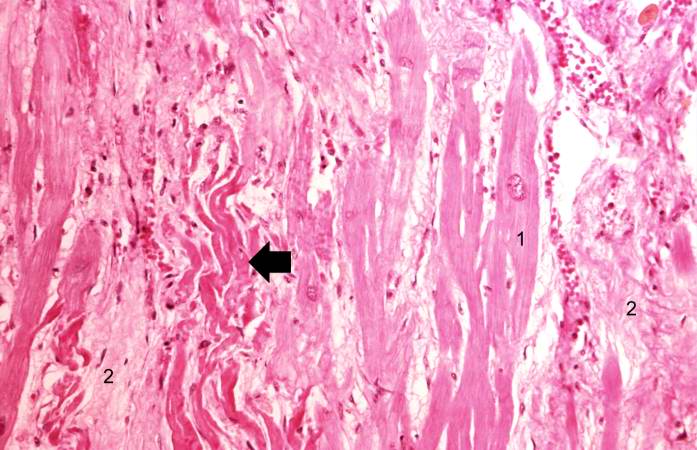
Eosinophilic Phase with Loss of Cell Nucleus
Subsequently, the myocyte cytoplasm becomes more eosinophilic (pink) and the cells lose their transversal striations, with typical changes and eventually loss of the cell nucleus.[4]
Coagulation Necrosis
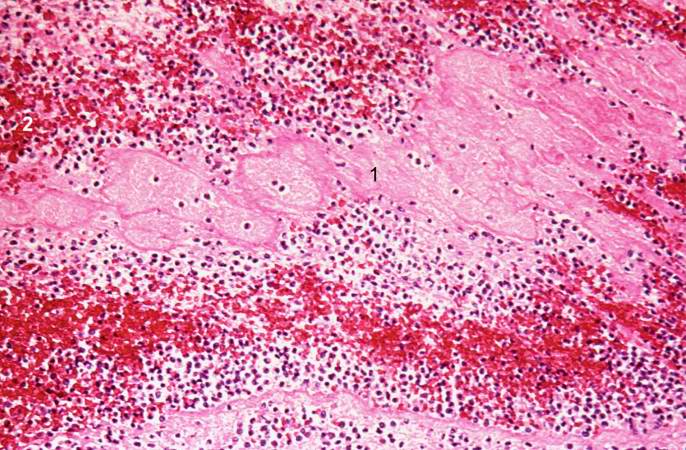
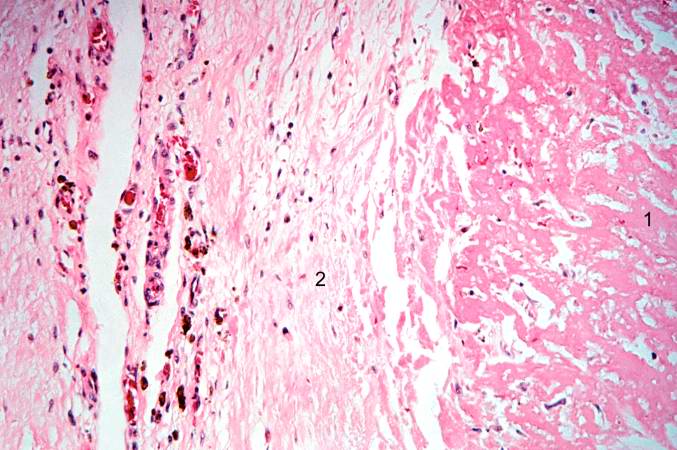
Coagulation necrosis, characterized by hypereosinophilia and nuclear pyknosis, followed by karyorrhexis, karyolysis, total loss of nuclei and loss of cytoplasmic cross-striations, is generally first visible in the period from 4-12 hours following infarction.[5]. Necrotic myocytes may retain their striations for a long time.[6]
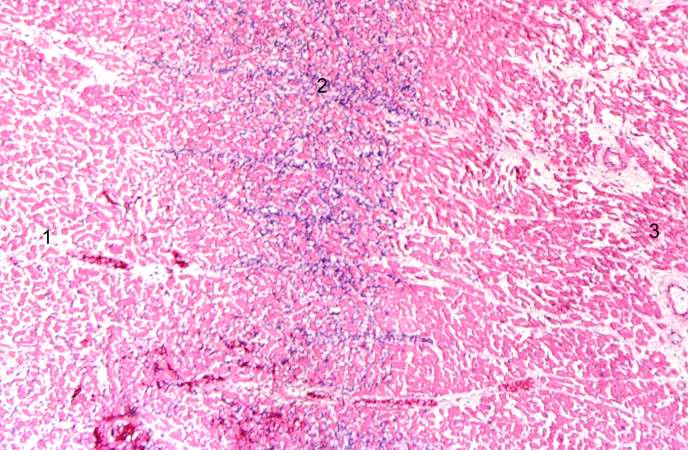
Neutrophilic infiltration (acute inflammation), edema and hemorrhage are also first visible at 4-12 hours but generally closer to 12 hours. The interstitium at the margin of the infarcted area is initially infiltrated with neutrophils, then with lymphocytes and macrophages, who phagocytose ("eat") the myocyte debris. The necrotic area is surrounded and progressively invaded by granulation tissue, which will replace the infarct with a fibrous (collagenous) scar (which are typical steps in wound healing). The interstitial space (the space between cells outside of blood vessels) may be infiltrated with red blood cells.[1]
Acute inflammation is generally present in a narrow band of the periphery at 24 hours, in a broad band of the periphery at 48 hours and tends to be maximal around 72 hours, with extensive basophilic debris from degenerating neutrophils.[6]
Infiltration by macrophages, lymphocytes, eosinophils, fibroblasts and capillaries begins around the periphery at 3-10 days. Contraction band necrosis, characterized by hypereosinophilic transverse bands of precipitated myofibrils in dead myocytes is usually seen at the edge of an infarct or with reperfusion (e.g. with thrombolytic therapy).[7]
Reperfusion of an infarct is also associated with more hemorrhage, less acute inflammation, less limitation of the acute inflammation to the periphery in the first few days, reactive stromal cells, more macrophage infiltration earlier and a more patchy distribution of necrosis, especially around the periphery.[8]
These features can be recognized in cases where the perfusion was not restored; reperfused infarcts can have other hallmarks, such as contraction band necrosis.[9]
Summary of Time from Onset and Morphologic Findings
- 1 - 3 hours: Wavy myocardial fibers
- 2 - 3 hours: Staining defect with tetrazolium or basic fuchsin dye
- 4 - 12 hours: Coagulation necrosis with loss of cross striations, contraction bands, edema, hemorrhage, and early neutrophilic infiltrate
- 18 - 24 hours: Continuing coagulation necrosis, pyknosis of nuclei, and marginal contraction bands
- 24 - 72 hours: Total loss of nuclei and striations along with heavy neutrophilic infiltrate
- 3 - 7 days: Macrophage and mononuclear infiltration begin, fibrovascular response begins
- 10 - 21 days: Fibrovascular response with prominent granulation tissue
- 7 weeks: Fibrosis
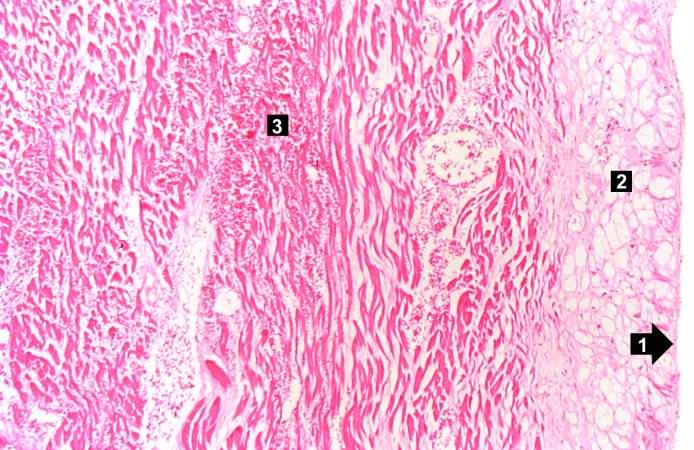
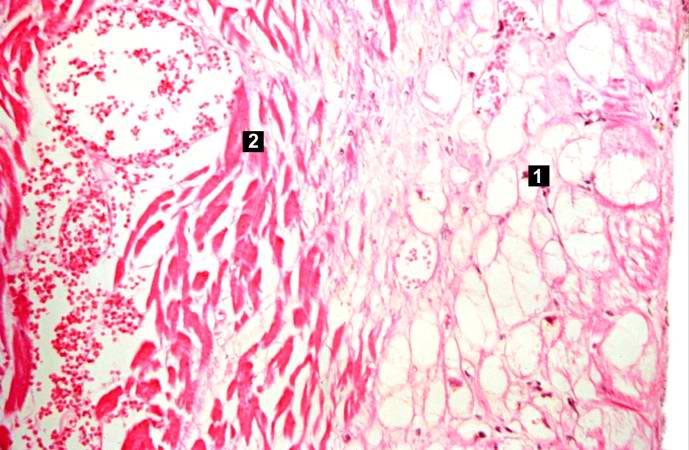
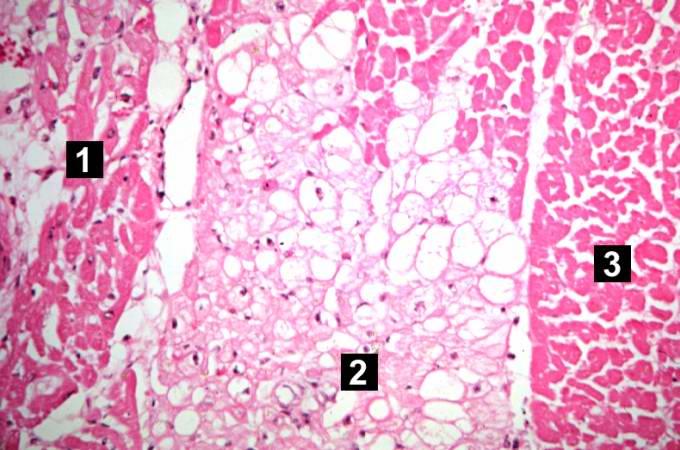
Images of Histopathological Findings
Case Examples
Case 1
Medical History, Clinical & Laboratory Findings
An 83-year-old male was admitted with the chief complaint of chest pain. He had been awakened the previous night with dull chest pain which was retrosternal and radiated through to his back. The pain was associated with sweating, nausea, and vomiting and could not be relieved by antacids. Nitroglycerin gave prompt relief.
Following admission he developed cardiac arrhythmias.
His AST was found to be 130 IU/L. In the early morning of the day after admission, he developed severe epigastric pain and several episodes of tachycardia (150-160 beats per minute) and later cardiac arrest.
There was a history of hypertension and diabetes.
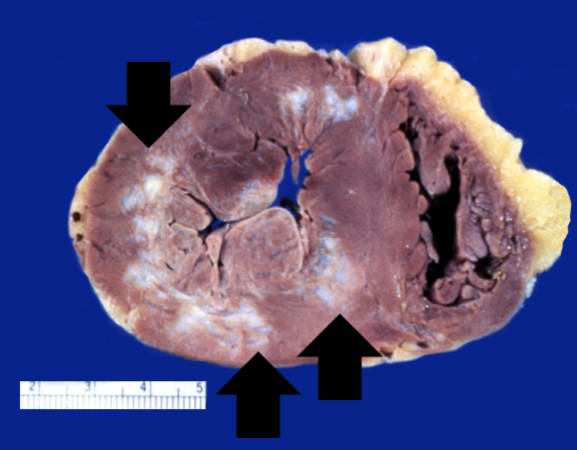
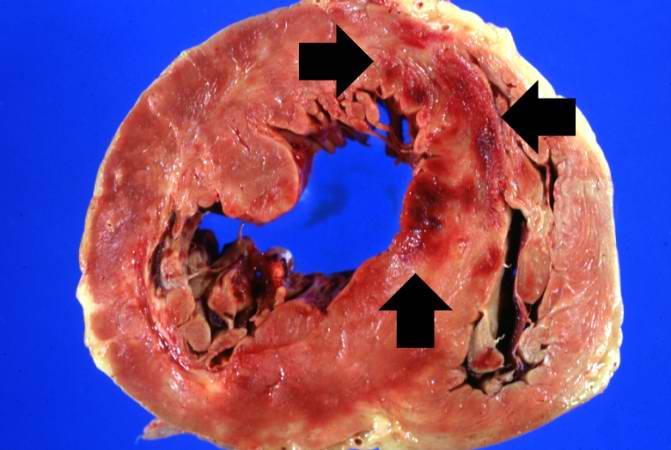
Autopsy Findings
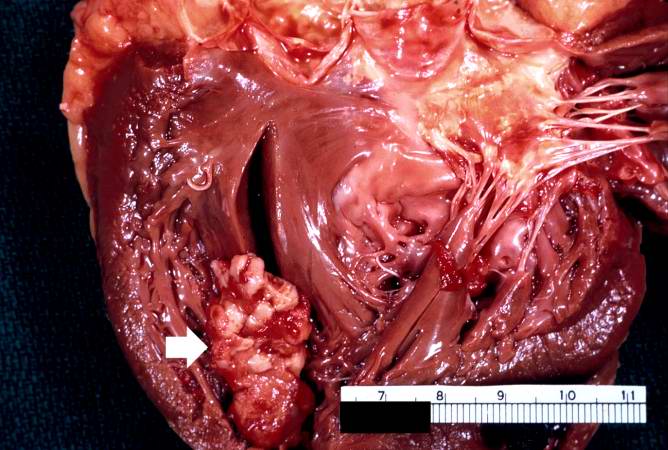
The heart weighed 500 grams.
There was massive acute myocardial infarction (about 2 days old) involving the posterior left ventricle, interventricular septum, and right ventricle from apex to base.
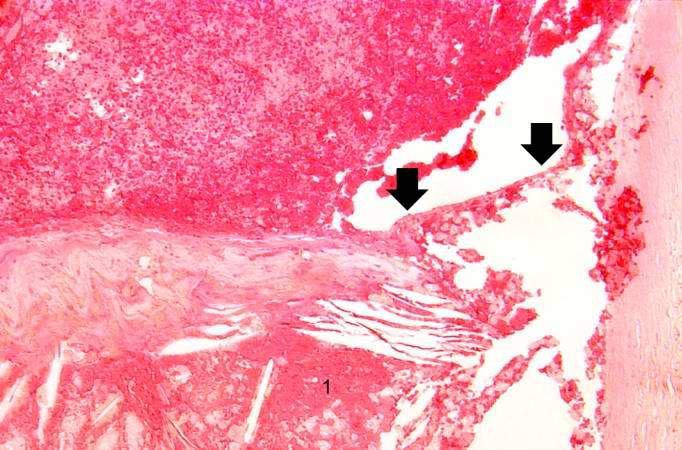
The infarct was transmural, and there was a small rupture in the soft infarcted area at the apex.
There were 1200 mL of blood within the right pleural cavity, probably secondary to this rupture.
The coronary arteries showed moderate to severe atherosclerosis throughout the coronary tree.
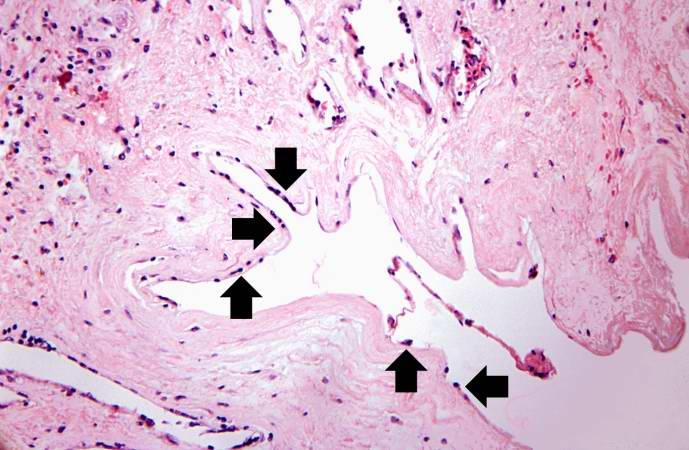
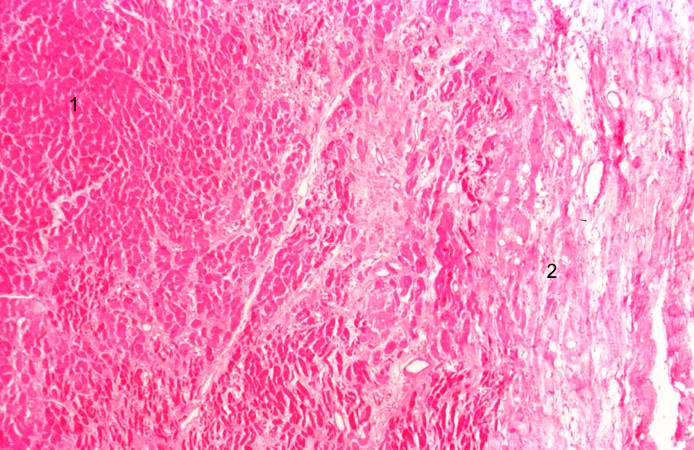
Histopathologic Findings





Case 2
Medical History, Clinical & Laboratory Findings
A 78-year-old male experienced a posterior myocardial infarction six years prior to this admission.
Recently, he had begun to experience occasional angina.
Four days prior to death, he experienced anterior chest pain and discomfort which he regarded as not too distressing.
However, EKGs showed a classic acute anterior myocardial infarction in addition to the healed posterior infarct.
The patient progressively deteriorated with left ventricular failure and died with arrhythmias and pulmonary edema. Pertinent laboratory data are:
- Aspartate aminotransferase (AST) 60 IU/L.
- Total Creatine phosphokinase (CPK) 165 IU/L. All of the activity was due to CPK III (MM) isoenzyme fraction; no CPK (MB) activity was detectable.
- Lactate dehydrogenase (LDH) 720 IU/L. LD1 fraction was greater than LD2.
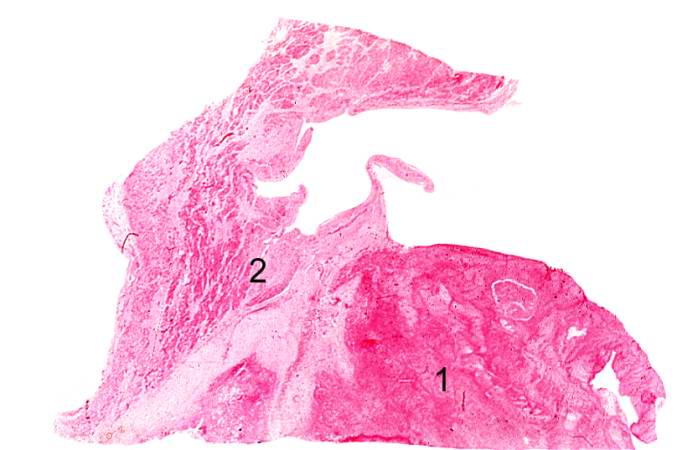
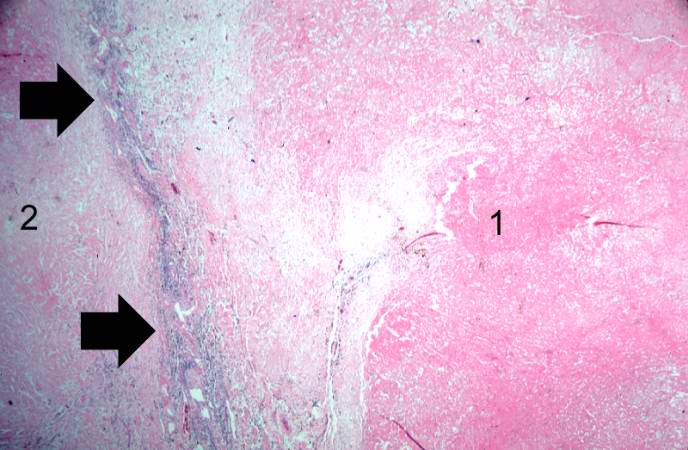
Autopsy Findings
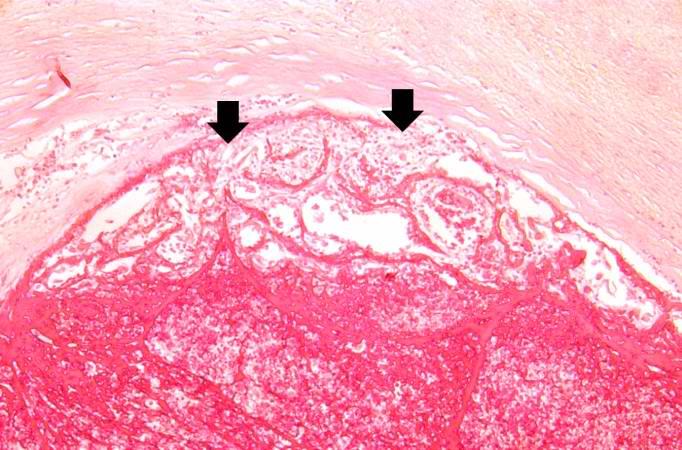
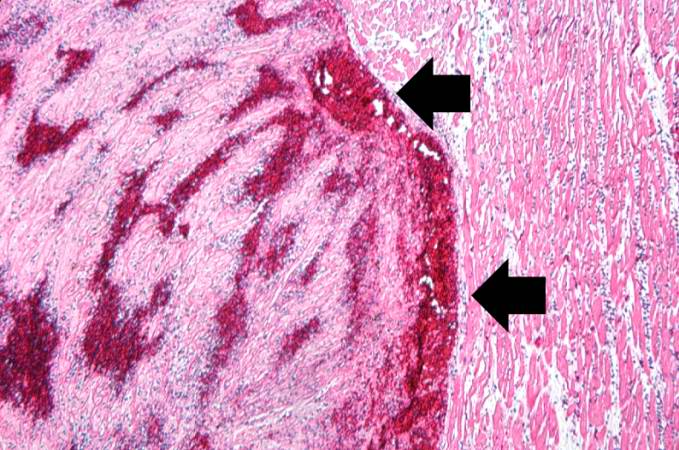
Examination of the heart showed a healed posterior infarct. The right coronary artery was completely occluded but partially recanalized. The left main coronary artery had severe atherosclerotic stenosis and a thrombus filling the lumen. The entire anterolateral aspect of the left ventricle was soft with variegated areas appearing hyperemic or pale.
There was extensive mural thrombosis and reactive pericarditis.
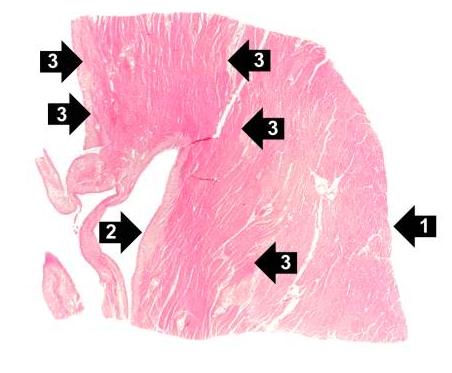
Histopathologic Findings
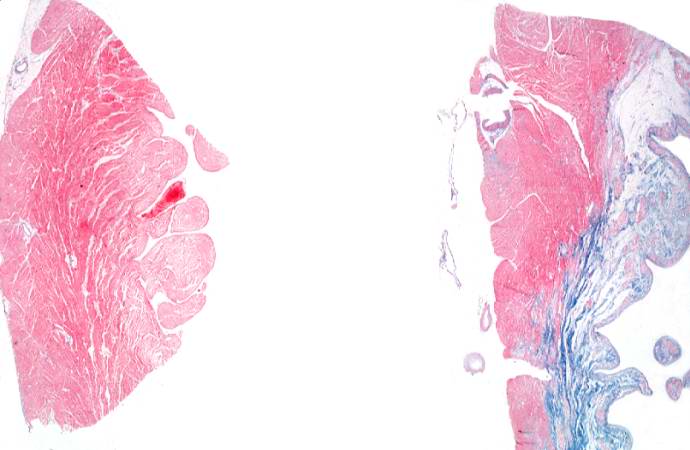
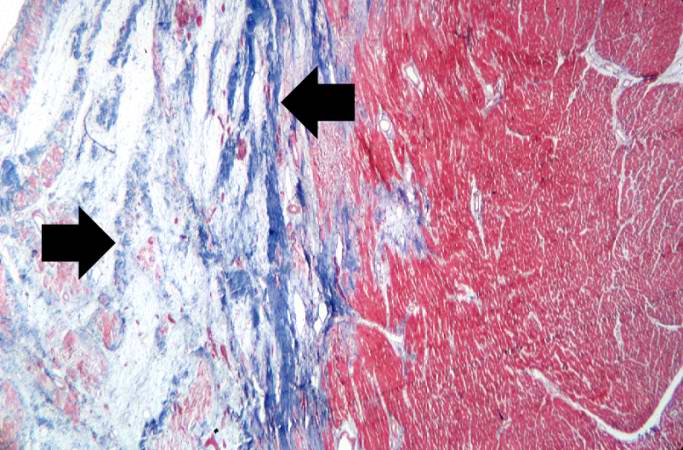
Case 3: Healed Myocardial Infarction
Medical History
A 37-year-old female with a 22 year history of insulin-dependent diabetes mellitus was admitted to the hospital 10 hours prior to death complaining of chest pain and shortness of breath.
Three months before, she had begun to experience progressive weakness and for the previous 3 weeks she noticed increasing dyspnea on exertion and worsening of a chronic cough.
Autopsy Findings
Autopsy showed a 340-gram heart with extensive transmural reddish discoloration of the anterolateral portion of the myocardium of the left ventricle.
There was severe atherosclerotic narrowing of all coronary arteries especially the left anterior descending artery.
The lungs showed pulmonary edema and early bronchopneumonia.
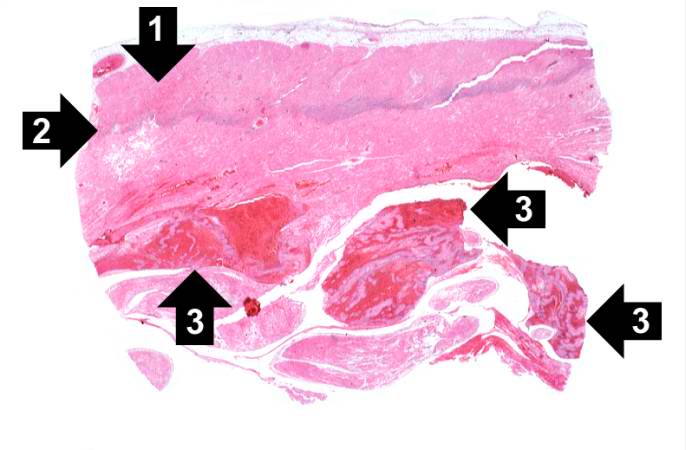
Histopathologic Findings
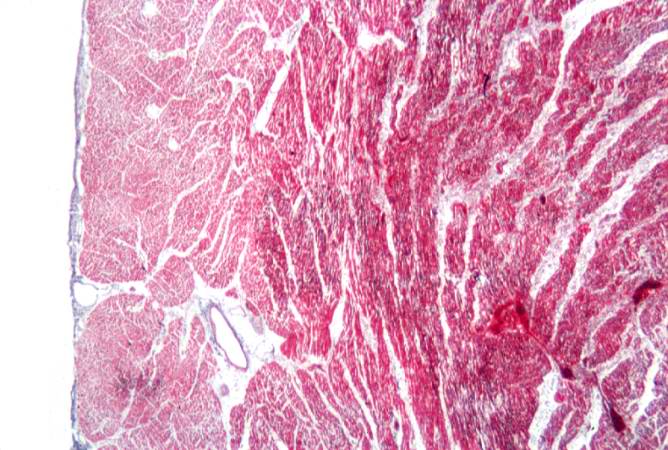
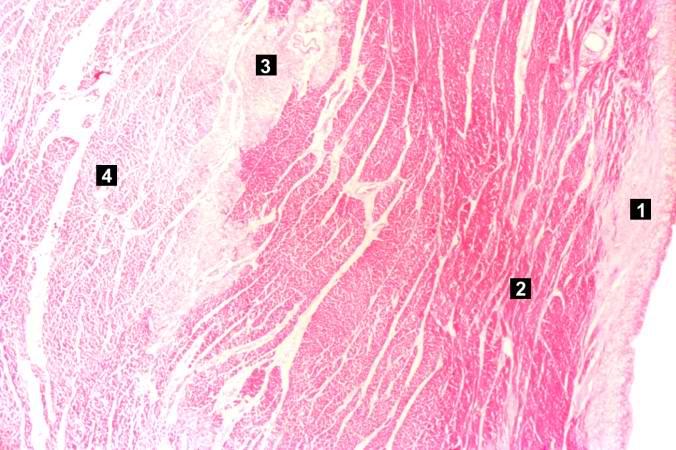
Case 4: Coagulative Necrosis
Clinical Summary
This was a 57-year-old male whose hospital course following abdominal surgery was characterized by progressive deterioration and hypotension.
Four days post-operatively, the patient sustained an anterior myocardial infarction and died the next day.
Autopsy Findings
The patient's heart weighed 410 grams.
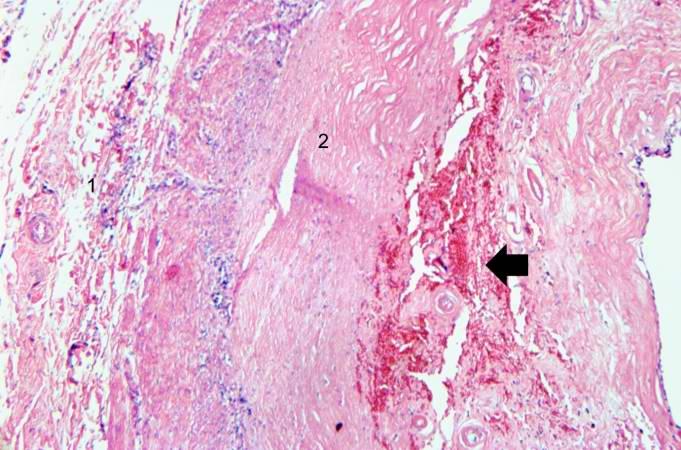
Examination of the coronary arteries revealed marked atherosclerotic narrowing of all three vessels with focal occlusion by a thrombus of the left anterior descending artery.
Fresh necrosis of the anterior wall of the left ventricle and anterior portion of the septum was present, extending from the endocardium to the inner half of the ventricular wall.
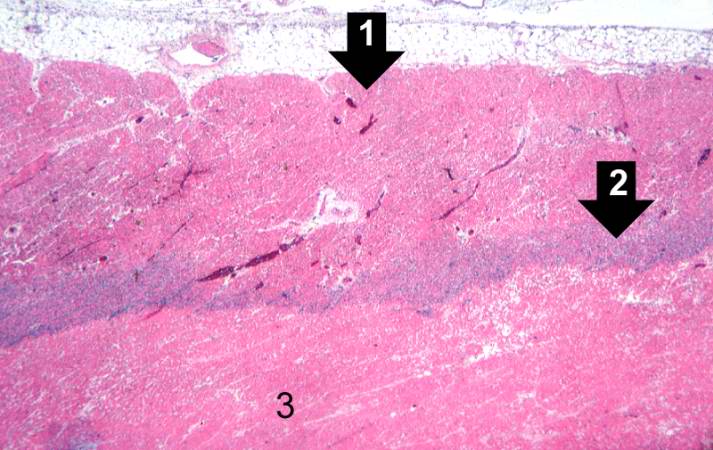
Histopathological Findings
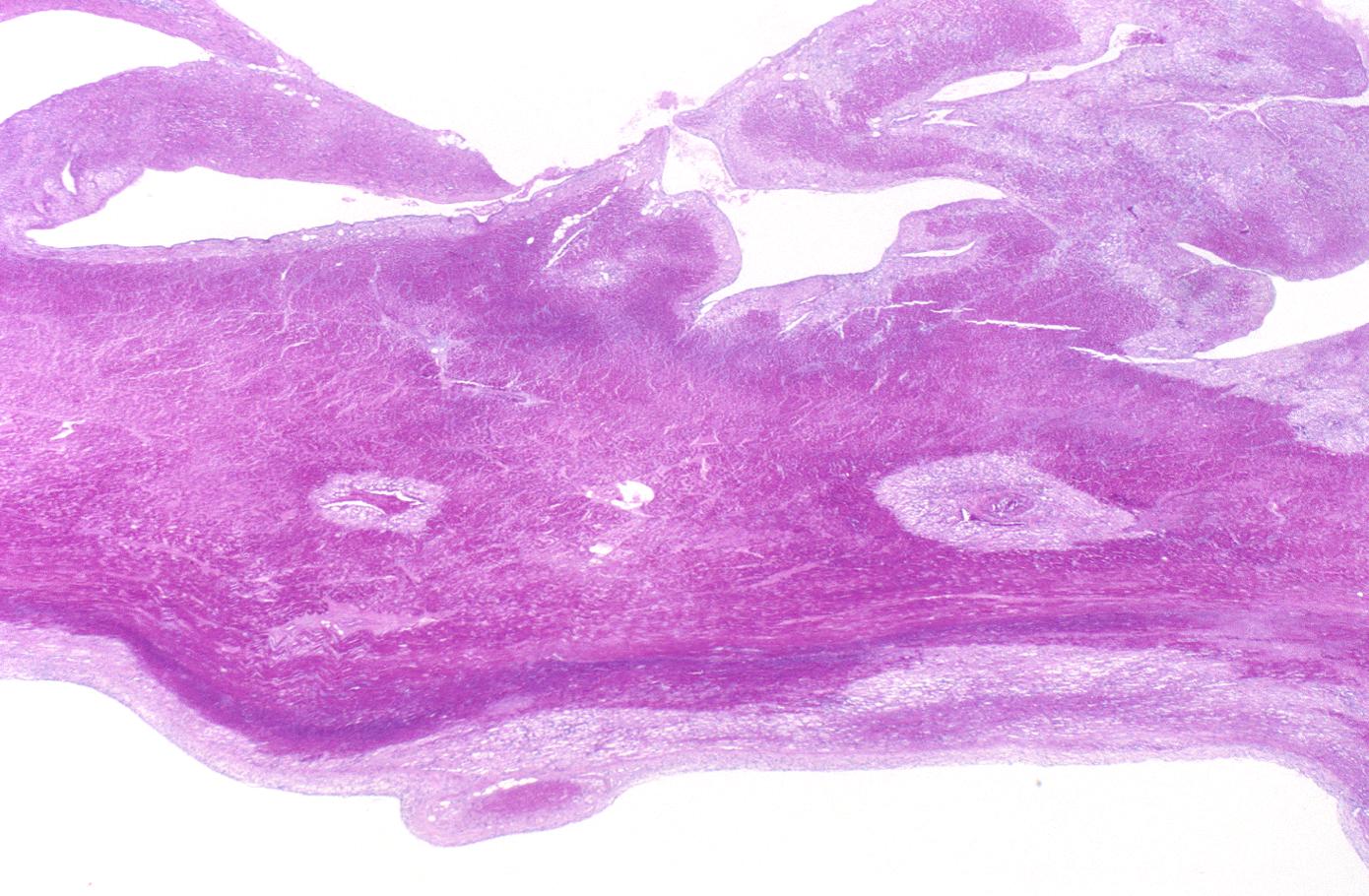
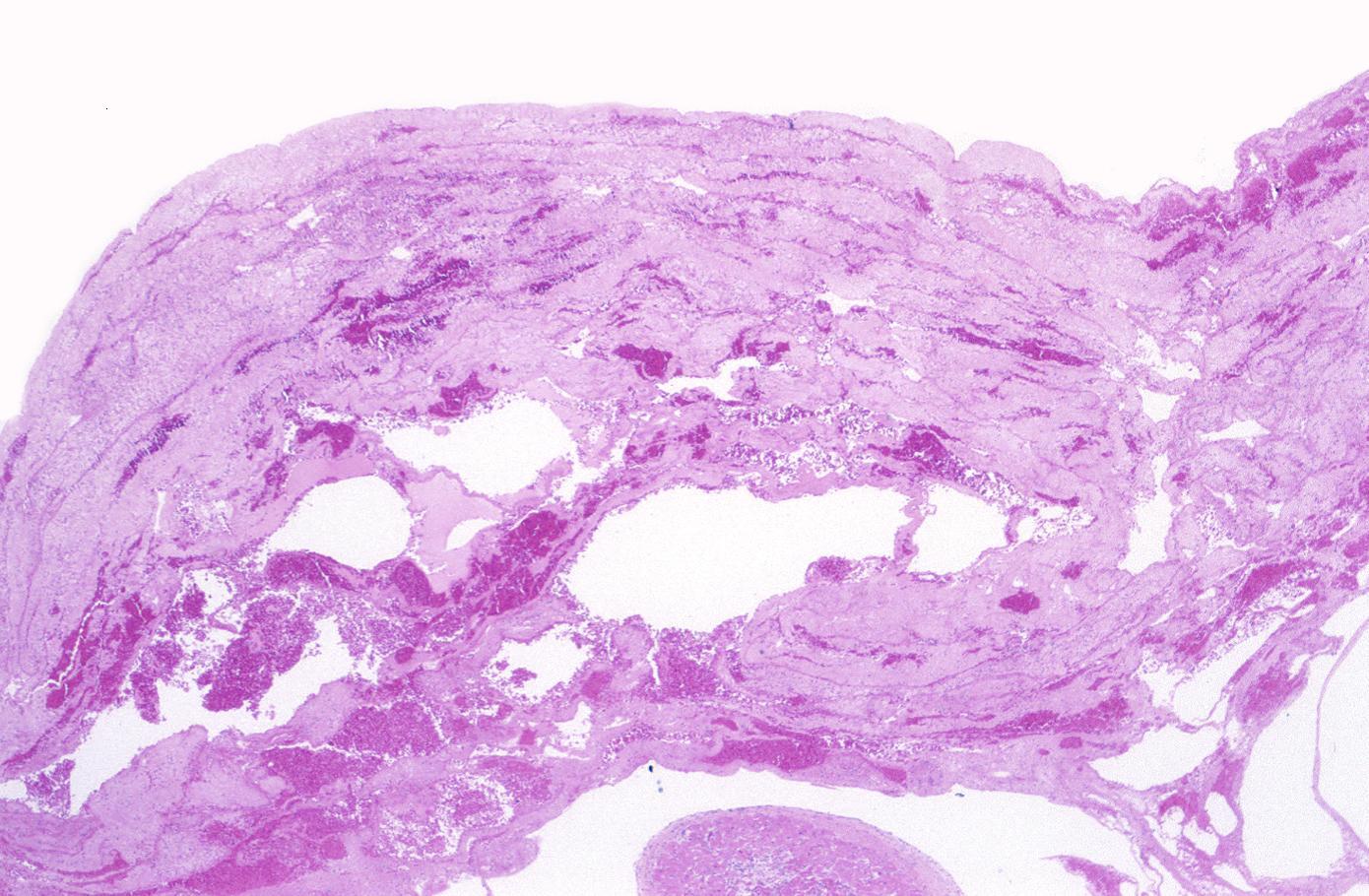
Case 5: Mural Thrombus
Clinical Summary
A 67-year-old female was transferred to the hospital from a nursing home in a comatose state.
Physical findings on examination were compatible with brain stem infarction.
On the fourth hospital day, an electrocardiogram revealed changes compatible with anterior myocardial infarction.
The patient remained comatose with quadriplegia and died on the 16th day of hospital stay.
Autopsy Findings
Examination of the brain revealed extensive infarction involving the midbrain and cerebellum with complete occlusion of the upper one-half of the basilar artery; there was also extensive coronary artery atherosclerosis.
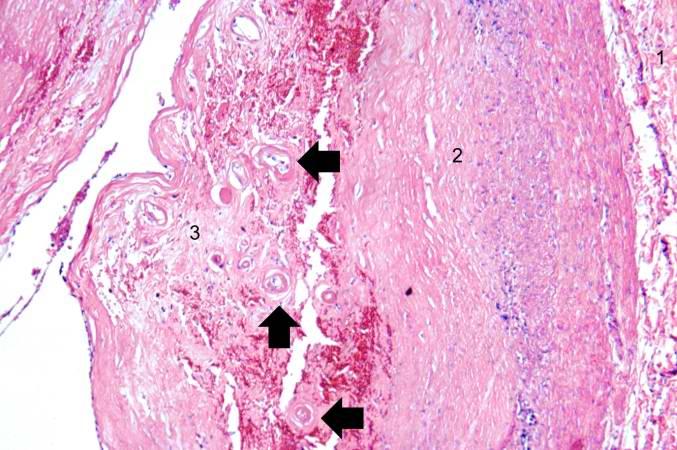
A large aneurysm of the left ventricle was present; this was filled with mural thrombus.
Extensive infarction of the lateral and posterior portions of the left ventricular wall toward the base of the heart was also found.
Histopathological Findings
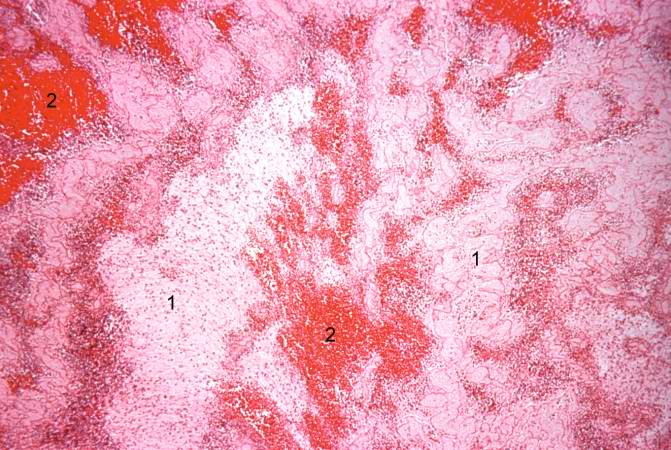
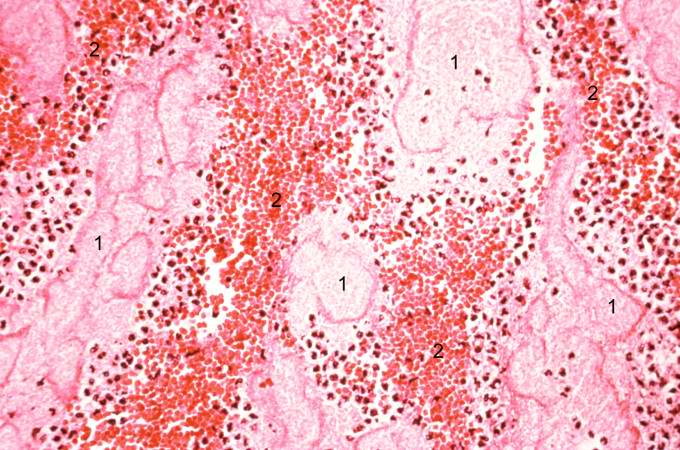
Virtual Microscopic Images
Sources
- The 2004 ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction [10]
- The 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction [11]
References
- ↑ 1.0 1.1 Rubin's Pathology - Clinicopathological Foundations of Medicine. Maryland: Lippincott Williams & Wilkins. 2001. pp. p. 546. ISBN 0-7817-4733-3. Unknown parameter
|coauthors=ignored (help) - ↑ Eichbaum FW (1975). "'Wavy' myocardial fibers in spontaneous and experimental adrenergic cardiopathies". Cardiology. 60 (6): 358–65. PMID 782705.
- ↑ Bouchardy B, Majno G (1974). "Histopathology of early myocardial infarcts. A new approach". Am. J. Pathol. 74 (2): 301–30. PMC 1910768. PMID 4359735. Unknown parameter
|month=ignored (help) - ↑ S Roy. Myocardial infarction. Retrieved November 28, 2006.
- ↑ Schoen FJ. The heart. Chapter 12 in Robbins Pathologic Basis of Disease, fifth edition, 1994, Cotran RS, Kumar V, Schoen FJ, eds., Philadelphia, W.B.Saunders, pp.517-582
- ↑ 6.0 6.1 Fishbein MC, Maclean D, Maroko PR (1978). "The histopathologic evolution of myocardial infarction". Chest. 73 (6): 843–9. PMID 657859. Unknown parameter
|month=ignored (help) - ↑ Reichenbach D, Cowan MJ. Healing of myocardial infarction with and without reperfusion. Chapter 5, in Cardiovascular Pathology, 1991, Virmani R, Atkinson JB, Fenoglio JJ, eds., Philadelphia, W.B.Saunders, pp. 86-98.
- ↑ Reichenbach D, Cowan MJ. Healing of myocardial infarction with and without reperfusion. Chapter 5, in Cardiovascular Pathology, 1991, Virmani R, Atkinson JB, Fenoglio JJ, eds., Philadelphia, W.B.Saunders, pp. 86-98.
- ↑ Fishbein MC (1990). "Reperfusion injury". Clin Cardiol. 13 (3): 213–7. PMID 2182247. Unknown parameter
|month=ignored (help) - ↑ Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK (2004). "ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction)". Circulation. 110 (9): e82–292. PMID 15339869. Unknown parameter
|month=ignored (help) - ↑ Antman EM, Hand M, Armstrong PW; et al. (2008). "2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee". Circulation. 117 (2): 296–329. doi:10.1161/CIRCULATIONAHA.107.188209. PMID 18071078. Unknown parameter
|month=ignored (help)