Mitral stenosis resident survival guide: Difference between revisions
Rim Halaby (talk | contribs) |
|||
| (55 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div style="width: 80%;"> | |||
__NOTOC__ | __NOTOC__ | ||
{{CMG}}; {{AE}} {{TS}}; {{MM}}; {{AM}}; {{Rim}} | |||
{ | {| class="infobox" style="margin: 0 0 0 0; border: 0; float: right; width: 100px; background: #A8A8A8; position: fixed; top: 250px; right: 21px; border-radius: 0 0 10px 10px;" cellpadding="0" cellspacing="0"; | ||
|- | |||
! style="padding: 0 5px; font-size: 85%; background: #A8A8A8" align=center| {{fontcolor|#2B3B44|Mitral Stenosis Resident Survival Guide Microchapters}} | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Mitral stenosis resident survival guide#Overview|Overview]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Mitral stenosis resident survival guide#Causes|Causes]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Mitral stenosis resident survival guide#Stages|Stages]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Mitral stenosis resident survival guide#FIRE: Focused Initial Rapid Evaluation|FIRE]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Mitral stenosis resident survival guide#Complete Diagnostic Approach|Diagnosis]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Mitral stenosis resident survival guide#Treatment|Treatment]] | |||
: [[Mitral stenosis resident survival guide#Medical Therapy|Medical Therapy]] | |||
: [[Mitral stenosis resident survival guide#Intervention|Intervention]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Mitral stenosis resident survival guide#Secondary Prevention of Rheumatic Fever|Secondary Prevention of Rheumatic Fever]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Mitral stenosis resident survival guide#Do's|Do's]] | |||
|} | |||
==Overview== | ==Overview== | ||
[[Mitral stenosis]] refers to abnormal narrowing of mitral orifice, which leads to obstruction of blood flow from [[left atrium]] to [[left ventricle]]. The most common presentations of [[mitral stenosis]] are [[dyspnea]], [[orthopnea]], [[paroxysmal nocturnal dyspnea]], and [[peripheral edema]]. [[Mitral stenosis]] has a characteristic low-pitched, rumbling diastolic murmur, heard best at the apex during physical examination. The definitive therapy for [[mitral stenosis]] include [[Aortic stenosis valvuloplasty|percutaneous balloon valvotomy]], surgical [[mitral valve repair]], or [[mitral valve replacement]]. | [[Mitral stenosis]] refers to abnormal narrowing of mitral orifice, which leads to obstruction of blood flow from [[left atrium]] to [[left ventricle]] most commonly as a complication of [[rheumatic fever]]. The most common presentations of [[mitral stenosis]] are [[dyspnea]], [[orthopnea]], [[paroxysmal nocturnal dyspnea]], and [[peripheral edema]]. [[Mitral stenosis]] has a characteristic low-pitched, rumbling diastolic murmur, heard best at the apex during physical examination. The definitive therapy for [[mitral stenosis]] include [[Aortic stenosis valvuloplasty|percutaneous balloon valvotomy]], surgical [[mitral valve repair]], or [[mitral valve replacement]]. | ||
==Causes== | ==Causes== | ||
| Line 17: | Line 38: | ||
*[[Mitral annular calcification]] | *[[Mitral annular calcification]] | ||
*[[Rheumatic fever]]<ref name="Tadele-2013">{{Cite journal | last1 = Tadele | first1 = H. | last2 = Mekonnen | first2 = W. | last3 = Tefera | first3 = E. | title = Rheumatic mitral stenosis in Children: more accelerated course in sub-Saharan Patients. | journal = BMC Cardiovasc Disord | volume = 13 | issue = 1 | pages = 95 | month = Nov | year = 2013 | doi = 10.1186/1471-2261-13-95 | PMID = 24180350 }}</ref> | *[[Rheumatic fever]]<ref name="Tadele-2013">{{Cite journal | last1 = Tadele | first1 = H. | last2 = Mekonnen | first2 = W. | last3 = Tefera | first3 = E. | title = Rheumatic mitral stenosis in Children: more accelerated course in sub-Saharan Patients. | journal = BMC Cardiovasc Disord | volume = 13 | issue = 1 | pages = 95 | month = Nov | year = 2013 | doi = 10.1186/1471-2261-13-95 | PMID = 24180350 }}</ref> | ||
== | |||
Shown below is | Click '''[[Mitral stenosis causes|here]]''' for the complete list of causes | ||
<span style="font-size:85%">'''Abbreviations:''' '''AF''': | |||
==Stages== | |||
Shown below is a table depicting the 4 stages of mitral stenosis, adapted from 2014 AHA/ACC guidelines for management of valvular heart diseases.<ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref> | |||
<span style="font-size:85%">'''Abbreviations:''' '''MS: ''' mitral stenosis; '''MVA: '''mitral valve area; '''PASP: ''' pulmonary artery systolic pressure</span> | |||
{|Class="wikitable" | |||
|- | |||
|style="background:#DCDCDC;"|'''Stage'''||style="background:#DCDCDC;"|'''Definition'''||style="background:#DCDCDC;"|'''Valve anatomy'''||style="background:#DCDCDC;"|'''Valve hemodynamics'''||style="background:#DCDCDC;"|'''Hemodynamic consequences'''||style="background:#DCDCDC;"|'''Symptoms''' | |||
|- | |||
|'''A'''||At risk of [[MS]]||❑ Mild diastolic doming of mitral valve leaflets||❑ Normal transmitral velocity||Absent||Absent | |||
|- | |||
|'''B'''||Progressive [[MS]]|| ❑ Rheumatic valve changes characterized by commissural fusion and diastolic doming of [[mitral valve]]<br>❑ MVA > 1.5 cm<sup>2</sup> (planimetered)||❑ Increased transmitral flow velocities<br>❑ MVA > 1.5 cm<sup>2</sup> <br>❑ Pressure half time during diastole < 150 ms||❑ Mild to moderate [[left atrial]] enlargement<br>❑ Normal pulmonary pressure at rest ||None | |||
|- | |||
|'''C'''||Asymptomatic severe [[MS]]||❑ Rheumatic valve changes characterized by commissural fusion and diastolic doming of [[mitral valve]]<br> ❑ MVA ≤ 1.5 cm<sup>2</sup><br>❑ MVA ≤ 1 cm<sup>2</sup> in very severe [[MS]]|| ❑ MVA ≤ 1.5 cm<sup>2</sup> (planimetered)<br>❑ MVA ≤ 1 cm<sup>2</sup> (planimetered) in very severe [[MS]]<br>❑ Diastolic pressure half time ≥ 150 ms<br> ❑ Diastolic pressure half time ≥ 220 ms with very severe [[MS]]||❑ Severe [[left atrial]] enlargement<br>❑ PASP > 30 mm Hg||Absent | |||
|- | |||
|'''D'''||Symptomatic severe [[MS]]||❑ Rheumatic valve changes characterized by commissural fusion and diastolic doming of [[mitral valve]]<br> ❑ MVA ≤ 1.5 cm<sup>2</sup> (planimetered)||❑ MVA ≤ 1.5 cm<sup>2</sup><br>❑ MVA ≤ 1 cm<sup>2</sup> in very severe [[MS]]<br>❑ Diastolic pressure half time ≥ 150 ms<br> ❑ Diastolic pressure half time ≥ 220 ms with very severe [[MS]]||❑ Severe left atrial enlargement<br>❑ PASP > 30 mm Hg||❑ [[Dyspnea]] on exertion<br>❑ Decreased exercise tolerance | |||
|} | |||
==FIRE: Focused Initial Rapid Evaluation== | |||
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention. | |||
<span style="font-size:85%">Boxes in the red color signify that an urgent management is needed.</span> | |||
{{Family tree/start}} | |||
{{familytree | | | | | | | A00 | | | | | | | | | A00=<div style="width:22em">'''Identify cardinal findings that increase the pretest probability of [[mitral stenosis]]'''</div><br><div style="width:22em; text-align:left">❑ [[Mid diastolic murmur]] | |||
:❑ Low-pitched diastolic rumble | |||
:❑ Associated with an opening snap | |||
:❑ Best heard at the cardiac apex | |||
:❑ Radiating to the [[axilla]] | |||
:❑ Increases with lying down, raising the legs and with exercise | |||
:❑ Decreases with [[valsalva maneuver]] and [[amyl nitrate]] <br> | |||
❑ Reduced [[pulse pressure]]</div> }} | |||
{{familytree | | | | | | | |!| | | | | | | | | | }} | |||
{{familytree | | | | | | | A01 | | | | | | | | | | A01= <div style="text-align: left; width: 18em; padding: 1em;">'''Does the patient have any of the following findings of decompensated [[mitral stenosis]] that require urgent management?'''<br> | |||
❑ [[Tachycardia]] <br> ❑ [[Hypotension]]<br> ❑ [[Dyspnea|Severe dyspnea]]<br> ❑ [[Loss of consciousness]]<br>❑ [[Chest pain]]<br>❑ Sudden [[weakness]] or [[paralysis]]</div>}} | |||
{{familytree | | | | |,|-|-|^|-|-|.| | | | |}} | |||
{{familytree |boxstyle= padding: 0; background: #FA8072; text-align: center;| | | | B01 | | | | | B02 | | | |B01={{fontcolor|#F8F8FF|'''Yes'''}}| B02=<div style="text-align: center; background: #FFFFFF; height: 25px; line-height: 25px;">'''No'''</div>}} | |||
{{familytree | | | | |!| | | | | |!| }} | |||
{{familytree |boxstyle= padding: 0; background: #FA8072; text-align: center;| | | | C01 | | | | | C02 | C01=<div style="padding: 5px; text-align: center; color: #F8F8FF;">What is the complication of [[mitral stenosis|<span style="color:white;">mitral stenosis</span>]] that is causing decompensation?</div>| C02=<div style="text-align: center; background: #FFFFFF; height: 77px; line-height: 30px; padding: 5px;">'''[[Mitral stenosis resident survival guide#Complete Diagnostic Approach|Continue with the complete diagnostic approach below]]'''</div> }} | |||
{{familytree | |,|-|-|+|-|-|-|-|v|-|-|.| | | |}} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| H01| |H02 | | H03 | | H04 | | | | | | | | | H01=<div style=" text-align: center; width:15em">'''[[Stroke|<span style="color:white;">Stroke</span>]]'''</div><br><div style=" text-align: left">❑ Suspect in case of: | |||
:❑ Sudden weakness or [[paralysis|<span style="color:white;">paralysis</span>]] - face, arm or leg<br> | |||
:❑ Speech or visual difficulties<br> | |||
:❑ [[Altered level of consciousness|<span style="color:white;">Altered level of consciousness</span>]] <br> | |||
:❑ Sudden severe [[headache|<span style="color:white;">headache</span>]]<br> </div>|H02=<div style=" text-align: center; width:15em">'''[[Atrial fibrillation|<span style="color:white;">Atrial fibrillation</span>]]'''</div><br><div style=" text-align: left"> ❑ Suspect in case of [[palpitations|<span style="color:white;">palpitations</span>]] <br> ❑ Order an [[ECG|<span style="color:white;">ECG</span>]] immediately looking for | |||
:❑ Irregularly irregular rhythm, and | |||
:❑ Absent [[P waves|<span style="color:white;">P waves</span>]] | |||
</div> |H03= <div style=" text-align: center; width: 15em">[[Pulmonary embolism|<span style="color:white;">'''Pulmonary embolism'''</span>]]</div> <br><div style=" text-align: left"> ❑ Suspect in case of: | |||
:❑ Acute onset of exertional [[dyspnea|<span style="color:white;">dyspnea</span>]] or [[dyspnea|<span style="color:white;">dyspnea</span>]] at rest<br> | |||
:❑ Pleuritic or substernal [[chest pain|<span style="color:white;">chest pain</span>]] <br> | |||
:❑ [[Hemoptysis|<span style="color:white;">Hemoptysis</span>]] <br> </div>|H04=<div style=" text-align: center; width:15em">[[Pulmonary hypertension|<span style="color:white;">'''Pulmonary hypertension'''</span>]] ± '''right sided [[heart failure|<span style="color:white;">heart failure</span>]]'''</div><br> <div style=" text-align: left"> ❑ Suspect in case of severe [[dyspnea|<span style="color:white;">dyspnea</span>]] <br>❑ Increased [[jugular venous pressure|<span style="color:white;">jugular venous pressure</span>]] immediately<br> | |||
❑ [[Hepatomegaly|<span style="color:white;">Hepatomegaly </span>]] ± pulsatile [[liver|<span style="color:white;">liver</span>]] | |||
</div>}} | |||
{{familytree | |!| | |!| | | | | |!| | |!| | | | }} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| J01| |J02 | | J03 | | J04 | | | | | | | | | J01= <div style=" background: #FA8072; text-align: left; width: 15em">[[Stroke resident survival guide#First Initial Rapid Evaluation of Suspected Stroke|<span style="color:white;"> '''Click here for stroke resident survival guide'''</span>]] </div>| J02= <div style=" background: #FA8072; text-align: left; width: 15em">[[Atrial fibrillation resident survival guide|<span style="color:white;">'''Click here for atrial fibrillation resident survival guide'''</span>]] </div> | J03=<div style=" background: #FA8072; text-align: left; width: 15em">[[Pulmonary embolism resident survival guide|<span style="color:white;">'''Click here for pulmonary embolism resident survival guide'''</span>]] </div>| J04= <div style=" background: #FA8072; text-align: left; width: 15em">[[Pulmonary hypertension resident survival guide|<span style="color:white;">'''Click here for Pulmonary hypertension resident survival guide'''</span>]], or<br>[[Acute heart failure resident survival guide|<span style="color:white;">'''Click here for Acute heart failure resident survival guide'''</span>]] </div>}} | |||
{{familytree | |L|~|~|A|~|~|V|~|~|A|~|~|J| | |}} | |||
{{familytree | | | | | | | |:| | | | | | | | |}} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | | | | G01 | | | | G01= <div style=" background: #FA8072; text-align: left; width: 20em"> {{fontcolor|#F8F8FF| ❑ Treat the complications of [[mitral stenosis|<span style="color:white;">mitral stenosis</span>]] that lead to decompensation <br> ❑ Order a [[TTE|<span style="color:white;">TTE</span>]] to evaluate the severity of the [[mitral stenosis|<span style="color:white;">mitral stenosis</span>]]}}</div>}} | |||
{{familytree | | | | | | | |!| | }} | |||
{{familytree | | | | | | | H01 | | | | | | | | | H01=<div style=" background: ; text-align: left; width: 20em"> '''When to consider intervention in [[mitral stenosis]] ?''' <br> | |||
❑ '''[[Mitral stenosis resident survival guide#Treatment|<span style="color:navy;">Continue with the treatment algorithm below</span>]]'''</div> }} | |||
{{Family tree/end}} | |||
==Complete Diagnostic Approach== | |||
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.<ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref>.<br> | |||
<span style="font-size:85%">'''Abbreviations:''' '''AF''': [[Atrial fibrillation]]; '''[[PMBV|PMBC]]''': Percutaneous mitral ballon commissurotomy; '''TR''': [[Tricuspid regurgitation]]; '''[[S1]]''': First heart sound; '''[[P2]]''': Pulmonary component of second heart sound; '''EKG''': [[Electrocardiogram]]; '''TTE''': [[Transthoracic echocardiography]]; '''MS''': [[Mitral stenosis]] </span> <br> | |||
{{familytree/start |summary=PE diagnosis Algorithm.}} | {{familytree/start |summary=PE diagnosis Algorithm.}} | ||
{{familytree | | A01 |A01=<div style="float: left; text-align: left; padding:1em;"> '''Characterize the symptoms:''' | {{familytree | | | | | A01 |A01=<div style="float: left; text-align: left; padding:1em;"> '''Characterize the symptoms:'''<br> | ||
❑ [[Exercise intolerance]]<br> | ❑ [[Exercise intolerance]]<br> | ||
❑ [[Dyspnea on exertion]]<br> | ❑ [[Dyspnea on exertion]]<br> | ||
| Line 33: | Line 118: | ||
❑ [[Hemoptysis]]<br> | ❑ [[Hemoptysis]]<br> | ||
❑ [[Thromboembolism]]<br> | ❑ [[Thromboembolism]]<br> | ||
:❑ [[Stroke]] | |||
:❑ [[Pulmonary embolism]] | |||
❑ [[Respiratory infections]]<br> | ❑ [[Respiratory infections]]<br> | ||
❑ [[Fatigue]]<br> | ❑ [[Fatigue]]<br> | ||
❑ [[Right heart failure | ❑ [[Right heart failure]]</div>}} | ||
: ❑ [[ | {{familytree | | | | | |!| | | | | | | | | | | | | | | | | | | | | | | | | }} | ||
{{Family tree| | | | | Y01 | | | | | | | | | | Y01=<div style="float: left; text-align: Left; width:25em ">'''Inquire about past medical history:''' <br>❑ [[Rheumatic fever]] <br> ❑ [[Respiratory infection]] <br> ❑ Congenital [[MS]] </div> }} | |||
{{family tree| | | | | |!| | | | | | | | | | | }} | |||
{{ | |||
{{familytree | | B01 | | | | | | | | | | | | | | | | | | | | | | | |B01=<div style="float: left; text-align: left; padding:1em;">'''Examine the patient:'''<br> | {{familytree | | | | | B01 | | | | | | | | | | | | | | | | | | | | | | | |B01=<div style="float: left; text-align: left; padding:1em;">'''Examine the patient:'''<br> | ||
'''Appearance of the patient'''<br> | '''Appearance of the patient'''<br> | ||
| Line 52: | Line 139: | ||
:❑ Rhythm<br> | :❑ Rhythm<br> | ||
::❑ [[Irregularly irregular pulse|Irregularly irregular]] ( | ::❑ [[Irregularly irregular pulse|Irregularly irregular]] (suggestive of [[AF]])<br> | ||
:❑ Strength | :❑ Strength | ||
| Line 60: | Line 147: | ||
'''Neck''':<br> | '''Neck''':<br> | ||
❑ [[Jugular venous distension]]<br> | ❑ [[Jugular venous distension]]<br> | ||
: ❑ Prominent [[a wave]] | : ❑ Prominent [[a wave]] (suggestive of [[right heart failure]])<br> | ||
: ❑ Absent [[a wave]] | : ❑ Absent [[a wave]] (suggestive of [[AF]])<br> | ||
: ❑ Prominent [[v wave]] | : ❑ Prominent [[v wave]] (suggestive of [[TR]])<br> | ||
'''Extremities''': <br> | |||
❑ [[Peripheral edema]] (suggestive of right sided [[heart failure]])<br> | |||
'''Abdominal examination''': <br> | |||
❑ [[Ascites]] (suggestive of right sided [[heart failure]])<br> | |||
❑ [[Hepatomegaly]] (suggestive of right sided [[heart failure]])<br> | |||
''' | '''Cardiovascular examination''':<br> | ||
'''Auscultation''' | '''Auscultation''' | ||
| Line 72: | Line 166: | ||
❑ Opening snap<br> | ❑ Opening snap<br> | ||
❑ [[Murmur]]<br> | ❑ [[Murmur]]<br> | ||
: ❑ Most prominent at the apex and best heard using the bell of the stethoscope <br> | |||
: ❑ [[Mid diastolic murmur]] (low pitched, rumbling)<br> | : ❑ [[Mid diastolic murmur]] (low pitched, rumbling)<br> | ||
: ❑ [[Holosystolic murmur]] | : ❑ [[Holosystolic murmur]] (suggestive of [[TR]])<br> | ||
: ❑ [[Graham-Steell murmur]] | : ❑ [[Graham-Steell murmur]] (suggestive of [[pulmonary regurgitation]])<br> | ||
{{#ev:youtube|HW2pk1icYdM|250}}<br> | {{#ev:youtube|HW2pk1icYdM|250}}<br> | ||
<SMALL>''Video adapted from Youtube.com''</SMALL><br> | <SMALL>''Video adapted from Youtube.com''</SMALL><br> | ||
❑ [[Rales]]</div>}} | ❑ [[Rales]]</div>}} | ||
{{familytree | | |!| | | | | | | | | | | | | | | | | | | | | | | | | }} | {{familytree | | | | | |!| | | | | | | | | | | | | | | | | | | | | | | | | }} | ||
{{familytree | | C01 | | | | | | | | | | | | | | | | | | | | | | | |C01=<div style="float: left; text-align: left; padding:1em;">'''Order tests:''' | {{familytree | | | | | C01 | | | | | | | | | | | | | | | | | | | | | | | |C01=<div style="float: left; text-align: left; padding:1em;">'''Order tests:''' <br> | ||
❑ [[Transthoracic echocardiography]] <br> | |||
:❑ Assess valve area<br> | |||
:❑ Assess disease of other valves <br> | |||
:❑ Assess mean [[pressure gradient]]<br> | |||
:❑ Assess [[pulmonary artery]] pressure<br> | |||
:❑ Assess suitability of valve morphology for [[PMBV|PMBC]]<br> | |||
❑ Exercise testing with [[Doppler]] or invasive hemodynamic assessment in case of discrepancy between resting Doppler echocardiographic findings and clinical symptoms or signs | |||
:❑ Assess the response of the mean mitral gradient | |||
:❑ Assess the pulmonary artery pressure | |||
❑ | ❑ [[EKG]]<br> | ||
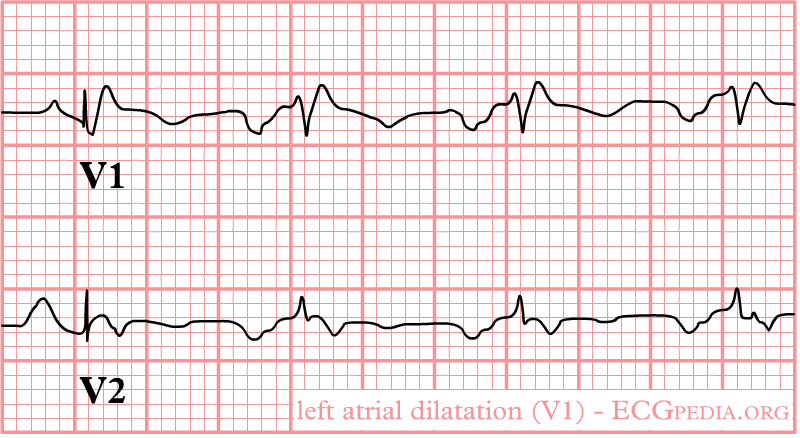
:❑ [[Left atrial enlargement electrocardiogram|Left atrial enlargement]]<br> | :❑ [[Left atrial enlargement electrocardiogram|Left atrial enlargement]]<br> | ||
::❑ Broad, bifid P wave in lead II (P mitrale)<br> | ::❑ Broad, bifid [[P wave]] in lead II (P mitrale)<br> | ||
[[Image:P mitrale.gif|200px]]<br> | [[Image:P mitrale.gif|200px]]<br> | ||
<SMALL>''Picture adapted from en.ecgpedia.org''</SMALL><br> | <SMALL>''Picture adapted from en.ecgpedia.org''</SMALL><br> | ||
::❑ Biphasic P wave with terminal negative portion<br> | ::❑ Biphasic [[P wave]] with terminal negative portion<br> | ||
[[Image:LAE-v1.png|Left atrial enlargement as seen in lead V1|200px]]<br> | [[Image:LAE-v1.png|Left atrial enlargement as seen in lead V1|200px]]<br> | ||
<SMALL>''Picture adapted from en.ecgpedia.org''</SMALL><br> | <SMALL>''Picture adapted from en.ecgpedia.org''</SMALL><br> | ||
| Line 93: | Line 197: | ||
::❑ [[Right axis deviation]] of +90 degrees or more | ::❑ [[Right axis deviation]] of +90 degrees or more | ||
::❑ Incomplete [[RBBB]] pattern | ::❑ Incomplete [[RBBB]] pattern | ||
::❑ ST T strain pattern in leads 2,3,aVF | ::❑ ST T strain pattern in leads 2,3,aVF | ||
::❑ [[P pulmonale]] or [[right atrial enlargement]] or P congenitale | ::❑ [[P pulmonale]] or [[right atrial enlargement]] or P congenitale | ||
::❑ Inverted [[T wave]] in the anterior precordial leads <br> | |||
::❑ Inverted [[T wave]] in the anterior precordial leads | ''Click [[Electrocardiographic findings in right ventricular hypertrophy|here]] for the rest of the EKG findings in right ventricular hypertrophy'' | ||
:❑ [[Right axis deviation]]<br> | :❑ [[Right axis deviation]]<br> | ||
::❑ [[QRS complex]] is positive in leads III and aVF<br> | ::❑ [[QRS complex]] is positive in leads III and aVF<br> | ||
::❑ [[QRS complex]] is negative in leads I and aVL<br> | ::❑ [[QRS complex]] is negative in leads I and aVL<br> | ||
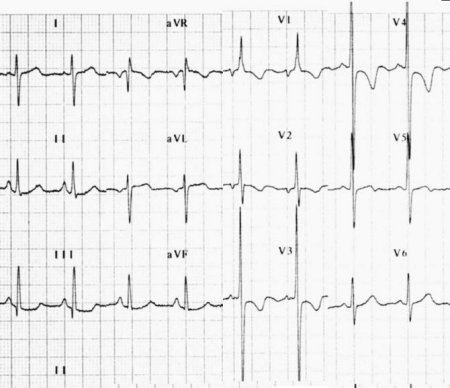
''Shown below an [[ECG]] depicting [[right axis deviation]]'' <br> | |||
[[File:De-Rightaxis.jpg|200px]]<br> | [[File:De-Rightaxis.jpg|200px]]<br> | ||
:❑ [[Atrial fibrillation]]<br> | :❑ [[Atrial fibrillation]]<br> | ||
::❑ Absence of [[P waves]]<br> | ::❑ Absence of [[P waves]]<br> | ||
::❑ Irregularly irregular [[heart rate]]<br> | ::❑ Irregularly irregular [[heart rate]]<br> | ||
''Shown below an [[ECG]] depicting [[atrial fibrillation]]'' <br> | |||
[[Image:AFIB_06.jpg|200px]]<br> | [[Image:AFIB_06.jpg|200px]]<br> | ||
<SMALL>''Picture adapted from Wikidoc.org''</SMALL><br> | <SMALL>''Picture adapted from Wikidoc.org''</SMALL><br> | ||
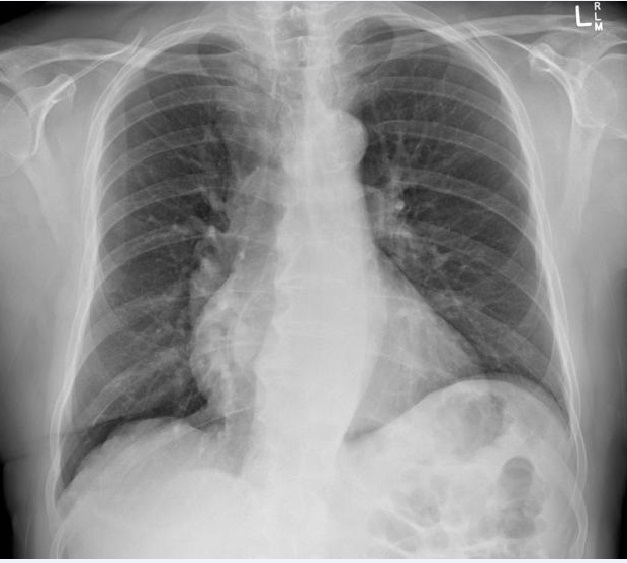
❑ | ❑ [[Chest X-ray]]<br> | ||
:❑ Double right heart border (suggestive of [[left atrial hypertrophy]]) | :❑ Double right heart border (suggestive of [[left atrial hypertrophy]]) | ||
:❑ Prominent pulmonary artery | :❑ Prominent [[pulmonary artery]] | ||
:❑ [[Kerley lines]] (suggestive of interstitial [[pulmonary edema]]) | :❑ [[Kerley lines]] (suggestive of interstitial [[pulmonary edema]]) | ||
[[File:M.S chest X-ray.jpg|200px]]<br> | [[File:M.S chest X-ray.jpg|200px]]<br> | ||
<SMALL>''Picture adapted from Radiopedia.org''</SMALL><br> | <SMALL>''Picture adapted from Radiopedia.org''</SMALL><br> | ||
</div>}} | </div>}} | ||
{{familytree | | |!| | | | | | | | | | | | | | | | | | | | | | | | | }} | {{familytree | | | | | |!| | | | | | | | | | | | | | | | | | | | | | | | | }} | ||
{{ | {{Family tree | | | | | Z01 | | | | | | | | | | Z01=<div style="float: left; text-align: left; width:25em "> '''Classify [[mitral stenosis]] based on the following findings on [[TTE]]:'''<br> ❑ Valve anatomy <br> ❑ Valve hemodynamics gradient <br> ❑ Hemodynamic consequences</div>}} | ||
{{Family tree | |,|-|-|-|+|-|-|v|-|-|-|.| | | | | |}} | |||
{{Family tree |C01 | | C02 | |C03 | | C04| | | | |C01=<div style="float: left; text-align: center; width:15em">'''[[Mitral stenosis resident survival guide#Classification|Stage A]]'''</div>|C02=<div style="float: left; text-align: center; width:25em">'''[[Mitral stenosis resident survival guide#Classification|Stage B]]'''</div>|C03=<div style="float: left; text-align: center; width:15em">'''[[Mitral stenosis resident survival guide#Classification|Stage C]]'''</div>|C04=<div style="float: left; text-align: center; width:15em">'''[[Mitral stenosis resident survival guide#Classification|Stage D]]'''</div>}} | |||
:❑ | |||
</div>}} | |||
{{ | |||
{{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | {{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | ||
{{familytree/end}} | {{familytree/end}} | ||
==Treatment== | ==Treatment== | ||
===Medical Therapy=== | |||
{{ | {{Family tree/start}} | ||
{{ | {{Family tree | A01 | | A01=<div style="float: left; text-align: left; padding:1em;"> | ||
'''Treatment of Acute Decompensation'''<br> | |||
: ❑ | ❑ Digoxin <br> | ||
: ❑ [[ | In the following cases:<br> | ||
❑ | :❑ Symptomatic [[right ventricular]] or [[left ventricular]] dysfunction ([[digitalis]] increases [[myocardial]] contractility) | ||
: ❑ [[ | :❑ [[Atrial fibrillation]] ([[digitalis]] slows the ventricular response which prolongs the diastolic filling time)<ref name="pmid11907022">{{cite journal| author=Boon NA, Bloomfield P| title=The medical management of valvar heart disease. | journal=Heart | year= 2002 | volume= 87 | issue= 4 | pages= 395-400 | pmid=11907022 | doi= | pmc=PMC1767079 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11907022 }} </ref> | ||
: ❑ | ❑ Diuretics (In the following cases fluid overload)<br> | ||
❑ Low sodium diet <br> | |||
{{ | ❑ Activity restriction <br> | ||
'''Systemic Embolization Prevention'''<ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref> <br> | |||
In the following cases:<br> | |||
❑ Paroxysmal, persistent, or permanent [[atrial fibrillation]] ([[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I, Level of Evidence B]]) <br> | |||
❑ Prior [[embolization]] event ([[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I, Level of Evidence B]]) <br> | |||
❑ [[Left atrial]] thrombus ([[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I, Level of Evidence B]]) <br> | |||
'''Rate Control'''<ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref><br> | |||
In the following cases:<br> | |||
❑ [[Atrial fibrillation]] associated with fast ventricular response ([[ACC AHA guidelines classification scheme#Classification of Recommendations|Class IIa, Level of Evidence C]]) | |||
❑ Normal [[sinus rhythm]] plus symptoms associated with exercise ([[ACC AHA guidelines classification scheme#Classification of Recommendations|Class IIb, Level of Evidence B]]) </div>}} | |||
{{Family tree/end}} | |||
===Intervention=== | |||
Shown below is an algorithm depicting the indications for mitral stenosis intervention according to the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease.<ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref> | |||
<span style="font-size:85%">'''Abbreviations:''' '''AF''': [[atrial fibrillation]]; '''MR:''' [[mitral regurgitation]]; '''MS:''' [[mitral stenosis]]; '''MVA:''' mitral valve area ; '''PCWP:''' [[pulmonary capillary wedge pressure]]; '''PMBC:''' [[percutaneous mitral balloon commissurotomy]]; '''T<sub>1/2</sub>:''' pressure half-time</span> | |||
{{Familytree/start}} | |||
{{Family tree | | | | | | | | | | | | | | | | | | A01 | | | | | | | | | | | | | | | | A01= <div style="float: left; text-align: left; width: 8em; padding:1em;">'''Determine the severity of rheumatic [[mitral stenosis]] (MS)'''</div>}} | |||
{{Family tree | | | | | | | | |,|-|-|-|-|-|-|-|-|-|+|-|-|-|-|-|-|-|-|-|-|-|-|.| | | | }} | |||
{{Family tree | | | | | | | | B01 | | | | | | | | B02 | | | | | | | | | | | B03 | | | B01= <div style="float: left; text-align: left; width: 8em; padding:1em;">'''Very severe MS''' <br> ❑ MVA ≤1 cm2 <br> ❑ T<sub>1/2</sub> ≥220 ms </div>| B02= <div style="float: left; text-align: left; width: 8em; padding:1em;">'''Severe MS''' <br> ❑ MVA ≤1.5 cm2 <br> ❑ T<sub>1/2</sub> ≥150 ms </div>| B03= <div style="float: left; text-align: left; width: 8em; padding:1em;">'''Progressive MS''' <br> MVA >1.5 cm2 <br> T<sub>1/2</sub> <150 ms </div>}} | |||
{{Family tree | | | | | | | | |!| | | | | | | | | |!| | | | | | | | | | | | |!| | }} | |||
{{Family tree | | | | | | | | B04 | | | | | | | | B05 | | | | | | | | | | | B06 | B04= <div style="float: left; text-align: left; width: 8em; padding:1em;">Is the patient symptomatic? </div>| B05= <div style="float: left; text-align: left; width: 8em; padding:1em;">Is the patient symptomatic?</div>| B06=<div style="float: left; text-align: left; width: 8em; padding:1em;">Is the patient symptomatic? </div>}} | |||
{{Family tree | | | |,|-|-|-|-|^|-|-|.| |,|-|-|-|-|^|-|-|-|-|-|-|.| | | | | |!| | | | }} | |||
{{Family tree | | | C01 | | | | | | | C02 | | | | | | | | | | | C03 | | | | C04 | | | C01= No <br> ([[Mitral stenosis resident survival guide#Classification| Stage C]])| C02= Yes <br> ([[Mitral stenosis resident survival guide#Classification|Stage D]])| C03= No <br> ([[Mitral stenosis resident survival guide#Classification|Stage C]])| C04= <div style="float: left; text-align: left; width: 8em; padding:1em;">Yes <br> With no other cause for the symptoms </div>}} | |||
{{Family tree | | | |!| | | | | | | | |!| | | | | | | | | | | | |!| | | | | |!| | | | }} | |||
{{Family tree | | | D01 | | | | | | | D02 | | | | | | | | | | | |!| | | | | |!| | | | D01= <div style="float: left; text-align: left; width: 8em; padding:1em;">Does the patient have: <br> ❑ Favorable valve morphology <br> ''AND'' <br>❑ No [[left atrial]] clot <br> ''AND'' <br>❑ No or mild [[MR]] </div>| D02= <div style="float: left; text-align: left; width: 8em; padding:1em;">Does the patient have: <br> ❑ Favorable valve morphology <br> ''AND'' <br>❑ No [[left atrial]] clot <br> ''AND'' <br> ❑ No or mild [[MR]] </div>}} | |||
{{Family tree | | | |!| | | | | | | | |!| | | | | | | | | | | | |!| | | | | |!| | | | }} | |||
{{Family tree | | | |!| | | | | | | | |!| | | | | | | | | | | | D03 | | | | D04 | | | | D03= <div style="float: left; text-align: left; width: 8em; padding:1em;">Is there a new onset of [[AF]]? </div>| D04= <div style="float: left; text-align: left; width: 8em; padding:1em;">Order an exercise treadmill test </div>}} | |||
{{Family tree | |,|-|^|-|.| | | |,|-|-|^|-|-|.| | | | | | | |,|-|^|-|.| | | |!| | | | }} | |||
{{Family tree | E01 | | E02 | | E03 | | | | E04 | | | | | | E05 | | E06 | | E07 | | | E01= No| E02= Yes| E03= Yes| E04= No| E05= Yes| E06= No| E07= Is [[PCWP]]> 25 mm Hg?}} | |||
{{Family tree | |!| | | |!| | | |!| | | | | |!| | | | | | | |!| | | |!| |,|-|^|-|.| | }} | |||
{{Family tree | |!| | | |!| | | |!| | | | | F01 | | | | | | F02 | | |!| |!| | | |!| F01= <div style="float: left; text-align: left; width: 8em; padding:1em;">Does the patient have: <br> ❑ [[NYHA class]] III-IV symptoms <br> ''AND'' <br> ❑ High surgical risk </div>| F02= <div style="float: left; text-align: left; width: 8em; padding:1em;">Does the patient have: <br> ❑ Favorable valve morphology <br> ''AND'' <br>❑ No [[left atrial]] clot <br> ''AND'' <br>❑ No or mild [[MR]] </div>}} | |||
{{Family tree | |!| | | |!| | | |!| | | |,|-|^|-|.| | | |,|-|^|-|.| |!| |!| | | |!| | }} | |||
{{Family tree | |!| | | |!| | | |!| | | G01 | | G02 | | G03 | | G04 |!| G05 | | G06 | | G01= No| G02= Yes| G03= Yes| G04= No| G05= Yes| G06= No}} | |||
{{Family tree | |!| | | |!| | | |!| | | |!| | | | |!| |!| | | | |!| |!| |!| | | |!| | }} | |||
{{Family tree | H01 | | H02 | | H03 | | H04 | | | | H05 | | | | | H06 | | H07 | | H08 | H01= Periodic monitoring| H02= [[PMBC]] (Class IIa)| H03= [[PMBC]] (Class I)| H04= Mitral valve surgery (Class I)| H05= [[PMBC]] (Class IIb)| H06= Periodic monitoring| H07= [[PMBC]] (Class IIb)| H08= Periodic monitoring}} | |||
{{Familytree/end}} | |||
Shown below is | ==Secondary Prevention of Rheumatic Fever== | ||
===Indications=== | |||
Shown below is the table depicting the indication for secondary prophylaxis of [[rheumatic fever]].<ref name="pmid19246689">{{cite journal| author=Gerber MA, Baltimore RS, Eaton CB, Gewitz M, Rowley AH, Shulman ST et al.| title=Prevention of rheumatic fever and diagnosis and treatment of acute Streptococcal pharyngitis: a scientific statement from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young, the Interdisciplinary Council on Functional Genomics and Translational Biology, and the Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics. | journal=Circulation | year= 2009 | volume= 119 | issue= 11 | pages= 1541-51 | pmid=19246689 | doi=10.1161/CIRCULATIONAHA.109.191959 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19246689 }} </ref> | |||
{| style="cellpadding=0; cellspacing= 0; width: 600px;" | |||
{| style=" | |||
|- | |- | ||
| style="font-size: | | style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF;" align=center | '''Indications'''|| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF;" align=center | '''Duration of prophylaxis''' | ||
|- | |- | ||
| style="font-size: | |style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left | ▸ '''''[[Rheumatic fever]] with [[carditis]] and persistent [[valvular heart disease]] || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left |▸ '''''10 years or until the patient is 40 years (whichever is longer)''''' ([[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I, Level of Evidence C]]) | ||
|- | |- | ||
|style="font-size: | |style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left | ▸ '''''[[Rheumatic fever]] with [[carditis]] but no [[valvular heart disease]] || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left |▸ '''''10 years or until the patient is 21 years (whichever is longer)''''' ([[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I, Level of Evidence C]]) | ||
|- | |- | ||
|style="font-size: | |style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left | ▸ '''''[[Rheumatic fever]] without [[carditis]] || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left |▸ '''''5 years or until the patient is 21 years (whichever is longer)''''' ([[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I, Level of Evidence C]]) | ||
|- | |- | ||
|} | |} | ||
|} | |||
< | ===Antibiotic Regimens=== | ||
Shown below is the table depicting the antibiotic regimens for secondary prophylaxis of [[rheumatic fever]].<ref name="pmid19246689">{{cite journal| author=Gerber MA, Baltimore RS, Eaton CB, Gewitz M, Rowley AH, Shulman ST et al.| title=Prevention of rheumatic fever and diagnosis and treatment of acute Streptococcal pharyngitis: a scientific statement from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young, the Interdisciplinary Council on Functional Genomics and Translational Biology, and the Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics. | journal=Circulation | year= 2009 | volume= 119 | issue= 11 | pages= 1541-51 | pmid=19246689 | doi=10.1161/CIRCULATIONAHA.109.191959 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19246689 }} </ref> | |||
{| style="cellpadding=0; cellspacing= 0; width: 600px;" | {| style="cellpadding=0; cellspacing= 0; width: 600px;" | ||
|- | |- | ||
| style="padding: 0 5px; font-size: 100%; background: # | | style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF;" align=center | '''Antibiotics'''|| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF;" align=center | '''Dosage''' | ||
|- | |||
|- | |||
| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left | '''''[[Penicillin G benzathine]]''''' <br> ([[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I, Level of Evidence A]])||style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left| ▸ '''''Weight >27 Kg (60 lb): 1.2 million units IM every day for 4 weeks'''''<br>▸ '''''Weight ≤27 Kg (60 lb): 600,000 units IM every day for 4 weeks''''' | |||
|- | |- | ||
| style="font-size: | |style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left |'''''[[Penicillin V]]''''' <br> ([[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I, Level of Evidence B]])|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left |▸ '''''200 mg orally twice a day''''' | ||
|- | |- | ||
|style="font-size: | |style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left|'''''[[Sulfadiazine]]''''' <br> ([[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I, Level of Evidence B]])|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left|▸ '''''Weight >27 Kg (60 lb): 1 g orally once a day''''' <br> ▸ '''''Weight ≤27 Kg (60 lb): o.5 g orally once a day''''' | ||
|- | |- | ||
|style="font-size: | |style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left|'''''[[Macrolide]] or [[azalide]] antibiotics (in patients allergic to [[penicillin]])''''' <br> ([[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I, Level of Evidence C]])|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left|▸ '''''Varies''''' | ||
|- | |- | ||
|} | |} | ||
==Do's== | ==Do's== | ||
* Perform [[transesophageal echocardiography]] (TEE) in patients considered for [[PMBV|PMBC]] to rule out left atrial thrombus and to determine [[mitral regurgitation]] severity. | * Perform [[transesophageal echocardiography]] ([[TEE]]) in patients considered for [[PMBV|PMBC]] to rule out left atrial [[thrombus]] and to determine [[mitral regurgitation]] severity. | ||
* Perform [[exercise testing]] or invasive hemodynamic testing, when clinical signs and symptoms don't co-relate with echocardiographic findings. | * Perform [[exercise testing]] or invasive hemodynamic testing, when clinical signs and symptoms don't co-relate with [[echocardiographic]] findings. | ||
* Perform [[mitral valve surgery]] in [[Mitral stenosis stages|stage C]] and [[Mitral stenosis stages|stage D]] mitral stenosis, if patient is undergoing cardiac surgery for some other indication. | * Perform [[mitral valve surgery]] in [[Mitral stenosis stages|stage C]] and [[Mitral stenosis stages|stage D]] [[mitral stenosis]], if patient is undergoing cardiac surgery for some other indication. | ||
* Perform [[mitral valve surgery]] in moderate mitral stenosis (mitral valve area: 1.6 - 2 cm<sup>2</sup>) if the patient is undergoing cardiac surgery for other indications. | * Perform [[mitral valve surgery]] in moderate [[mitral stenosis]] (mitral valve area: 1.6 - 2 cm<sup>2</sup>) if the patient is undergoing cardiac surgery for other indications. | ||
* Perform [[mitral valve surgery]] with excision of left atrial appendage in [[Mitral stenosis stages|stage C]] and [[Mitral stenosis stages|stage D]] mitral stenosis patients who have had recurrent embolic events despite being on [[anticoagulation therapy]]. | * Perform [[mitral valve surgery]] with excision of left atrial appendage in [[Mitral stenosis stages|stage C]] and [[Mitral stenosis stages|stage D]] [[mitral stenosis]] patients who have had recurrent embolic events despite being on [[anticoagulation therapy]]. | ||
* Perform [[TTE]] every 3-5 years in asymptomatic [[Mitral stenosis stages|stage B]] [[MS]] patients and every 1-2 years in asymptomatic [[Mitral stenosis stages|stage C]] [[MS]] patients who have mitral valve area 1-1.5 cm<sup>2</sup> . | * Perform [[TTE]] every 3-5 years in asymptomatic [[Mitral stenosis stages|stage B]] [[MS]] patients and every 1-2 years in asymptomatic [[Mitral stenosis stages|stage C]] [[MS]] patients who have mitral valve area 1-1.5 cm<sup>2</sup> . | ||
* Perform [[TTE]] once every year in asymptomatic [[Mitral stenosis stages|stage C]] [[MS]] patients who have mitral valve area < 1 cm<sup>2</sup>. | * Perform [[TTE]] once every year in asymptomatic [[Mitral stenosis stages|stage C]] [[MS]] patients who have mitral valve area < 1 cm<sup>2</sup>. | ||
* In cases of senile calcific mitral stenosis, intervention is done only when symptoms are severe and cannot be controlled with [[Atrial fibrillation resident survival guide#Heart rate control|heart rate control]] and [[diuretics]]. | * In cases of senile calcific [[mitral stenosis]], intervention is done only when symptoms are severe and cannot be controlled with [[Atrial fibrillation resident survival guide#Heart rate control|heart rate control]] and [[diuretics]]. | ||
==References== | ==References== | ||
| Line 229: | Line 338: | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
</div> | |||
Latest revision as of 22:36, 22 July 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Twinkle Singh, M.B.B.S. [2]; Mohamed Moubarak, M.D. [3]; Amr Marawan, M.D. [4]; Rim Halaby, M.D. [5]
| Mitral Stenosis Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| Stages |
| FIRE |
| Diagnosis |
| Treatment |
| Secondary Prevention of Rheumatic Fever |
| Do's |
Overview
Mitral stenosis refers to abnormal narrowing of mitral orifice, which leads to obstruction of blood flow from left atrium to left ventricle most commonly as a complication of rheumatic fever. The most common presentations of mitral stenosis are dyspnea, orthopnea, paroxysmal nocturnal dyspnea, and peripheral edema. Mitral stenosis has a characteristic low-pitched, rumbling diastolic murmur, heard best at the apex during physical examination. The definitive therapy for mitral stenosis include percutaneous balloon valvotomy, surgical mitral valve repair, or mitral valve replacement.
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
Click here for the complete list of causes
Stages
Shown below is a table depicting the 4 stages of mitral stenosis, adapted from 2014 AHA/ACC guidelines for management of valvular heart diseases.[2]
Abbreviations: MS: mitral stenosis; MVA: mitral valve area; PASP: pulmonary artery systolic pressure
| Stage | Definition | Valve anatomy | Valve hemodynamics | Hemodynamic consequences | Symptoms |
| A | At risk of MS | ❑ Mild diastolic doming of mitral valve leaflets | ❑ Normal transmitral velocity | Absent | Absent |
| B | Progressive MS | ❑ Rheumatic valve changes characterized by commissural fusion and diastolic doming of mitral valve ❑ MVA > 1.5 cm2 (planimetered) |
❑ Increased transmitral flow velocities ❑ MVA > 1.5 cm2 ❑ Pressure half time during diastole < 150 ms |
❑ Mild to moderate left atrial enlargement ❑ Normal pulmonary pressure at rest |
None |
| C | Asymptomatic severe MS | ❑ Rheumatic valve changes characterized by commissural fusion and diastolic doming of mitral valve ❑ MVA ≤ 1.5 cm2 ❑ MVA ≤ 1 cm2 in very severe MS |
❑ MVA ≤ 1.5 cm2 (planimetered) ❑ MVA ≤ 1 cm2 (planimetered) in very severe MS ❑ Diastolic pressure half time ≥ 150 ms ❑ Diastolic pressure half time ≥ 220 ms with very severe MS |
❑ Severe left atrial enlargement ❑ PASP > 30 mm Hg |
Absent |
| D | Symptomatic severe MS | ❑ Rheumatic valve changes characterized by commissural fusion and diastolic doming of mitral valve ❑ MVA ≤ 1.5 cm2 (planimetered) |
❑ MVA ≤ 1.5 cm2 ❑ MVA ≤ 1 cm2 in very severe MS ❑ Diastolic pressure half time ≥ 150 ms ❑ Diastolic pressure half time ≥ 220 ms with very severe MS |
❑ Severe left atrial enlargement ❑ PASP > 30 mm Hg |
❑ Dyspnea on exertion ❑ Decreased exercise tolerance |
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.
Boxes in the red color signify that an urgent management is needed.
Identify cardinal findings that increase the pretest probability of mitral stenosis ❑ Mid diastolic murmur
| |||||||||||||||||||||||||||||||||||||||||||||
Does the patient have any of the following findings of decompensated mitral stenosis that require urgent management? ❑ Tachycardia ❑ Hypotension ❑ Severe dyspnea ❑ Loss of consciousness ❑ Chest pain ❑ Sudden weakness or paralysis | |||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||
What is the complication of mitral stenosis that is causing decompensation? | |||||||||||||||||||||||||||||||||||||||||||||
❑ Suspect in case of:
| ❑ Suspect in case of palpitations ❑ Order an ECG immediately looking for | ❑ Suspect in case of:
| Pulmonary hypertension ± right sided heart failure ❑ Suspect in case of severe dyspnea ❑ Increased jugular venous pressure immediately ❑ Hepatomegaly ± pulsatile liver | ||||||||||||||||||||||||||||||||||||||||||
❑ Treat the complications of mitral stenosis that lead to decompensation ❑ Order a TTE to evaluate the severity of the mitral stenosis | |||||||||||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.[2].
Abbreviations: AF: Atrial fibrillation; PMBC: Percutaneous mitral ballon commissurotomy; TR: Tricuspid regurgitation; S1: First heart sound; P2: Pulmonary component of second heart sound; EKG: Electrocardiogram; TTE: Transthoracic echocardiography; MS: Mitral stenosis
Characterize the symptoms: ❑ Exercise intolerance ❑ Respiratory infections | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Examine the patient: Appearance of the patient Vital signs ❑ Pulse
Neck:
Extremities: Abdominal examination: Cardiovascular examination: Auscultation
{{#ev:youtube|HW2pk1icYdM|250}} | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Order tests: ❑ Transthoracic echocardiography
❑ Exercise testing with Doppler or invasive hemodynamic assessment in case of discrepancy between resting Doppler echocardiographic findings and clinical symptoms or signs
❑ EKG
Click here for the rest of the EKG findings in right ventricular hypertrophy
Shown below an ECG depicting right axis deviation
Shown below an ECG depicting atrial fibrillation
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Classify mitral stenosis based on the following findings on TTE: ❑ Valve anatomy ❑ Valve hemodynamics gradient ❑ Hemodynamic consequences | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment
Medical Therapy
Treatment of Acute Decompensation
❑ Diuretics (In the following cases fluid overload)
| |||||||
Intervention
Shown below is an algorithm depicting the indications for mitral stenosis intervention according to the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease.[2]
Abbreviations: AF: atrial fibrillation; MR: mitral regurgitation; MS: mitral stenosis; MVA: mitral valve area ; PCWP: pulmonary capillary wedge pressure; PMBC: percutaneous mitral balloon commissurotomy; T1/2: pressure half-time
Determine the severity of rheumatic mitral stenosis (MS) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Very severe MS ❑ MVA ≤1 cm2 ❑ T1/2 ≥220 ms | Severe MS ❑ MVA ≤1.5 cm2 ❑ T1/2 ≥150 ms | Progressive MS MVA >1.5 cm2 T1/2 <150 ms | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Is the patient symptomatic? | Is the patient symptomatic? | Is the patient symptomatic? | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No ( Stage C) | Yes (Stage D) | No (Stage C) | Yes With no other cause for the symptoms | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Is there a new onset of AF? | Order an exercise treadmill test | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No | Yes | Yes | No | Yes | No | Is PCWP> 25 mm Hg? | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No | Yes | Yes | No | Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Periodic monitoring | PMBC (Class IIa) | PMBC (Class I) | Mitral valve surgery (Class I) | PMBC (Class IIb) | Periodic monitoring | PMBC (Class IIb) | Periodic monitoring | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Secondary Prevention of Rheumatic Fever
Indications
Shown below is the table depicting the indication for secondary prophylaxis of rheumatic fever.[4]
| Indications | Duration of prophylaxis |
| ▸ Rheumatic fever with carditis and persistent valvular heart disease | ▸ 10 years or until the patient is 40 years (whichever is longer) (Class I, Level of Evidence C) |
| ▸ Rheumatic fever with carditis but no valvular heart disease | ▸ 10 years or until the patient is 21 years (whichever is longer) (Class I, Level of Evidence C) |
| ▸ Rheumatic fever without carditis | ▸ 5 years or until the patient is 21 years (whichever is longer) (Class I, Level of Evidence C) |
Antibiotic Regimens
Shown below is the table depicting the antibiotic regimens for secondary prophylaxis of rheumatic fever.[4]
| Antibiotics | Dosage |
| Penicillin G benzathine (Class I, Level of Evidence A) |
▸ Weight >27 Kg (60 lb): 1.2 million units IM every day for 4 weeks ▸ Weight ≤27 Kg (60 lb): 600,000 units IM every day for 4 weeks |
| Penicillin V (Class I, Level of Evidence B) |
▸ 200 mg orally twice a day |
| Sulfadiazine (Class I, Level of Evidence B) |
▸ Weight >27 Kg (60 lb): 1 g orally once a day ▸ Weight ≤27 Kg (60 lb): o.5 g orally once a day |
| Macrolide or azalide antibiotics (in patients allergic to penicillin) (Class I, Level of Evidence C) |
▸ Varies |
Do's
- Perform transesophageal echocardiography (TEE) in patients considered for PMBC to rule out left atrial thrombus and to determine mitral regurgitation severity.
- Perform exercise testing or invasive hemodynamic testing, when clinical signs and symptoms don't co-relate with echocardiographic findings.
- Perform mitral valve surgery in stage C and stage D mitral stenosis, if patient is undergoing cardiac surgery for some other indication.
- Perform mitral valve surgery in moderate mitral stenosis (mitral valve area: 1.6 - 2 cm2) if the patient is undergoing cardiac surgery for other indications.
- Perform mitral valve surgery with excision of left atrial appendage in stage C and stage D mitral stenosis patients who have had recurrent embolic events despite being on anticoagulation therapy.
- Perform TTE every 3-5 years in asymptomatic stage B MS patients and every 1-2 years in asymptomatic stage C MS patients who have mitral valve area 1-1.5 cm2 .
- Perform TTE once every year in asymptomatic stage C MS patients who have mitral valve area < 1 cm2.
- In cases of senile calcific mitral stenosis, intervention is done only when symptoms are severe and cannot be controlled with heart rate control and diuretics.
References
- ↑ Tadele, H.; Mekonnen, W.; Tefera, E. (2013). "Rheumatic mitral stenosis in Children: more accelerated course in sub-Saharan Patients". BMC Cardiovasc Disord. 13 (1): 95. doi:10.1186/1471-2261-13-95. PMID 24180350. Unknown parameter
|month=ignored (help) - ↑ 2.0 2.1 2.2 2.3 2.4 Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. doi:10.1161/CIR.0000000000000029. PMID 24589852.
- ↑ Boon NA, Bloomfield P (2002). "The medical management of valvar heart disease". Heart. 87 (4): 395–400. PMC 1767079. PMID 11907022.
- ↑ 4.0 4.1 Gerber MA, Baltimore RS, Eaton CB, Gewitz M, Rowley AH, Shulman ST; et al. (2009). "Prevention of rheumatic fever and diagnosis and treatment of acute Streptococcal pharyngitis: a scientific statement from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young, the Interdisciplinary Council on Functional Genomics and Translational Biology, and the Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics". Circulation. 119 (11): 1541–51. doi:10.1161/CIRCULATIONAHA.109.191959. PMID 19246689.