Measles laboratory findings
|
Measles Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Measles laboratory findings On the Web |
|
American Roentgen Ray Society Images of Measles laboratory findings |
|
Risk calculators and risk factors for Measles laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Measles is a disease best diagnosed clinically, however laboratory tests have a limited role to play especially in those conditions where the diagnosis is uncertain and certain cases of atypical pneumonia. Detecting a positive rise in measles IgM antibodies is one of the methods used for laboratory diagnosis of measles.
Laboratory Findings
Laboratory confirmation is essential for all sporadic measles cases and all outbreaks. Detection of measles-specific IgM antibody and measles RNA by real-time polymerase chain reaction (RT-PCR) are the most common methods for confirming measles infection. Healthcare providers should obtain both a serum sample and a throat swab (or nasopharyngeal swab) from patients suspected to have measles at first contact with them. Urine samples may also contain virus, and when feasible to do so, collecting both respiratory and urine samples can increase the likelihood of detecting measles virus. [1]
In cases of measles infection following secondary vaccine failure IgM antibody may not be present. In these cases serological confirmation may be made by showing IgG antibody rises by Enzyme immunoasay or complement fixation. IgM antibodies are tested in a blood sample taken at least 4-5 days after appearance of rash and persist for 30-60 days thereafter. False positives are sometimes seen. More than 4 fold rise in IgG antibodies between actue and convalescent phase sera, is also diagnostic.
Positive contact with other patients known to have measles adds strong epidemiological evidence to the diagnosis.
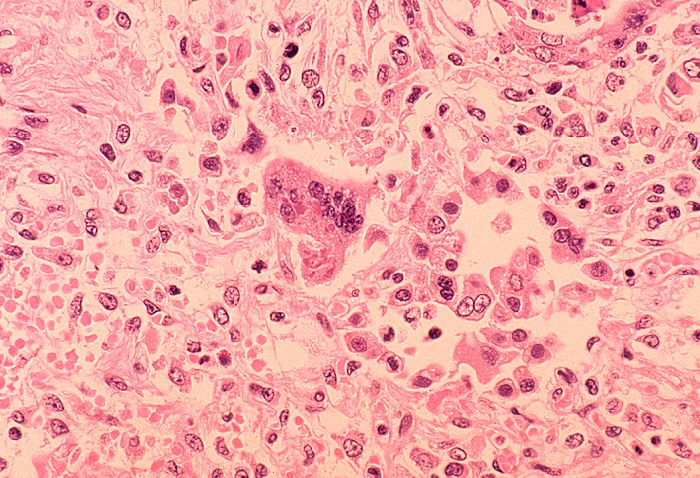
Some patients will develop pneumonia as a sequela to the measles. Histologically, a unique cell can be found in the paracortical region of hyperplastic lymph nodes in patients affected with this condition. This cell, known as the Warthin-Finkeldey cell, is a multinucleated giant with eosinophilic cytoplasmic and nuclear inclusions. Shown below is an image depicting histological section of lung specimen in a patient with measles associated pneumonia: