Kidney stone
Template:DiseaseDisorder infobox
|
WikiDoc Resources for Kidney stone |
|
Articles |
|---|
|
Most recent articles on Kidney stone Most cited articles on Kidney stone |
|
Media |
|
Powerpoint slides on Kidney stone |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Kidney stone at Clinical Trials.gov Clinical Trials on Kidney stone at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Kidney stone
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Kidney stone Discussion groups on Kidney stone Patient Handouts on Kidney stone Directions to Hospitals Treating Kidney stone Risk calculators and risk factors for Kidney stone
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Kidney stone |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Kidney stones, also called renal calculi, are solid concretions (crystal aggregations) of dissolved minerals in urine; calculi typically form inside the kidneys or bladder. The terms nephrolithiasis and urolithiasis refer to the presence of calculi in the kidneys and urinary tract, respectively.
Renal calculi can vary in size from as small as grains of sand to as large as grapefruit. Kidney stones typically leave the body by passage in the urine stream, and many stones are formed and passed without causing symptoms. If stones grow to sufficient size before passage — on the order of at least 2-3 millimeters — they can cause obstruction of the ureter. The resulting obstruction with dilation or stretching of the upper ureter and renal pelvis as well as spasm of muscle, trying to move the stone, can cause severe episodic pain, most commonly felt in the flank, lower abdomen and groin (a condition called renal colic). Renal colic can be associated with nausea and vomiting due to the embyrological association of the kidneys with the intestinal tract. Hematuria (bloody urine) is commonly present due to damage to the lining of the urinary tract. Recurrence rates are estimated at about 10% per year. Men are affected approximately 4 times more often than women.
Causes
Kidney stones can be due to underlying metabolic conditions, such as renal tubular acidosis, Dent's disease and medullary sponge kidney. Many health facilities will screen for such disorders in patients with recurrent kidney stones. This is typically done with a 24 hour urine collection that is chemically analyzed for deficiencies and excesses that promote stone formation.
- Calcium nephrolithiasis
- Cystine
- Drug induced
- High urine pH
- High urinary sodium
- Hypercalciuria
- Hyperoxaluria
- Hyperuricosuria
- Hypocitaturia
- Hypomagnesiuria
- Inadequate amounts of inhibitors of stone formation
- Infection with urea splitting microorganisms
- Low urine volume
- Low urine pH
- Presence of nidus for crystal precipitation
- Struvite
- Supersaturatin of stone forming compunds in urine
- Uric acid nephrolithiasis
- Urinary obstruction
- Urinary stasis
Calcium oxalate stones
The most common type of kidney stone is composed of calcium oxalate crystals, and factors that promote the precipitation of crystals in the urine are associated with the development of these stones.
Conventional wisdom and common sense have long held that consumption of too much calcium could promote the development of calcium kidney stones. However, current evidence suggests that the consumption of low-calcium diets is actually associated with a higher overall risk for the development of kidney stones. This is perhaps related to the role of calcium in binding ingested oxalate in the gastrointestinal tract. As the amount of calcium intake decreases, the amount of oxalate available for absorption into the bloodstream increases; this oxalate is then excreted in greater amounts into the urine by the kidneys. In the urine, oxalate is a very strong promoter of calcium oxalate precipitation, about 15 times stronger than calcium.
Other types
Other types of kidney stones are composed of struvite (magnesium, ammonium and phosphate); uric acid; calcium phosphate; and cystine.
The formation of struvite stones is associated with the presence of urea-splitting bacteria, most commonly Proteus mirabilis (but also Klebsiella, Serratia, Providencia species). These organisms are capable of splitting urea into ammonia, decreasing the acidity of the urine and resulting in favorable conditions for the formation of struvite stones. Stuvite stones are always associated with urinary tract infections.
The formation of uric acid stones is associated with conditions that cause high blood uric acid levels, such as gout, leukemias/lymphomas treated by chemotherapy (secondary gout from the death of leukemic cells), and acid/base metabolism disorders where the urine is excessively acid resulting in uric acid precipitation.
The formation of calcium phosphate stones is associated with conditions such as hyperparathyroidism and renal tubular acidosis.
The formation of cystine stones is uniquely associated with people suffering from cystinuria, who accumulate cystine in their urine.
Symptoms
Symptoms of kidney stones include:
- Colicky pain: "loin to groin". Often described as the "the worst pain I've ever experienced"[1]
- Hematuria: blood in the urine, due to minor damage to inside wall of kidney, ureter and/or urethra
- Dysuria: burning on urination when passing stones (rare). More typical of infection.
- Oliguria: reduced urinary volume caused by obstruction of the bladder or urethra by stone, or extremely rarely, simultaneous obstruction of both ureters by a stone.
- Nausea/vomiting: embryological link with intestine — stimulates vomiting center
Diagnosis
Clinical diagnosis is usually made on the basis of the location and severity of the pain, which is typically colic in nature (comes and goes in spasmodic waves).
Imaging is used to confirm the diagnosis and a number of other tests can be undertaken to help establish both the possible cause and consequences of the stone. Ultrasound imaging is also useful as it will give details about the presence of hydronephrosis (swelling of the kidney - suggesting the stone is blocking the outflow of urine). It can also be used to show the kidneys during pregnancy when standard x-rays are discouraged. About 10% of stones do not have enough calcium to be seen on standard x-rays (radiolucent stones) and may show up on ultrasound although they typically are seen on CT scans.
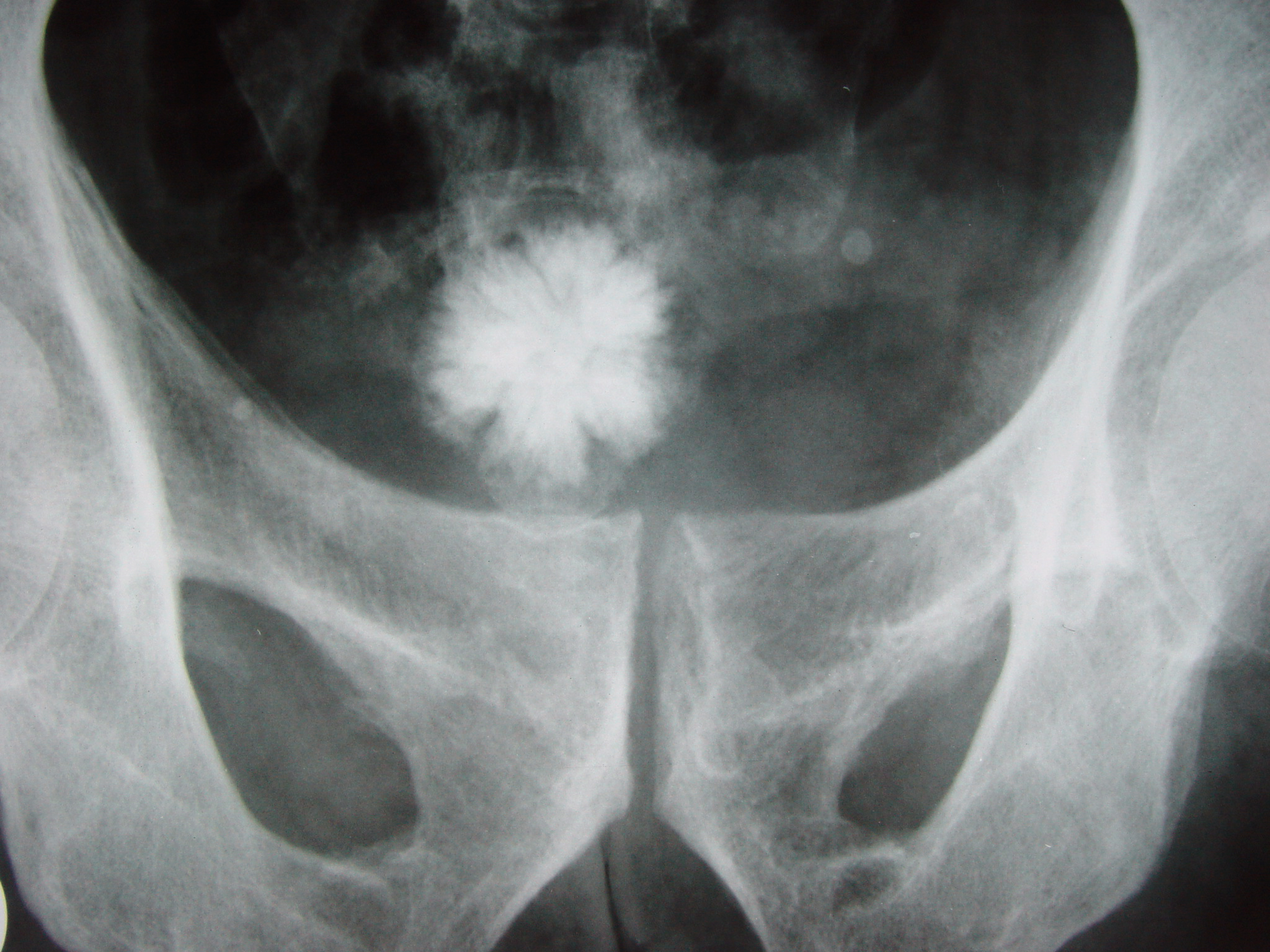
The relatively dense calcium renders these stones radio-opaque and they can be detected by a traditional X-ray of the abdomen that includes the Kidneys, Ureters and Bladder—KUB. This may be followed by an IVP (Intravenous Pyelogram; (IntraVenous Urogram (IVU) is the same test by another name)) which requires about 50 ml of a special dye to be injected into the bloodstream that is excreted by the kidneys and by its density helps outline any stone on a repeated X-ray. These can also be detected by a Retrograde pyelogram where similar "dye" is injected directly into the ureteral opening in the bladder by a surgeon, usually a urologist.
Computed tomography (CT or CAT scan), a specialized X-ray, is considered the gold-standard diagnostic test for the detection of kidney stones, and in this setting does not require the use of intravenous contrast, which carries some risk in certain people (eg, allergy, kidney damage). All stones are detectable by CT except very rare stones composed of certain drug residues in the urine. The non-contrast "renal colic study" CT scan has become the standard test for the immediate diagnosis of flank pain typical of a kidney stone. If positive for stones, a single standard x-ray of the abdomen (KUB) is recommended. This additional x-ray provides the physicians with a clearer idea of the exact size and shape of the stone as well as its surgical orientation. Further, it makes it simple to follow the progress of the stone without the need for the much more expensive CT scan just by doing another single x-ray at some point in the future.
Other investigations typically carried out include:
- Microscopic study of urine, which may show proteins, red blood cells, pus cells, bacteria, cellular casts and crystals.
- Culture of a urine sample to exclude urine infection (either as a differential cause of the patient's pain, or secondary to the presence of a stone)
- Blood tests: Full blood count for the presence of a raised white cell count (Neutrophilia) suggestive of infection, a check of renal function and to look for abnormally high blood calcium blood levels (hypercalcaemia).
- 24 hour urine collection to measure total daily urinary volume, magnesium, sodium, uric acid, calcium, citrate, oxalate and phosphate.
Differential Diagnosis of Causes of Kidney stone
Calcium stones
- Bone metastases
- Cushing's Syndrome
- Distal Renal Tubular Acidosis
- Excessive Vitamin C intake
- Hypercalcemia
- Hyperthyroidism
- Hyperoxaluria
- Hyperuricuria
- Hypophosphaturia
- Idiopathic hypercalcuria
- Increased intestinal absorbtion of oxalates
- Leukemia
- Milk-alkali syndrome
- Osteoporosis
- Paget's Disease
- Sarcoidosis
- Tumor hypercalcemias
- Vitamin D intoxication
Infectious Stones
- Klebsiella
- Proteus
- Pseudomonas
Uric Acid Stones
- Alcohol Abuse
- Dehydration
- Drugs
- Gout
- Idiopathic
- Purine metabolism
- Tumor
Congenital Stones
- Cystinuria
Treatment
Temporizing

About 90% of stones 4 mm or less in size usually will pass spontaneously, however the majority of stones greater than 6 mm will require some form of intervention. In most cases, a smaller stone that is not symptomatic is often given up to 30 days to move or pass before consideration is given to any surgical intervention as it has been found that waiting longer tends to lead to additional complications. Immediate surgery may be required in certain situations such as in people with only one working kidney, intractable pain or in the presence of an infected kidney blocked by a stone which can rapidly cause severe sepsis and toxic shock.
Analgesia
Management of pain from kidney stones varies from country to country and even from physician to physician, but usually requires intravenous administration of narcotics in an emergency room setting for acute situations. Similar classes of drugs may be reasonably effective orally in an outpatient setting for less severe discomfort where nonsteroidal anti-inflammatories or narcotics like codeine can be prescribed. Some doctors will give patients with recurring passing of small stones a small supply prescription for hydrocodone to avoid a future visit to the ER when the next episode occurs. Taken at the first sign of pain, hydrocodone can eliminate much of the acute pain, nausea and vomiting which necessitates the hospital visit and still facilitate stone passage, although a follow-up with a physician is still necessary.
The current standard of care for acute ureteral colic caused by a kidney stone in patients who are not allergic to aspirin, is intramuscular or intravenous injection of the non-steroidal medication Ketorolac (Toradol). Patients who are to be treated non-surgically, may also be started on an alpha adrenergic blocking agent (such as Flomax, Uroxatral, terazosin or doxazosin), which acts to reduce the muscle tone of the ureter and facilitate stone passage. For smaller stones near the bladder, this type of medical treatment can increase the spontaneous stone passage rate by about 30%.
After treatment, the pain may return if the stone moves but re-obstructs in another location. Patients are encouraged to strain their urine so they can collect the stone when it eventually passes and send it for chemical composition analysis which will be used along with a 24 hour urine chemical analysis test to establish preventative options.
Urologic interventions
Most kidney stones don't require surgery and will pass on their own. Surgery is necessary when the pain is persistent and severe, in renal failure and when there is a kidney infection. It may also be advisible if the stone fails to pass or move after 30 days. Finding a significant stone before it passes into the ureter allows physicians to fragment it surgically before it causes any severe problems. In most of these cases, non-invasive Extracorporeal Shock Wave Lithotripsy or (ESWL) will be used. Otherwise some form of invasive procedure is required; with approaches including ureteroscopic fragmentation (or simple basket extraction if feasible) using laser, ultrasonic or mechanical (pneumatic, shock-wave) forms of energy to fragment the larger stones. Percutaneous nephrolithotomy or rarely open surgery may ultimately be necessary for large or complicated stones or stones which fail other less invasive attempts at treatment.
A single retrospective study in the USA, at the Mayo Clinic, has suggested that lithotripsy may increase subsequent incidence of diabetes and hypertension,[2] but it has not been felt warranted to change clinical practice at the clinic.[3] The study reflects early experience with the original lithotripsy machine which had a very large blast path, much larger than what is used on modern machines. Further study is believed necessary to determine how much risk this treatment actually has using modern machines and treatment regimens.
More common complications related to ESWL are bleeding, pain related to passage of stone fragments, failure to fragment the stone, and the possible requirement for additional or alternative interventions.
Ureteral (double-J) stents
One modern medical technique uses a ureteral stent (a small tube between the bladder and the inside of the kidney) to provide immediate relief of a blocked kidney. This is especially useful in saving a failing kidney due to swelling and infection from the stone. Ureteral stents vary in length and width but most have the same shape usually called a "double-J or double pigtail". They are designed to allow urine to drain around any stone or obstruction. They can be retained for some length of time as infections recede and as stones are dissolved or fragmented with ESWL or other treatment. The stents will gently dilate or stretch the ureters which can facilitate instrumentation and they will also provide a clear landmark to help surgeons see the stones on x-ray. Most stents can be removed easily during a final office visit. Discomfort levels from stents typically range from minimal associated pain to moderate discomfort.
Prevention
Preventive strategies include dietary modifications and sometimes also taking drugs with the goal of reducing excretory load on the kidneys:[4]
- Drinking enough water to make 2 to 2.5 liters of urine per day.
- A diet low in protein, nitrogen and sodium intake.
- Restriction of oxalate-rich foods and maintenance of an adequate intake of dietary calcium. There is equivocal evidence that calcium supplements increase the risk of stone formation, though calcium citrate appears to carry the lowest, if any, risk.
- Taking drugs such as thiazides, potassium citrate, magnesium citrate and allopurinol, depending on the cause of stone formation.
- Avoidance of cola beverages [5]
For those patients interested in optimizing their kidney stone prevention options, it's essential to have a 24 hour urine test performed. This should be done with the patient on his or her regular diet and activities. The results can then be analyzed for abnormalities and appropriate treatment given.
Diuretics
Although it has been claimed that the diuretic effects of alcohol can result in dehydration, which is important for kidney stone sufferers to avoid, there are no conclusive data demonstrating any cause and effect regarding kidney stones. However, some have theorized that frequent and binge drinkers create situations that set up dehydration, (alcohol consumption, hangovers, and poor sleep and stress habits). In this view, it is not the alcohol that creates a kidney stone but it is the alcohol drinker's associated behavior that sets it up.[6]
One of the recognized medical therapies for prevention of stones is thiazides, a class of drugs usually thought of as diuretics. These drugs prevent stones through an effect independent of their diuretic properties: they reduce urinary calcium excretion. Nonetheless, their diuretic property does not preclude their efficacy as stone preventive. Sodium restriction is necessary for clinical effect of thiazides, as sodium excess promotes calcium excretion. Though some have said that the effect probably fades after two years or so of therapy (tachyphylaxis), in fact it is only randomized controlled trials lasting 2 years or more that show the effect; there is really no good evidence from studies of calcium metabolism that the thiazide effect does not last indefinitely. Thiazides are the medical therapy of choice for most cases of hypercalciuria (excessive urinary calcium) but may not be suitable for all calcium stone formers; just those with high urinary calcium levels.
Allopurinol
Allopurinol (Zyloprim) is another drug with proven benefits in some calcium kidney stone formers. Allopurinol interferes with the liver's production of uric acid. Hyperuricosuria, too much uric acid in the urine, is a risk factor for calcium stones. Allopurinol reduces calcium stone formation in such patients. The drug is also used in patients with gout or hyperuricemia, but hyperuricosuria is not the critical feature of uric acid stones. Uric acid stones are more often caused by low urine pH. Even relatively high uric acid excretion will not be associated with uric acid stone formation if the urine pH is alkaline. Therefore prevention of uric acid stones relies on alkalinization of the urine with citrate. Allopurinol is reserved for patients in whom alkalinization is difficult. For patients with increased uric acid levels and calcium stones, alloprinol is one of the few treatments that has been shown in double-blinded placebo controlled studies to actually reduce kidney stone recurrences. Dosage is adjusted to maintain a reduced urinary excretion of uric acid. Serum uric acid level at or below 6 mg/dL is often the goal of the drug's use in patients with gout or hyperuricemia.
Decreased protein diet
A high protein diet might be partially to blame. Protein from meat and other animal products is broken down into acids, including uric acid. The most available alkaline base to balance the acid from protein is calcium phosphate (hydroxyapatite) from the bones (buffering). The kidney filters the liberated calcium which may then form insoluble crystals (i.e., stones) in urine with available oxalate (partly from metabolic processes, partly from diet) or phosphate ions, depending on conditions. High protein intake is therefore associated with decreased bone density as well as stones. The acid load is associated with decreased urinary citrate excretion; citrate competes with oxalate for calcium and can thereby prevent stones. In addition to increased fluid intake, one of the simplest fixes is to moderate animal protein consumption. However, despite epidemiologic data showing that greater protein intake is associated with more stones, randomized controlled trials of protein restriction have not shown reduced stone prevalence. In this regard, it is not just dietary calcium per se that may cause stone formation, but rather the leaching of bone calcium. Some diseases (e.g., distal renal tubular acidosis) which cause a chronically acidic state also decrease urinary citrate levels; since citrates are normally present as potent inhibitors of stone formation, these patients are prone to frequent stone formation.
Other modifications
Potassium citrate is also used in kidney stone prevention. This is available as both a tablet and liquid preparation. The medication increases urinary pH (makes it more alkaline), as well as increases the urinary citrate level, which helps reduce calcium oxalate crystal aggregation. Optimal 24 hour urine levels of citrate are thought to be over 320 mg/liter of urine or over 600 mg per day. There are urinary dipsticks available that allow patients to monitor and measure urinary pH so patients can optimize their urinary citrate level.
Though caffeine does acutely increase urinary calcium excretion, several independent epidemiologic studies have shown that coffee intake overall is protective for stones.[7]
Measurements of food oxalate content have been difficult and issues remain about the proportion of oxalate that is bio-available, versus a proportion that is not absorbed by the intestine. Oxalate-rich foods are usually restricted to some degree, particularly in patients with high urinary oxalate levels, but no randomized controlled trial of oxalate restriction has been performed to test that hypothesis.
Calgranulin
Crystallization of calcium oxalate (CaOx) appears to be reduced by molecules in the urine that retard the formation, growth, aggregation, and renal cell adherence of calcium oxalate. By purifying urine using salt precipitation, preparative isoelectric focusing, and sizing chromatography, some researchers have found that the molecule calgranulin is able to inhibit calcium oxalate crystal growth.[8] Calgranulin is a protein formed in the kidney.
Given the large amounts of calcium oxalate in the urine, and considering its potency, calgranulin could become an important contribution to the normal urinary inhibition of crystal growth and aggregation. If so, it will be an important tool in the renal defense against kidney stones.
See also
References
- ↑ "USNews.com: Health: Kidney Stone Disease: Overview". Retrieved 2008-01-01.
- ↑ Krambeck AE, Gettman MT, Rohlinger AL, Lohse CM, Patterson DE, Segura JW (2006). "Diabetes mellitus and hypertension associated with shock wave lithotripsy of renal and proximal ureteral stones at 19 years of followup". J Urol. 175 (5): 1742–7. PMID 16600747.
- ↑ Ed Edelson (2006). "Kidney Stone Shock Wave Treatment Boosts Diabetes, Hypertension Risk - Study suggests link, but doctors say it's too early to abandon this therapy". HealthFinder. National Health Information Center.
- ↑ Goldfarb DS, Coe FL (1999, November 15). "Prevention of recurrent nephrolithiasis". Am Fam Physician. 60 (8): 2269–76. PMID 10593318. Check date values in:
|date=(help) - ↑ "nytimes.com: The Claim: Too Much Cola Can Cause Kidney Problems". Retrieved 2008-01-25.
- ↑ Rodman, John, S (May, 1997). "No More Kidney Stones". Prevention. Check date values in:
|date=(help) - ↑ Curhan GC, Willett WC, Rimm EB, Spiegelman D, Stampfer MJ (1996, February 1). "Prospective Study of Beverage Use and the Risk of Kidney Stones". Am Jour Epidemiology. 143 (3): 240–247. PMID 8561157. Check date values in:
|date=(help) - ↑ http://ajprenal.physiology.org/cgi/content/abstract/275/2/F255 Calcim Oxalate crystallization experiment
External links
- Patient Guide To Kidney Stone Diagnosis, Treatment and Prevention. By Dr. R. Ari Rabenou, a kidney stone specialist at the New York University School of Medicine.
- International Kidney Stone Institute
- Pictures of kidney stones, showing their crystalline shape
- Renal calculi
- International Cystinuria Foundation
- Cystinuria Clearinghouse-"Kidney Stone Disease"
- National Kidney and Urologic Diseases Information Clearinghouse
- Patient Experiences with Kidney Stones
- Information on Nephrology & Kidney Disease for Professionals and Patients
- NIH Article
- Kidney stones overview
- Kidney stones
Template:Nephrology
Template:SIB
af:Niersteen ar:حصوة كلوية ca:Litiasi renal da:Nyresten de:Nierenstein hy:Միզաքարային հիվանդություններ id:Batu ginjal ia:Calculo renal he:אבנים בכליות lt:Inkstų akmenligė hu:Vesekövesség nl:Niersteen no:Nyrestein qu:Wasa ruru rumi fi:Virtsakivitauti sv:Njursten yi:ניר שטיין