Medullary thyroid cancer pathophysiology: Difference between revisions
No edit summary |
|||
| (18 intermediate revisions by 2 users not shown) | |||
| Line 3: | Line 3: | ||
{{CMG}}; {{AE}} {{Ammu}} | {{CMG}}; {{AE}} {{Ammu}} | ||
==Overview== | ==Overview== | ||
Development of medullary thyroid cancer is the result of genetic mutation of [[RET proto-oncogene]]. On gross pathology, well circumscribed, gray, white, or yellow colored masses are characteristic findings of medullary thyroid cancer. On microscopic histopathological analysis, polygonal to spindle to small cells, [[interstitial edema]], and vascular hyalinized stroma are characteristic findings of medullary thyroid cancer. | Development of medullary thyroid cancer is the result of [[genetic mutation]] of [[RET proto-oncogene]]. On [[gross pathology]], well-circumscribed, gray, white, or yellow-colored [[Mass|masses]] are characteristic findings of medullary thyroid cancer. On microscopic [[Histopathological|histopathological analysis]], polygonal to the spindle to small cells, [[interstitial edema]], and vascular hyalinized stroma are characteristic findings of medullary thyroid cancer. | ||
==Pathogenesis== | ==Pathogenesis== | ||
* Medullary thyroid cancer is a form of [[Thyroid cancer|thyroid carcinoma]] which originates from the [[parafollicular cell]]s (C cells), which produce the hormone [[calcitonin]].<ref name="hu">Hu MI, Vassilopoulou-Sellin R, Lustig R, Lamont JP. [http://www.cancernetwork.com/cancer-management-11/chapter05/article/10165/1402668 "Thyroid and Parathyroid Cancers"] in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds) [http://www.cancernetwork.com/cancer-management-11/ Cancer Management: A Multidisciplinary Approach]. 11 ed. 2008.</ref> | |||
*[[Mutations]] in the [[RET proto-oncogene|''RET'' proto-oncogene]] (REarranged during Transfection), located on [[chromosome 10]], lead to the [[gene expression|expression]] of a mutated [[receptor tyrosine kinase]] protein. | |||
* Medullary thyroid cancer is a form of [[Thyroid cancer|thyroid carcinoma]] which originates from the [[parafollicular cell]]s (C cells), which produce the hormone [[calcitonin]].<ref name=hu>Hu MI, Vassilopoulou-Sellin R, Lustig R, Lamont JP. [http://www.cancernetwork.com/cancer-management-11/chapter05/article/10165/1402668 "Thyroid and Parathyroid Cancers"] in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds) [http://www.cancernetwork.com/cancer-management-11/ Cancer Management: A Multidisciplinary Approach]. 11 ed. 2008.</ref>It is characterized by consistent production of a hormonal marker called [[calcitonin]]. | *[[RET proto-oncogene|''RET'' proto-oncogene]] is involved in the regulation of cell growth and development and its [[germline mutation]] is responsible for nearly all cases of [[hereditary]] or familial medullary thyroid carcinoma. | ||
* Approximately 25% of reported cases of medullary thyroid carcinoma are familial. Familial medullary thyroid carcinoma syndromes include [[ | *[[Germline mutation]] of [[RET proto-oncogene|''RET'']] may also be responsible for the development of [[hyperparathyroidism]] and [[pheochromocytoma]]. | ||
* Medullary thyroid cancer may be sporadic or hereditary as part of [[MEN, type 2a|MEN type 2 A]] and [[MEN type IIb|B]].<ref name="WellsAsa2015">{{cite journal|last1=Wells|first1=Samuel A.|last2=Asa|first2=Sylvia L.|last3=Dralle|first3=Henning|last4=Elisei|first4=Rossella|last5=Evans|first5=Douglas B.|last6=Gagel|first6=Robert F.|last7=Lee|first7=Nancy|last8=Machens|first8=Andreas|last9=Moley|first9=Jeffrey F.|last10=Pacini|first10=Furio|last11=Raue|first11=Friedhelm|last12=Frank-Raue|first12=Karin|last13=Robinson|first13=Bruce|last14=Rosenthal|first14=M. Sara|last15=Santoro|first15=Massimo|last16=Schlumberger|first16=Martin|last17=Shah|first17=Manisha|last18=Waguespack|first18=Steven G.|title=Revised American Thyroid Association Guidelines for the Management of Medullary Thyroid Carcinoma|journal=Thyroid|volume=25|issue=6|year=2015|pages=567–610|issn=1050-7256|doi=10.1089/thy.2014.0335}}</ref><ref name="pmid15233908">{{cite journal |vauthors=Gertner ME, Kebebew E |title=Multiple endocrine neoplasia type 2 |journal=Curr Treat Options Oncol |volume=5 |issue=4 |pages=315–25 |date=August 2004 |pmid=15233908 |doi= |url=}}</ref> | |||
* Sporadic form accounts for 80% of the cases. This form usually occurs unilaterally. | |||
* Medullary thyroid carcinoma is a subtype of [[thyroid cancer]] which accounts for 5-10% of all [[Thyroid Cancer|thyroid malignancies]]. | |||
* It is characterized by consistent production of a hormonal [[marker]] called [[calcitonin]]. | |||
*[[Metastatic]] involvement may be seen in up to 50% at the time of presentation. | |||
* Approximately 25% of reported cases of medullary thyroid carcinoma are familial. | |||
*Hereditary medullary thyroid cancer is inherited as an [[autosomal dominant]] trait. | |||
*In the familial form, the [[tumor]] is almost always [[bilateral]]. | |||
*In addition, the familial form may be associated with [[benign]] or [[malignant tumors]] of other endocrine organs, commonly referred to as the [[multiple endocrine neoplasia]] syndromes. | |||
*Familial medullary thyroid carcinoma syndromes include:<ref name="pmid25810047">{{cite journal |vauthors=Wells SA, Asa SL, Dralle H, Elisei R, Evans DB, Gagel RF, Lee N, Machens A, Moley JF, Pacini F, Raue F, Frank-Raue K, Robinson B, Rosenthal MS, Santoro M, Schlumberger M, Shah M, Waguespack SG |title=Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma |journal=Thyroid |volume=25 |issue=6 |pages=567–610 |date=June 2015 |pmid=25810047 |pmc=4490627 |doi=10.1089/thy.2014.0335 |url=}}</ref> | |||
*[[Multiple endocrine neoplasia type 2A]] | |||
*[[Multiple endocrine neoplasia type 2B]] | |||
*familial non-multiple endocrine neoplasia syndromes | |||
* Medullary carcinoma usually presents as a hard mass and is often accompanied by [[blood vessel]] invasion. | |||
*[[Metastases]] to regional [[lymph nodes]] are found in about 50% of cases. | |||
==Genetics== | ==Genetics== | ||
* | * Medullary thyroid cancer is [[Association (statistics)|associated]] with [[RET proto-oncogene|''RET'' proto-oncogene]] [[mutations]].<ref name="pmid9506724">{{cite journal |vauthors=Berndt I, Reuter M, Saller B, Frank-Raue K, Groth P, Grussendorf M, Raue F, Ritter MM, Höppner W |title=A new hot spot for mutations in the ret protooncogene causing familial medullary thyroid carcinoma and multiple endocrine neoplasia type 2A |journal=J. Clin. Endocrinol. Metab. |volume=83 |issue=3 |pages=770–4 |date=March 1998 |pmid=9506724 |doi=10.1210/jcem.83.3.4619 |url=}}</ref> | ||
==Associated Conditions== | ==Associated Conditions== | ||
* [[ Von Hippel-Lindau Disease]] | * Medullary thyroid cancer may be [[Association (statistics)|associated]] with:<ref name="ErcolinoLai2014">{{cite journal|last1=Ercolino|first1=Tonino|last2=Lai|first2=Roberta|last3=Giachè|first3=Valentino|last4=Melchionda|first4=Salvatore|last5=Carella|first5=Massimo|last6=Delitala|first6=Alessandro|last7=Mannelli|first7=Massimo|last8=Fanciulli|first8=Giuseppe|title=Patient affected by neurofibromatosis type 1 and thyroid C-cell hyperplasia harboring pathogenic germ-line mutations in both NF1 and RET genes|journal=Gene|volume=536|issue=2|year=2014|pages=332–335|issn=03781119|doi=10.1016/j.gene.2013.12.003}}</ref><ref name="KochBrouwers2006">{{cite journal|last1=Koch|first1=Christian A|last2=Brouwers|first2=Frederieke M|last3=Vortmeyer|first3=Alexander O|last4=Tannapfel|first4=Andrea|last5=Libutti|first5=Steven K|last6=Zhuang|first6=Zhengping|last7=Pacak|first7=Karel|last8=Neumann|first8=Hartmut PH|last9=Paschke|first9=Ralf|title=Somatic VHLgene alterations in MEN2-associated medullary thyroid carcinoma|journal=BMC Cancer|volume=6|issue=1|year=2006|issn=1471-2407|doi=10.1186/1471-2407-6-131}}</ref><ref name="RaueFrank-Raue2015">{{cite journal|last1=Raue|first1=Friedhelm|last2=Frank-Raue|first2=Karin|title=Epidemiology and Clinical Presentation of Medullary Thyroid Carcinoma|volume=204|year=2015|pages=61–90|issn=0080-0015|doi=10.1007/978-3-319-22542-5_3}}</ref> | ||
* [[Neurofibromatosis type 1]] | **[[MEN 2a|MEN2A]] | ||
**[[MEN 2B|MEN2B]] | |||
**[[Pheochromocytoma]] | |||
**[[Parathyroid adenoma]] | |||
** Cutaneous lichen [[amyloidosis]] | |||
** Mucosal neuroma | |||
**[[Von Hippel-Lindau Disease]] | |||
**[[Neurofibromatosis type 1]] | |||
==Gross Pathology== | ==Gross Pathology== | ||
* Medullary thyroid cancer is usually | * Medullary thyroid cancer is usually a well circumscribed, gray, white, or yellow colored mass which is gritty to firm in consistency.<ref name="HusainShukla2014">{{cite journal|last1=Husain|first1=Nuzhat|last2=Shukla|first2=Saumya|last3=Awasthi|first3=NamrataP|title=Papillary variant of medullary carcinoma thyroid|journal=Indian Journal of Pathology and Microbiology|volume=57|issue=1|year=2014|pages=151|issn=0377-4929|doi=10.4103/0377-4929.130933}}</ref> | ||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
* | * On microscopic [[histopathological]] analysis, presence of [[amyloid]] is a characteristic finding of medullary thyroid cancer.<ref name="pmid2654432">{{cite journal |vauthors=Nelkin BD, de Bustros AC, Mabry M, Baylin SB |title=The molecular biology of medullary thyroid carcinoma. A model for cancer development and progression |journal=JAMA |volume=261 |issue=21 |pages=3130–5 |date=June 1989 |pmid=2654432 |doi= |url=}}</ref><ref name="ValentaMichel-Bechet1977">{{cite journal|last1=Valenta|first1=Lubomir J.|last2=Michel-Bechet|first2=Marc|last3=Mattson|first3=Joan C.|last4=Singer|first4=Frederick R.|title=Microfollicular thyroid carcinoma with amyloid rich stroma, resembling the medullary carcinoma of the thyroid (MCT)|journal=Cancer|volume=39|issue=4|year=1977|pages=1573–1586|issn=0008-543X|doi=10.1002/1097-0142(197704)39:4<1573::AID-CNCR2820390433>3.0.CO;2-A}}</ref> | ||
=== | * Other microscopic features associated with the [[diagnosis]] of medullary thyroid cancer include: | ||
** The majority of [[tumor]] cells are epithelioid, but spindle cells may be found as well. | |||
** The nuclei demonstrate the characteristic granular appearance known as salt-and-pepper. | |||
** The [[cytoplasm]] of [[Tumor cell|tumor cells]] contains perinuclear calcitonin-containing azurophilic granules that are best seen in samples stained with the May–Grünwald–Giemsa stain. | |||
: | {| {{table}} cellpadding="4" cellspacing="0" style="border:#c9c9c9 1px solid; margin: 1em 1em 1em 0; border-collapse: collapse;" | ||
: | | align="center" style="background: #4479BA;" | {{fontcolor|#FFF|''' Medullary thyroid cancer'''}} | ||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Image'''}} | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Image'''}} | |||
|- | |||
| | |||
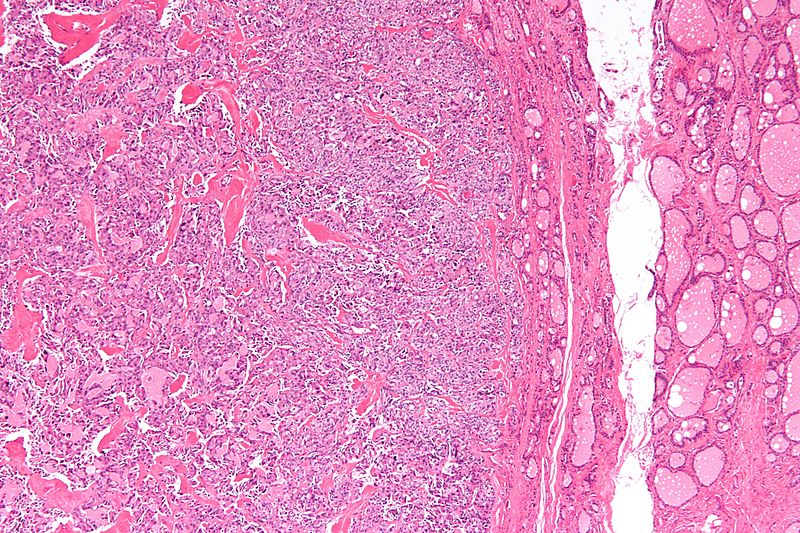
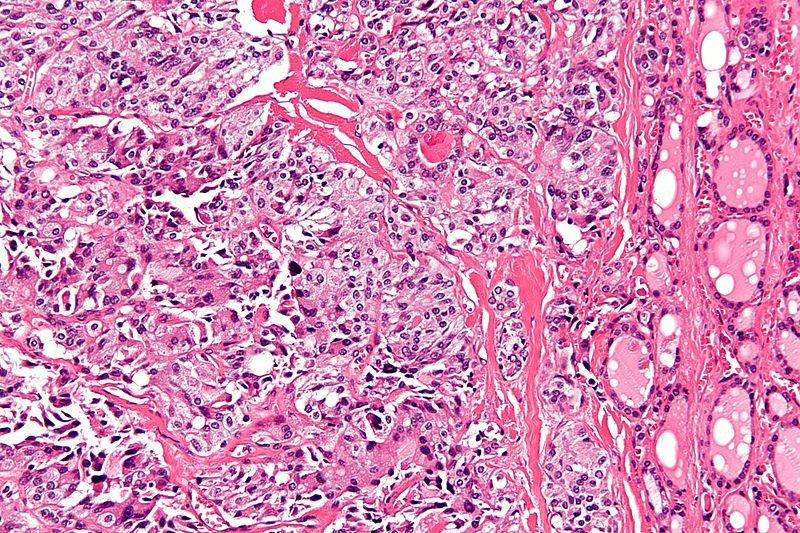
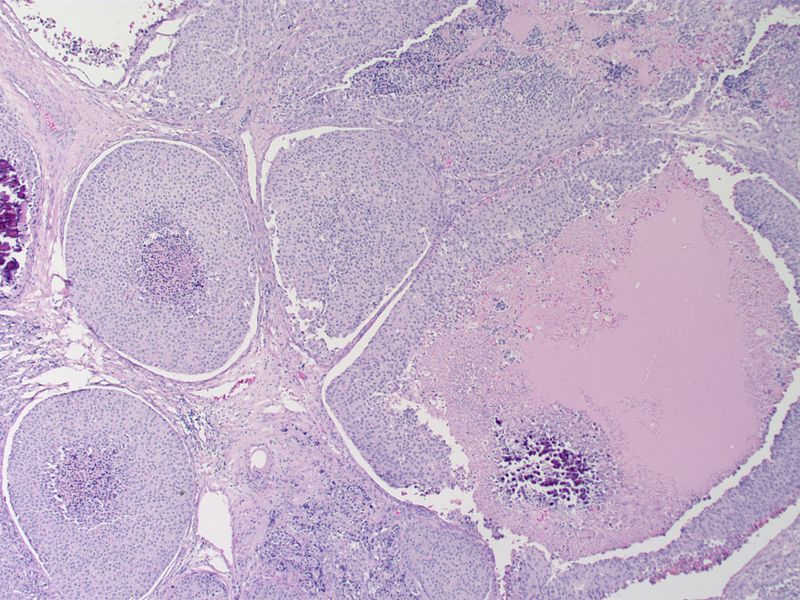
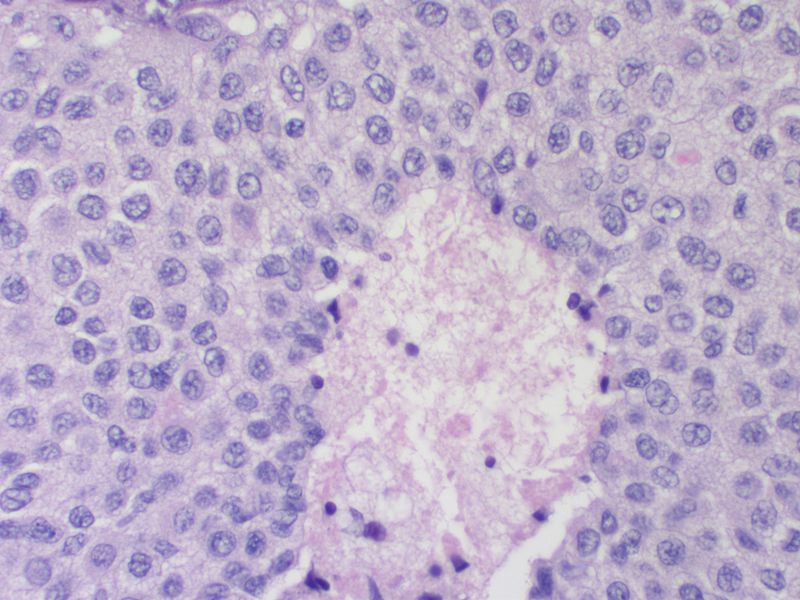
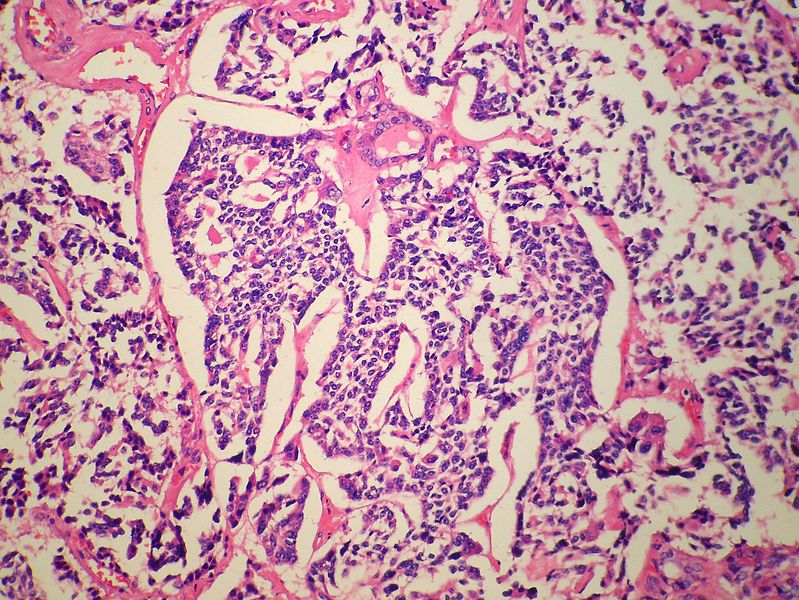
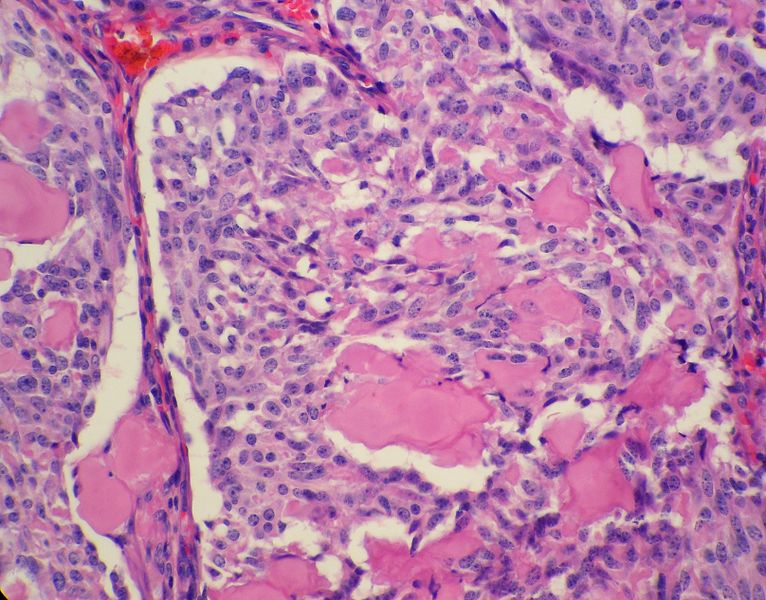
: | * Medullary thyroid carcinoma | ||
: | |[[File:Medullary thyroid carcinoma - low mag.jpg|thumb|none|250px| H&E stain, low power. Contributed in wikimedia.commons]] | ||
: | |[[File:Medullary thyroid carcinoma - high mag.jpg|thumb|none|250px| H&E stain, high power. Contributed in wikimedia.commons]] | ||
|- | |||
=== | | | ||
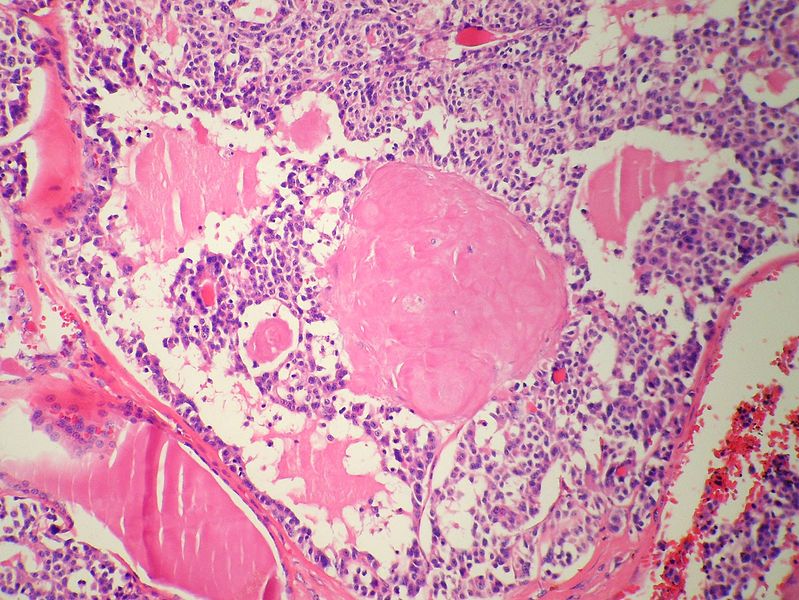
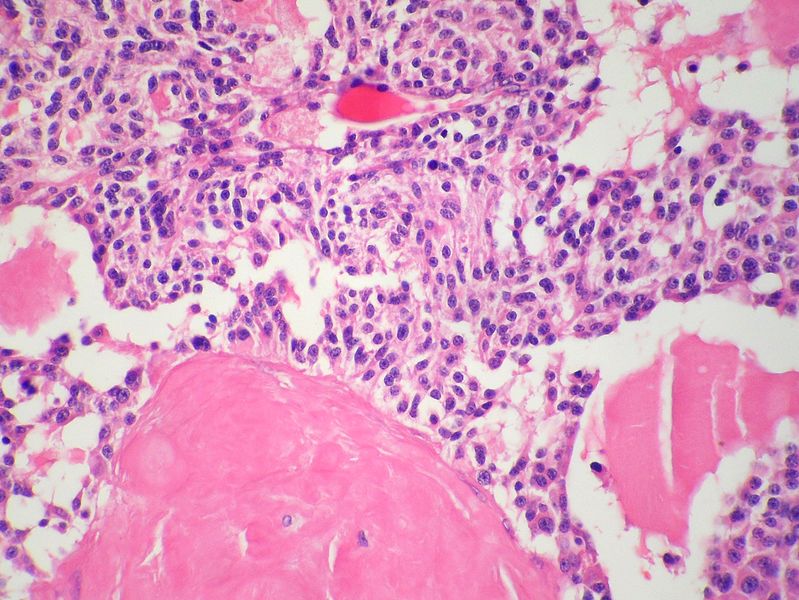
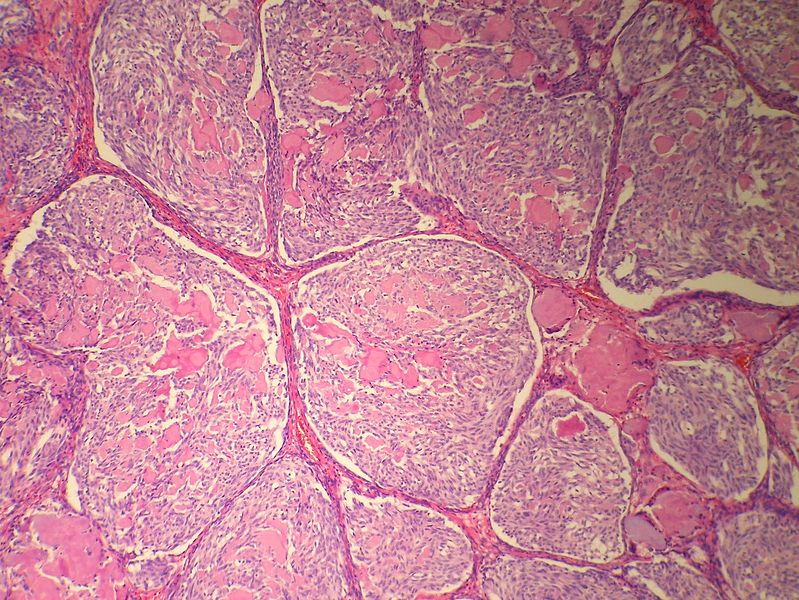
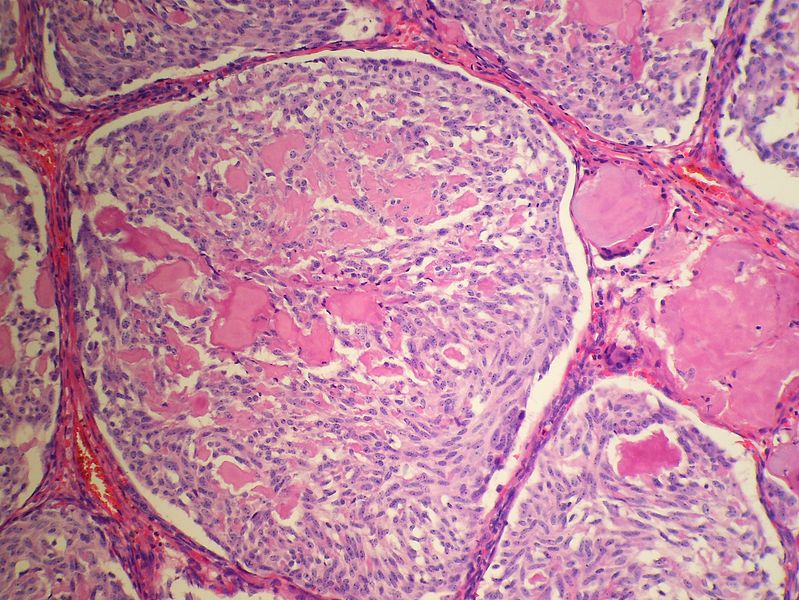
: | * Medullary thyroid cancer amyloid | ||
|[[File:Thyroid MedullaryCarcinoma Amyloid MP PA.JPG|thumb|none|250px| H&E stain, medium power. Contributed in wikimedia.commons]] | |||
|[[File:Thyroid MedullaryCarcinoma Amyloid HP PA.JPG|thumb|none|250px| H&E stain, high power. Contributed in wikimedia.commons]] | |||
|- | |||
| | |||
* Thyroid MedullaryCarcinoma Comedonecrosis | |||
|[[File:Thyroid MedullaryCarcinoma Comedonecrosis LP2 CTR.jpg|thumb|none|250px| H&E stain, medium power. Contributed in wikimedia.commons]] | |||
|[[File:Thyroid MedullaryCarcinoma Comedonecrosis HP CTR.jpg|thumb|none|250px| H&E stain, high power. Contributed in wikimedia.commons]] | |||
|- | |||
| | |||
* Medullary thyroid carcinoma spindle cell | |||
|[[File:Thyroid MedullaryCarcinoma SpindleCell LP PA.JPG|thumb|none|250px| H&E stain, low power. Contributed in wikimedia.commons]] | |||
|[[File:Thyroid MedullaryCarcinoma SpindleCell MP PA.JPG|thumb|none|250px| H&E stain, medium power. Contributed in wikimedia.commons]] | |||
|- | |||
| | |||
* Medullary thyroid carcinoma spindle cell | |||
|[[File:Thyroid MedullaryCarcinoma SmallCell HP PA.JPG|thumb|none|250px| H&E stain, low power. Contributed in wikimedia.commons]] | |||
|[[File:Thyroid MedullaryCarcinoma SpindleCell LP2 PA.JPG|thumb|none|250px| H&E stain, high power. Contributed in wikimedia.commons]] | |||
|} | |||
* For more images of medullary thyroid cancer please [[Medullary thyroid cancer biopsy|click here]] | |||
==Immunohistochemistry== | |||
*[[Marker|Markers]] associated with medullary throid cancers include:<ref name="NakazawaCameselle-Teijeiro2014">{{cite journal|last1=Nakazawa|first1=Tadao|last2=Cameselle-Teijeiro|first2=José|last3=Vinagre|first3=João|last4=Soares|first4=Paula|last5=Rousseau|first5=Emmanuel|last6=Eloy|first6=Catarina|last7=Sobrinho-Simões|first7=Manuel|title=C-Cell-Derived Calcitonin-Free Neuroendocrine Carcinoma of the Thyroid|journal=International Journal of Surgical Pathology|volume=22|issue=6|year=2014|pages=530–535|issn=1066-8969|doi=10.1177/1066896914525228}}</ref><ref name="MendelsohnWells1984">{{cite journal|last1=Mendelsohn|first1=Geoffrey|last2=Wells|first2=Samuel A.|last3=Baylin|first3=Stephen B.|title=Relationship of tissue carcinoembryonic antigen and calcitonin to tumor virulence in medullary thyroid carcinoma. An immunohistochemical study in early, localized, and virulent disseminated stages of disease|journal=Cancer|volume=54|issue=4|year=1984|pages=657–662|issn=0008-543X|doi=10.1002/1097-0142(1984)54:4<657::AID-CNCR2820540412>3.0.CO;2-V}}</ref><ref name="pmid2654432">{{cite journal |vauthors=Nelkin BD, de Bustros AC, Mabry M, Baylin SB |title=The molecular biology of medullary thyroid carcinoma. A model for cancer development and progression |journal=JAMA |volume=261 |issue=21 |pages=3130–5 |date=June 1989 |pmid=2654432 |doi= |url=}}</ref> | |||
**[[Calcitonin]] | |||
** [[Chromogranin]] | |||
** [[CEA]] | |||
** Calcitonin gene-related peptide (CGRP) | |||
** [[Somatostatin]] | |||
** [[Serotonin]] | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
Latest revision as of 14:27, 1 October 2019
|
Medullary thyroid cancer Microchapters |
|
Differentiating Medullary thyroid cancer from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Medullary thyroid cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Medullary thyroid cancer pathophysiology |
|
Risk calculators and risk factors for Medullary thyroid cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
Overview
Development of medullary thyroid cancer is the result of genetic mutation of RET proto-oncogene. On gross pathology, well-circumscribed, gray, white, or yellow-colored masses are characteristic findings of medullary thyroid cancer. On microscopic histopathological analysis, polygonal to the spindle to small cells, interstitial edema, and vascular hyalinized stroma are characteristic findings of medullary thyroid cancer.
Pathogenesis
- Medullary thyroid cancer is a form of thyroid carcinoma which originates from the parafollicular cells (C cells), which produce the hormone calcitonin.[1]
- Mutations in the RET proto-oncogene (REarranged during Transfection), located on chromosome 10, lead to the expression of a mutated receptor tyrosine kinase protein.
- RET proto-oncogene is involved in the regulation of cell growth and development and its germline mutation is responsible for nearly all cases of hereditary or familial medullary thyroid carcinoma.
- Germline mutation of RET may also be responsible for the development of hyperparathyroidism and pheochromocytoma.
- Medullary thyroid cancer may be sporadic or hereditary as part of MEN type 2 A and B.[2][3]
- Sporadic form accounts for 80% of the cases. This form usually occurs unilaterally.
- Medullary thyroid carcinoma is a subtype of thyroid cancer which accounts for 5-10% of all thyroid malignancies.
- It is characterized by consistent production of a hormonal marker called calcitonin.
- Metastatic involvement may be seen in up to 50% at the time of presentation.
- Approximately 25% of reported cases of medullary thyroid carcinoma are familial.
- Hereditary medullary thyroid cancer is inherited as an autosomal dominant trait.
- In the familial form, the tumor is almost always bilateral.
- In addition, the familial form may be associated with benign or malignant tumors of other endocrine organs, commonly referred to as the multiple endocrine neoplasia syndromes.
- Familial medullary thyroid carcinoma syndromes include:[4]
- Multiple endocrine neoplasia type 2A
- Multiple endocrine neoplasia type 2B
- familial non-multiple endocrine neoplasia syndromes
- Medullary carcinoma usually presents as a hard mass and is often accompanied by blood vessel invasion.
- Metastases to regional lymph nodes are found in about 50% of cases.
Genetics
- Medullary thyroid cancer is associated with RET proto-oncogene mutations.[5]
Associated Conditions
- Medullary thyroid cancer may be associated with:[6][7][8]
- MEN2A
- MEN2B
- Pheochromocytoma
- Parathyroid adenoma
- Cutaneous lichen amyloidosis
- Mucosal neuroma
- Von Hippel-Lindau Disease
- Neurofibromatosis type 1
Gross Pathology
- Medullary thyroid cancer is usually a well circumscribed, gray, white, or yellow colored mass which is gritty to firm in consistency.[9]
Microscopic Pathology
- On microscopic histopathological analysis, presence of amyloid is a characteristic finding of medullary thyroid cancer.[10][11]
- Other microscopic features associated with the diagnosis of medullary thyroid cancer include:
- The majority of tumor cells are epithelioid, but spindle cells may be found as well.
- The nuclei demonstrate the characteristic granular appearance known as salt-and-pepper.
- The cytoplasm of tumor cells contains perinuclear calcitonin-containing azurophilic granules that are best seen in samples stained with the May–Grünwald–Giemsa stain.
- For more images of medullary thyroid cancer please click here
Immunohistochemistry
- Markers associated with medullary throid cancers include:[12][13][10]
- Calcitonin
- Chromogranin
- CEA
- Calcitonin gene-related peptide (CGRP)
- Somatostatin
- Serotonin
References
- ↑ Hu MI, Vassilopoulou-Sellin R, Lustig R, Lamont JP. "Thyroid and Parathyroid Cancers" in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds) Cancer Management: A Multidisciplinary Approach. 11 ed. 2008.
- ↑ Wells, Samuel A.; Asa, Sylvia L.; Dralle, Henning; Elisei, Rossella; Evans, Douglas B.; Gagel, Robert F.; Lee, Nancy; Machens, Andreas; Moley, Jeffrey F.; Pacini, Furio; Raue, Friedhelm; Frank-Raue, Karin; Robinson, Bruce; Rosenthal, M. Sara; Santoro, Massimo; Schlumberger, Martin; Shah, Manisha; Waguespack, Steven G. (2015). "Revised American Thyroid Association Guidelines for the Management of Medullary Thyroid Carcinoma". Thyroid. 25 (6): 567–610. doi:10.1089/thy.2014.0335. ISSN 1050-7256.
- ↑ Gertner ME, Kebebew E (August 2004). "Multiple endocrine neoplasia type 2". Curr Treat Options Oncol. 5 (4): 315–25. PMID 15233908.
- ↑ Wells SA, Asa SL, Dralle H, Elisei R, Evans DB, Gagel RF, Lee N, Machens A, Moley JF, Pacini F, Raue F, Frank-Raue K, Robinson B, Rosenthal MS, Santoro M, Schlumberger M, Shah M, Waguespack SG (June 2015). "Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma". Thyroid. 25 (6): 567–610. doi:10.1089/thy.2014.0335. PMC 4490627. PMID 25810047.
- ↑ Berndt I, Reuter M, Saller B, Frank-Raue K, Groth P, Grussendorf M, Raue F, Ritter MM, Höppner W (March 1998). "A new hot spot for mutations in the ret protooncogene causing familial medullary thyroid carcinoma and multiple endocrine neoplasia type 2A". J. Clin. Endocrinol. Metab. 83 (3): 770–4. doi:10.1210/jcem.83.3.4619. PMID 9506724.
- ↑ Ercolino, Tonino; Lai, Roberta; Giachè, Valentino; Melchionda, Salvatore; Carella, Massimo; Delitala, Alessandro; Mannelli, Massimo; Fanciulli, Giuseppe (2014). "Patient affected by neurofibromatosis type 1 and thyroid C-cell hyperplasia harboring pathogenic germ-line mutations in both NF1 and RET genes". Gene. 536 (2): 332–335. doi:10.1016/j.gene.2013.12.003. ISSN 0378-1119.
- ↑ Koch, Christian A; Brouwers, Frederieke M; Vortmeyer, Alexander O; Tannapfel, Andrea; Libutti, Steven K; Zhuang, Zhengping; Pacak, Karel; Neumann, Hartmut PH; Paschke, Ralf (2006). "Somatic VHLgene alterations in MEN2-associated medullary thyroid carcinoma". BMC Cancer. 6 (1). doi:10.1186/1471-2407-6-131. ISSN 1471-2407.
- ↑ Raue, Friedhelm; Frank-Raue, Karin (2015). "Epidemiology and Clinical Presentation of Medullary Thyroid Carcinoma". 204: 61–90. doi:10.1007/978-3-319-22542-5_3. ISSN 0080-0015.
- ↑ Husain, Nuzhat; Shukla, Saumya; Awasthi, NamrataP (2014). "Papillary variant of medullary carcinoma thyroid". Indian Journal of Pathology and Microbiology. 57 (1): 151. doi:10.4103/0377-4929.130933. ISSN 0377-4929.
- ↑ 10.0 10.1 Nelkin BD, de Bustros AC, Mabry M, Baylin SB (June 1989). "The molecular biology of medullary thyroid carcinoma. A model for cancer development and progression". JAMA. 261 (21): 3130–5. PMID 2654432.
- ↑ Valenta, Lubomir J.; Michel-Bechet, Marc; Mattson, Joan C.; Singer, Frederick R. (1977). "Microfollicular thyroid carcinoma with amyloid rich stroma, resembling the medullary carcinoma of the thyroid (MCT)". Cancer. 39 (4): 1573–1586. doi:10.1002/1097-0142(197704)39:4<1573::AID-CNCR2820390433>3.0.CO;2-A. ISSN 0008-543X.
- ↑ Nakazawa, Tadao; Cameselle-Teijeiro, José; Vinagre, João; Soares, Paula; Rousseau, Emmanuel; Eloy, Catarina; Sobrinho-Simões, Manuel (2014). "C-Cell-Derived Calcitonin-Free Neuroendocrine Carcinoma of the Thyroid". International Journal of Surgical Pathology. 22 (6): 530–535. doi:10.1177/1066896914525228. ISSN 1066-8969.
- ↑ Mendelsohn, Geoffrey; Wells, Samuel A.; Baylin, Stephen B. (1984). "Relationship of tissue carcinoembryonic antigen and calcitonin to tumor virulence in medullary thyroid carcinoma. An immunohistochemical study in early, localized, and virulent disseminated stages of disease". Cancer. 54 (4): 657–662. doi:10.1002/1097-0142(1984)54:4<657::AID-CNCR2820540412>3.0.CO;2-V. ISSN 0008-543X.