Hemolytic anemia laboratory findings: Difference between revisions
| Line 32: | Line 32: | ||
====Acanthocytes==== | ====Acanthocytes==== | ||
* Liver disease | * Liver disease | ||
====Thick and thin smear==== | ====Parasitic inclusion==== | ||
=====Thick and thin smear===== | |||
* [[Malaria]] | * [[Malaria]] | ||
* [[Babesiosis]] | * [[Babesiosis]] | ||
* [[Bartonellosis]] | * [[Bartonellosis]] | ||
===Direct antiglobulin test=== | |||
* Direct antiglobulin tests | |||
measures whether there is antibody coating the patient's red blood cells, and is over 95% sensitive in diagnosing immune hemolytic anemia. The test is done by mixing the patient's erythrocytes with anti-human globulin (which contains antibody to IgG and C3). If agglutination occurs, the test is positive and further testing is done to determine whether IgG and/or C3 are coating the red cells (Figure 15). The indirect antiglobulin (indirect Coombs') is done to detect antibodies present in the patient's serum but not coating their red cells. It is helpful for detecting alloantibodies that were introduced by prior transfusion or by fetal transfer of red blood cells to the mother. | |||
==Laboratory Findings== | ==Laboratory Findings== | ||
Revision as of 13:42, 11 October 2012
|
Hemolytic anemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hemolytic anemia laboratory findings On the Web |
|
American Roentgen Ray Society Images of Hemolytic anemia laboratory findings |
|
Risk calculators and risk factors for Hemolytic anemia laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Hemolytic anemia is anemia caused secondary to shortened survival of circulating red blood cells. The normal life span of RBCs is 110 to 120 days. RBC destruction before that time is defined as hemolytic anemia. As opposed to the normal senecence of RBC, the random hemolysis (premature RBC death) is increased in hemolytic anemia.
Approach to diagnosis of hemolytic anemia
Check for presence of hemolysis
- Elevated corrected reticulocyte count will be elevated (>2%), LDH, indirect bilirubin, and low haptoglobin. Haptoglobin is produced in the liver and bind free hemoglobin. During hemolysis, haptoglobin decreases as it is consumed at a faster rate compared to the rate of production by the liver.
Specific findings for intravascular hemolysis
- Urine hemosiderin and urine hemoglobin, and microangiopathic blood smear.
Specific findings for extravascular hemolysis
- Spherocytic red cell morphology
- Negative urine hemosiderin and urine hemoglobin.
Peripheral smear
Findings on peripheral smears can guide towards diagnosis. Some important findings are:
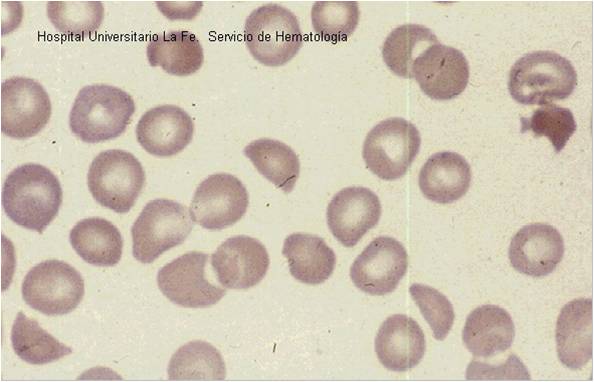
Spherocytes
- Do a direct antiglobulin test
- If antiglobulin negative then diagnosis is hereditary spherocytosis.
- If antiglobulin positive the diagnosis is autoimmune hemolytic anemia.
Sickle cells
Bite cells
- Do G6PD levels
- If G6PD levels decreased then G6PD anemia present. With normal levels diagnosis of unstable hemoglobinopathy should be considered.
Target cell
- Order hemoglobulin electrophoresis.
- Electrophoresis helps to differentiate between thalassemia and liver diseases (elevated liver enzymes), and other hemoglobinopathies.
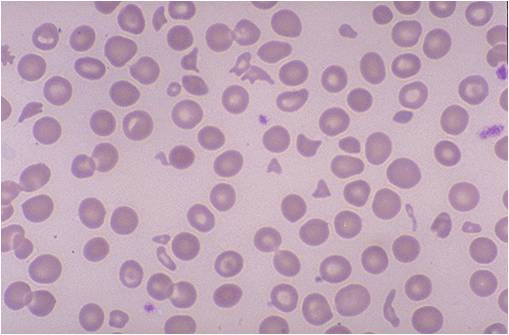
Schistocytes
- HUS-TTP, DIC, Prosthetic heart valve, malignant hypertension
- Other tests to rule out between these diagnosis are platelet, PT, PTT, and creatinine
Acanthocytes
- Liver disease
Parasitic inclusion
Thick and thin smear
Direct antiglobulin test
- Direct antiglobulin tests
measures whether there is antibody coating the patient's red blood cells, and is over 95% sensitive in diagnosing immune hemolytic anemia. The test is done by mixing the patient's erythrocytes with anti-human globulin (which contains antibody to IgG and C3). If agglutination occurs, the test is positive and further testing is done to determine whether IgG and/or C3 are coating the red cells (Figure 15). The indirect antiglobulin (indirect Coombs') is done to detect antibodies present in the patient's serum but not coating their red cells. It is helpful for detecting alloantibodies that were introduced by prior transfusion or by fetal transfer of red blood cells to the mother.
Laboratory Findings
Peripheral blood smear
- Fragments of the red blood cells ("schistocytes") can be present.
- Some red blood cells may appear smaller and rounder than usual (spherocytes).
- Reticulocytes are present in elevated numbers. This may be overlooked if a special stain is not used
- The reticulocytes response act as an important indicator for the severity of the hemolytic anemia. The different methods used to judge the correct response are, absolute reticulocyte count, corrected reticulocyte count, and reticulocyte production index.
Reticulocyte count
Absolute reticulocyte count
The normal values are:
- RBC count - 5 million/microLitre
- Reticulocyte count - 0.5 -1.5 %
- Absolute reticulocyte count - 25,000 to 75,000/microLitre
Reticulocyte production index
- Reticulocytes are newly-produced red blood cells. They are slightly larger than totally mature red blood cells, and have some residual ribosomal RNA. The presence of RNA allows a visible blue stain to bind or, in the case of fluorescent dye, result in a different brightness. This allows them to be detected and counted as a distinct population.
- The Reticulocyte production index (RPI, also called a corrected reticulocyte count) is a calculated value used in the diagnosis of anemia.
- The corrected absolute reticulocyte count = absolute reticulocyte count / reticulocyte maturation time (in days).
- This calculation is necessary because the raw reticulocyte count is misleading in anemic patients.
- The problem arises because the reticulocyte count is not really a count but rather a percentage: it reports the number of reticulocytes as a percentage of the number of red blood cells.
- In anemia, the patient's red blood cells are depleted, creating an erroneously elevated reticulocyte count.
- The idea of the RPI is to assess whether the bone marrow is producing an appropriate response to an anemic state.
- Reticulocyte production should increase in response to any loss of red blood cells.
- It should increase within 2-3 days of a major acute hemorrhage, for instance, and reach its peak in 6-10 days.
- If reticulocyte production is not raised in response to anemia, then the anemia may be due to an acute cause with insufficient time to compensate, or there is a defect with red blood cell production in the bone marrow.
- Marrow defects include nutritional deficiencies (i.e. iron, folate, or B12) or insufficient erythropoietin, the stimulus for red blood cell production.
- Reticulocyte Production Index is calculated as follows:
- The degree of anemia (done by normalizing hematocrit of 45%)
- Reticulocyte maturation time (RMT)
- The Reticulocyte maturation time is 1.0 days for a hematocrit of 45 % to 2.5 days for a hematocrit of 15 %:
- Reticulocyte production index = Reticulocytes % x (HCT / 45) x (1 / RMT)
- The reticulocyte index (RI) should be between 1.0 and 2.0 for a healthy individual.
- RI < 2 with anemia indicates decreased production of reticulocytes and therefore red blood cells.
- RI > 2 with anemia indicates loss of red blood cells (destruction, bleeding, etc) leading to increased compensatory production of reticulocytes to replace the lost red blood cells.
- Value of 45 is usually used as a normal hematocrit.
- So,in a person whose reticulocyte count is 5%, hemoglobin 7.5 g/dL, hematocrit 25%, the RPI would be:
5 x [corrected retic count]/[maturation correction] = 5 x (25/45) /2 = 1.4
Other lab tests
- Elevated lactate dehydrogenase (LDH)
- Elevated haptoglobin
- The direct Coombs test is positive if hemolysis is caused by an immune process
Liver function test
Urinalysis
- Hemosiderin in the urine indicates chronic intravascular hemolysis.
- There is also urobilinogen in the urine.
(Images shown below are courtesy of Melih Aktan MD, Istanbul Medical Faculty - Turkey, and Hospital Universitario La Fe Servicio Hematologia)