Prostate cancer: Difference between revisions
| Line 45: | Line 45: | ||
==[[Prostate cancer risk factors|Risk factors]]== | ==[[Prostate cancer risk factors|Risk factors]]== | ||
===High Intensity Focused Ultrasound (HIFU)=== | ===High Intensity Focused Ultrasound (HIFU)=== | ||
Revision as of 18:38, 15 December 2011
For patient information click here
Template:DiseaseDisorder infobox
|
Prostate cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Prostate cancer On the Web |
|
American Roentgen Ray Society Images of Prostate cancer |
Steven C. Campbell, M.D., Ph.D. Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [1] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Symptoms
Pathophysiology
Causes
Treatment
Treatment for prostate cancer may involve watchful waiting, surgery, radiation therapy including brachytherapy (prostate brachytherapy) and external beam radiation, High Intensity Focused Ultrasound (HIFU), chemotherapy, cryosurgery, hormonal therapy, or some combination. Which option is best depends on the stage of the disease, the Gleason score, and the PSA level. Other important factors are the man's age, his general health, and his feelings about potential treatments and their possible side effects. Because all treatments can have significant side effects, such as erectile dysfunction and urinary incontinence, treatment discussions often focus on balancing the goals of therapy with the risks of lifestyle alterations.
The selection of treatment options may be a complex decision involving many factors. For example, radical prostatectomy after primary radiation failure is a very technically challenging surgery and may not be an option.[1] This may enter into the treatment decision.
If the cancer has spread beyond the prostate, treatment options significantly change, so most doctors who treat prostate cancer use a variety of nomograms to predict the probability of spread. Treatment by watchful waiting, HIFU, radiation therapy, cryosurgery, and surgery are generally offered to men whose cancer remains within the prostate. Hormonal therapy and chemotherapy are often reserved for disease which has spread beyond the prostate. However, there are exceptions: radiation therapy may be used for some advanced tumors, and hormonal therapy is used for some early stage tumors. Cryotherapy, hormonal therapy, and chemotherapy may also be offered if initial treatment fails and the cancer progresses.
Medical therapy | Surgical options | Metastasis Treatment | Primary prevention | Secondary prevention | Financial costs | Future therapies
Screening
Diagnosis
When a man has symptoms of prostate cancer, or a screening test indicates an increased risk for cancer, more invasive evaluation is offered.
The only test which can fully confirm the diagnosis of prostate cancer is a biopsy, the removal of small pieces of the prostate for microscopic examination. However, prior to a biopsy, several other tools may be used to gather more information about the prostate and the urinary tract. Cystoscopy shows the urinary tract from inside the bladder, using a thin, flexible camera tube inserted down the urethra. Transrectal ultrasonography creates a picture of the prostate using sound waves from a probe in the rectum.
- History and Symptoms | Physical Examination | Staging | Lab Studies | Electrocardiogram | X Ray | MRI | CT | Echocardiography | Other imaging findings | Other diagnostic studies
Risk factors
High Intensity Focused Ultrasound (HIFU)
HIFU for prostate cancer utilizes high intensity focused ultrasound (HIFU) to ablate/destroy the tissue of the prostate. During the HIFU procedure, sound waves are used to heat the prostate tissue thus destroying the cancerous cells. Essentially, ultrasonic waves are precisely focused on specific areas of the prostate to eliminate the prostate cancer with minimal risks of affecting other tissue or organs. Temperatures at the focal point of the sound waves can exceed 100 °C (212 °F).[2] In lay terms, the HIFU technology is similar to using a magnifying glass to burn a piece of paper by focusing sunlight at a small precise point on the sheet. The ability to focus the ultrasonic waves leads to a relatively low occurrence of both incontinence and impotence. (0.6% and 0-20%, respectively)[3] According to international studies, when compared to other procedures, HIFU has a high success rate with a reduced risk of side effects. Studies using the Sonablate 500 HIFU machine have shown that 94% of patients with a pretreatment PSA (Prostate Specific Antigen) of less than 10 ng/mL were cancer-free after three years.[3] However, many studies of HIFU were performed by manufacturers of HIFU devices, or members of manufacturers' advisory panels.[4]
HIFU was first used in the 1940s and 1950s in efforts to destroy tumors in the central nervous system. Since then, HIFU has been shown to be effective at destroying malignant tissue in the brain, prostate, spleen, liver, kidney, breast, and bone.[2] Today, the HIF procedure for prostate cancer is performed using a transrectal probe. This procedure has been performed for over ten years and is currently approved for use in Japan, Europe, Canada, and parts of Central and South America.
Although not yet approved for use in the Unites States, many patients have received the HIFU procedure at facilities in Canada, and Central and South America. Currently, therapy is available using the Sonablate 500 or the Ablatherm. The Sonablate 500 is designed by Focus Surgery of Indianapolis, Indiana and is used in international HIFU centers around the world.
Prognosis
Prostate cancer rates are higher and prognosis poorer in developed countries than the rest of the world. Many of the risk factors for prostate cancer are more prevalent in the developed world, including longer life expectancy and diets high in red meat and dairy products (although it must be noted, that people who consume larger amounts of meat and dairy, also tend to consume fewer portions of fruits and vegetables. It's not currently known whether or not both of this factors, or just one of them, contributes to the occurrence of prostate cancer).[5] Also, where there is more access to screening programs, there is a higher detection rate. Prostate cancer is the ninth most common cancer in the world, but is the number one non-skin cancer in United States men. Prostate cancer affected eighteen percent of American men and caused death in three percent in 2005.[6] In Japan, death from prostate cancer was one-fifth to one-half the rates in the United States and Europe in the 1990s.[7] In India in the 1990s, half of the people with prostate cancer confined to the prostate died within ten years.[8] African-American men have 50–60 times more prostate cancer and prostate cancer deaths than men in Shanghai, China.[9] In Nigeria, two percent of men develop prostate cancer and 64% of them are dead after two years.[10]
In patients who undergo treatment, the most important clinical prognostic indicators of disease outcome are stage, pre-therapy PSA level and Gleason score. In general, the higher the grade and the stage, the poorer the prognosis. Nomograms can be used to calculate the estimated risk of the individual patient. The predictions are based on the experience of large groups of patients suffering from cancers at various stages.[11]
Progression
In 1941, Charles Huggins reported that androgen ablation therapy causes regression of primary and metastatic androgen-dependent prostate cancer.[12] Androgen ablation therapy causes remission in 80-90% of patients undergoing therapy, resulting in a median progression-free survival of 12 to 33 months. After remission an androgen-independent phenotype typically emerges, where the median overall survival is 23–37 months from the time of initiation of androgen ablation therapy.[13] The actual mechanism contributes to the progression of prostate cancer is not clear and may vary between individual patient. A few possible mechanisms have been proposed.[14] Scientists have established a few prostate cancer cell lines to investigate the mechanism involved in the progression of prostate cancer. LNCaP, PC-3, and DU-145 are commonly used prostate cancer cell lines. The LNCaP cancer cell line was established from a human lymph node metastatic lesion of prostatic adenocarcinoma. PC-3 and DU-145 cells were established from human prostatic adenocarcinoma metastatic to bone and to brain, respectively. LNCaP cells express androgen receptor (AR), however, PC-3 and DU-145 cells express very little or no AR. AR, an androgen-activated transcription factor, belongs to the steroid nuclear receptor family. Development of the prostate is dependent on androgen signaling mediated through AR, and AR is also important during the development of prostate cancer. The proliferation of LNCaP cells is androgen-dependent but the proliferation of PC-3 and DU-145 cells is androgen-insensitive.Elevation of AR expression is often observed in advanced prostate tumors in patients.[15][16] Some androgen-independent LNCaP sublines have been developed from the ATCC androgen-dependent LNCaP cells after androgen deprivation for study of prostate cancer progression. These androgen-independent LNCaP cells have elevated AR expression and express prostate specific antigen upon androgen treatment. Androgens paradoxically inhibit the proliferation of these androgen-independent prostate cancer cells.[17][18][19] Androgen at a concentration of 10-fold higher than the physiological concentration has also been shown to cause growth suppression and reversion of androgen-independent prostate cancer xenografts or androgen-independent prostate tumors derived in vivo model to an androgen-stimulated phenotype in athymic mice.[20][21] These observation suggest the possibility to use androgen to treat the development of relapsed androgen-independent prostate tumors in patients. Oral infusion of green tea polyphenols, a potential alternative therapy for prostate cancer by natural compounds, has been shown to inhibit the development, progression, and metastasis as well in autochthonous transgenic adenocarcinoma of the mouse prostate (TRAMP) model, which spontaneously develops prostate cancer.[22]
Epidemiology
Rates of prostate cancer vary widely across the world. Although the rates vary widely between countries, it is least common in South and East Asia, more common in Europe, and most common in the United States.[23] According to the American Cancer Society, prostate cancer is least common among Asian men and most common among black men, with figures for white men in-between.[24][25] However, these high rates may be affected by increasing rates of detection.[26]
Prostate cancer develops most frequently in men over fifty. This cancer can occur only in men, as the prostate is exclusively of the male reproductive tract. It is the most common type of cancer in men in the United States, where it is responsible for more male deaths than any other cancer, except lung cancer. In the United Kingdom it is also the second most common cause of cancer death after lung cancer, where around 35,000 cases are diagnosed every year and of which around 10,000 die of it. However, many men who develop prostate cancer never have symptoms, undergo no therapy, and eventually die of other causes. That is because malignant neoplasms of the prostate are, in most cases, slow-growing, and because most of those affected are over 60. Hence they often die of causes unrelated to the prostate cancer, such as heart/circulatory disease, pneumonia, other unconnected cancers or old age. Many factors, including genetics and diet, have been implicated in the development of prostate cancer. The Prostate Cancer Prevention Trial found that finasteride reduces the incidence of prostate cancer rate by 30%. There had been a controversy about this also increasing the risk of more aggressive cancers, but more recent research showed this was not the case.[27][28]
History

Although the prostate was first described by Venetian anatomist Niccolò Massa in 1536, and illustrated by Flemish anatomist Andreas Vesalius in 1538, prostate cancer was not identified until 1853.[29] Prostate cancer was initially considered a rare disease, probably because of shorter life expectancies and poorer detection methods in the 19th century. The first treatments of prostate cancer were surgeries to relieve urinary obstruction.[30] Removal of the entire gland (radical perineal prostatectomy) was first performed in 1904 by Hugh H. Young at Johns Hopkins Hospital.[31] Surgical removal of the testes (orchiectomy) to treat prostate cancer was first performed in the 1890s, but with limited success. Transurethral resection of the prostate (TURP) replaced radical prostatectomy for symptomatic relief of obstruction in the middle of the 20th century because it could better preserve penile erectile function. Radical retropubic prostatectomy was developed in 1983 by Patrick Walsh.[32] This surgical approach allowed for removal of the prostate and lymph nodes with maintenance of penile function.
In 1941 Charles B. Huggins published studies in which he used estrogen to oppose testosterone production in men with metastatic prostate cancer. This discovery of "chemical castration" won Huggins the 1966 Nobel Prize in Physiology or Medicine.[33] The role of the hormone GnRH in reproduction was determined by Andrzej W. Schally and Roger Guillemin, who both won the 1977 Nobel Prize in Physiology or Medicine for this work.
Receptor agonists, such as leuprolide and goserelin, were subsequently developed and used to treat prostate cancer.[34][35]
Radiation therapy for prostate cancer was first developed in the early 20th century and initially consisted of intraprostatic radium implants. External beam radiation became more popular as stronger radiation sources became available in the middle of the 20th century. Brachytherapy with implanted seeds was first described in 1983.[36] Systemic chemotherapy for prostate cancer was first studied in the 1970s. The initial regimen of cyclophosphamide and 5-fluorouracil was quickly joined by multiple regimens using a host of other systemic chemotherapy drugs.[37]
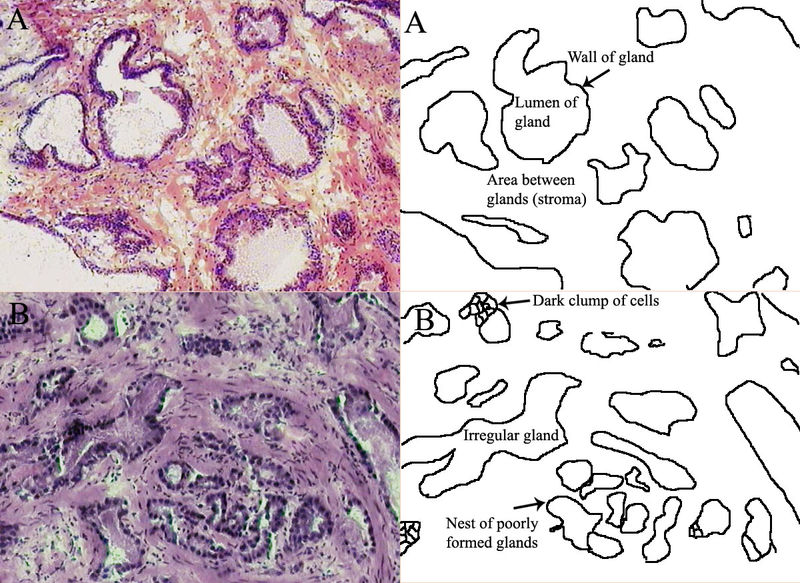
Histopathological Findings in Prostatic Adenocarcinoma
Prostate: Adenocarcinoma
<youtube v=1SZPLS1dxTo/>
Prostate: Adenocarcinoma (Gleason grading system)
Prostate: Adenocarcinoma (Gleason grade 1)
<youtube v=F7V0Zl7a2FY/>
Prostate : Adenocarcinoma (Gleason grade 2)
<youtube v=YSOLiSklIXw/>
Prostate : Adenocarcinoma (Gleason grade 3)
<youtube v=TG8vR_pE7yA/>
Prostate: Adenocarcinoma (Gleason grade 4)
<youtube v=R2Cl4HScdGc/>
Prostate: Adenocarcinoma (Gleason grade 5)
<youtube v=F7V0Zl7a2FY/>
See also
References
- ↑ Mouraviev V, Evans B, Polascik TJ (2006). "Salvage prostate cryoablation after primary interstitial brachytherapy failure: a feasible approach". Prostate Cancer Prostatic Dis. 9 (1): 99–101. doi:10.1038/sj.pcan.4500853. PMID 16314889.
- ↑ 2.0 2.1 Thomas A. Gardner and Michael A Koch, Indiana University Medical Center, Indianapolis. Prostate Cancer Therapy with High-Intensity Focused Ultrasound-Comprehensive Review. Clinical Genitourinary Cancer Vol 4. No.3, 2005.
- ↑ 3.0 3.1 Toyoaki Uchida, et al. Five years experience of transrectal high-intensity focused ultrasound using the Sonablate device in the treatment of localized prostate cancer. Dept of Urology University of Tokai Hachioji Hospital. International Journal of Urology
- ↑ Tom Pickles, Larry Goldenberg, Gary Steinhoff. High Intensity Focused Ultrasound for Prostate Cancer. British Columbia Cancer Agency http://www.bccancer.bc.ca/NR/rdonlyres/08EA1C8E-4345-4C7E-A83A-1F84853A1C27/8101/HIFUreport2005Feb10revised1.pdf
- ↑ ACS :: What Are The Risk Factors for Prostate Cancer?
- ↑ Jemal, A (2005). "Cancer statistics, 2005". CA Cancer J Clin. 55 (1): 10–30. PMID 15661684. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) Erratum in: CA Cancer J Clin. 2005 Jul-Aug;55(4):259. - ↑ Wakai, K (2005). "Descriptive epidemiology of prostate cancer in Japan and Western countries". Nippon Rinsho. 63 (2): 207–12. PMID 15714967. Unknown parameter
|month=ignored (help) Review. Template:Ja icon - ↑ Yeole, BB (2001). "Population based survival from prostate cancer in Mumbai (Bombay), India". Indian J Cancer. 38 (2–4): 126–32. PMID 1259345. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) - ↑ Hsing, AW (2000). "International trends and patterns of prostate cancer incidence and mortality". Int J Cancer. 85 (1): 60–7. doi:10.1002/(SICI)1097-0215(20000101)85:1<60::AID-IJC11>3.0.CO;2-B. PMID 10585584. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) - ↑ Osegbe, DN (1997). "Prostate cancer in Nigerians: facts and nonfacts". J Urol. 157 (4): 1340–3. doi:10.1016/S0022-5347(01)64966-8. PMID 9120935. Unknown parameter
|month=ignored (help) - ↑ Di Blasio CJ, Rhee AC, Cho D, Scardino PT, Kattan MW (2003). "Predicting clinical end points: treatment nomograms in prostate cancer". Semin Oncol. 30 (5): 567–86. doi:10.1016/S0093-7754(03)00351-8. PMID 14571407.
- ↑ Huggins C, Steven RE and Hodges CV, Studies on prostatic cancer. Arch. Sug. 43:209–223, 1941.
- ↑ Hellerstedt BA and Pienta KJ, The current state of hormonal therapy for prostate cancer, CA Cancer J. Clin. 52: 154–179, 2002.PMID 12018929
- ↑ Feldman BJ, Feldman D. The development of androgen-independent prostate cancer. Nat Rev Cancer. 2001 Oct;1(1):34–45. PMID 11900250
- ↑ Linja MJ, Savinainen KJ, Saramaki OR, Tammela TL, Vessella RL, Visakorpi T. Amplification and overexpression of androgen receptor gene in hormone-refractory prostate cancer. Cancer Res. 2001 May 1;61(9):3550–5. PMID 11325816
- ↑ Ford OH 3rd, Gregory CW, Kim D, Smitherman AB, Mohler JL. Androgen receptor gene amplification and protein expression in recurrent prostate cancer. J Urol. 2003 Nov;170(5):1817–21.PMID 14532783
- ↑ Kokontis J, Takakura K, Hay N, Liao S. Increased androgen receptor activity and altered c-myc expression in prostate cancer cells after long-term androgen deprivation. Cancer Res. 1994 March 15;54(6):1566–73. PMID 7511045
- ↑ Umekita Y, Hiipakka RA, Kokontis JM, Liao S. Human prostate tumor growth in athymic mice: inhibition by androgens and stimulation by finasteride. Proc Natl Acad Sci U S A. 1996 October 15;93(21):11802-7. PMID 8876218
- ↑ Kokontis JM, Hsu S, Chuu CP, Dang M, Fukuchi J, Hiipakka RA, Liao S. Role of androgen receptor in the progression of human prostate tumor cells to androgen independence and insensitivity. Prostate. 2005 December 1;65(4):287-98. PMID 16015608
- ↑ Chuu CP, Hiipakka RA, Fukuchi J, Kokontis JM, Liao S. Androgen causes growth suppression and reversion of androgen-independent prostate cancer xenografts to an androgen-stimulated phenotype in athymic mice. Cancer Res. 2005 March 15;65(6):2082–4. PMID 15781616
- ↑ Chuu CP, Hiipakka RA, Kokontis JM, Fukuchi J, Chen RY, Liao S. Inhibition of tumor growth and progression of LNCaP prostate cancer cells in athymic mice by androgen and liver X receptor agonist. Cancer Res. 2006 July 1;66(13):6482–6. PMID 16818617
- ↑ Gupta S, Hastak K, Ahmad N, Lewin JS, Mukhtar H. Inhibition of prostate carcinogenesis in TRAMP mice by oral infusion of green tea polyphenols. Proc Natl Acad Sci U S A. 2001 August 28;98(18):10350-5. PMID 11504910
- ↑ "IARC Worldwide Cancer Incidence Statistics—Prostate". JNCI Cancer Spectrum. Oxford University Press. December 19, 2001. Retrieved on 2007-04-05 through the Internet Archive
- ↑ Overview: Prostate Cancer—What Causes Prostate Cancer? American Cancer Society (2006-05-02). Retrieved on 2007-04-05
- ↑ Prostate Cancer FAQs. State University of New York School of Medicine Department of Urology (2006-08-31). Retrieved on 2007-04-05
- ↑ Potosky A, Miller B, Albertsen P, Kramer B (1995). "The role of increasing detection in the rising incidence of prostate cancer". JAMA. 273 (7): 548&ndash, 52. doi:10.1001/jama.273.7.548. PMID 7530782.
- ↑ Gine Kolata (June 15, 2008). "New Take on a Prostate Drug, and a New Debate". NY Times. Retrieved 2008-06-15.
- ↑ Potosky A, Miller B, Albertsen P, Kramer B (2008). "Finasteride Does Not Increase the Risk of High-Grade Prostate Cancer: A Bias-Adjusted Modeling Approach". Cancer Prevention Research. Published Online First on May 18, 2008 as 10.1158/1940-6207.CAPR-08-0092: 174. doi:10.1158/1940-6207.CAPR-08-0092.
- ↑ Adams, J. The case of scirrhous of the prostate gland with corresponding affliction of the lymphatic glands in the lumbar region and in the pelvis. Lancet 1, 393 (1853).
- ↑ Lytton, B. Prostate cancer: a brief history and the discovery of hormonal ablation treatment. J. Urol. 165, 1859–1862
- ↑ Young, H. H. Four cases of radical prostatectomy. Johns Hopkins Bull. 16, 315 (1905).
- ↑ Walsh, P. C., Lepor, H. & Eggleston, J. C. Radical prostatectomy with preservation of sexual function: anatomical and pathological considerations. Prostate 4, 473-485 (1983). PMID 6889192
- ↑ Huggins, C. B. & Hodges, C. V. Studies on prostate cancer: 1. The effects of castration, of estrogen and androgen injection on serum phosphatases in metastatic carcinoma of the prostate. Cancer Res. 1, 203 (1941).
- ↑ Schally, A. V., Kastin, A. J. & Arimura, A. Hypothalamic FSH and LH-regulating hormone. Structure, physiology and clinical studies. Fertil. Steril. 22, 703–721 (1971).
- ↑ Tolis G, Ackman D, Stellos A, Mehta A, Labrie F, Fazekas AT, Comaru-Schally AM, Schally AV. Tumor growth inhibition in patients with prostatic carcinoma treated with luteinizing hormone-releasing hormone agonists. Proc Natl Acad Sci U S A. 1982 Mar;79(5):1658–62 PMID 6461861
- ↑ Denmeade SR, Isaacs JT. A History of Prostate Cancer Treatment. Nature Reviews Cancer 2, 389–396 (2002). PMID 12044015
- ↑ Scott, W. W. et al. Chemotherapy of advanced prostatic carcinoma with cyclophosphamide or 5-fluorouracil: results of first national randomized study. J. Urol. 114, 909–911 (1975). PMID 1104900
External links
Template:Urogenital neoplasia Template:SIB Template:Link FA Template:Link FA af:Prostaatkanker bn:প্রোস্টেট ক্যান্সার bg:Рак на простатата ca:Càncer de pròstata da:Prostatakræft de:Prostatakrebs dv:ޕްރޮސްޓޭޓް ކެންސަރު el:Καρκίνος του προστάτη fa:سرطان پروستات hr:Rak prostate id:Kanker prostat it:Carcinoma della prostata he:סרטן הערמונית la:Cancer prostatae lv:Prostatas vēzis nl:Prostaatkanker no:Prostatakreft simple:Prostate cancer fi:Eturauhassyöpä sv:Prostatacancer tl:Kanser sa prostata