Glomerulonephritis
| Glomerulonephritis | |
 | |
|---|---|
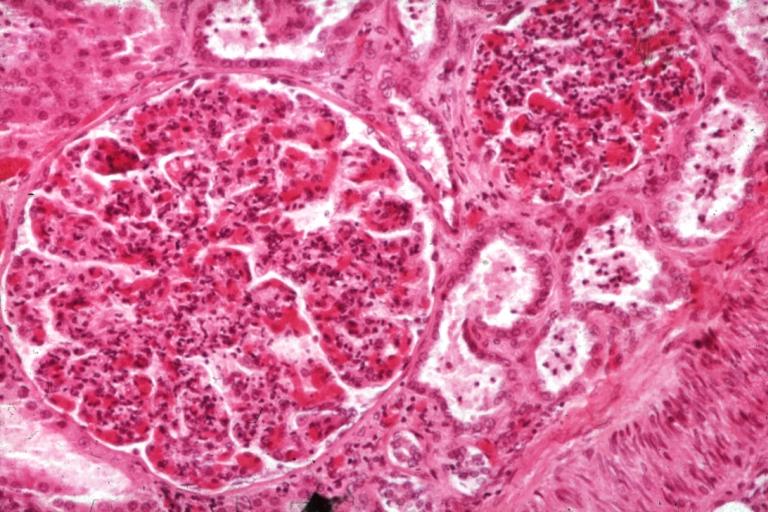
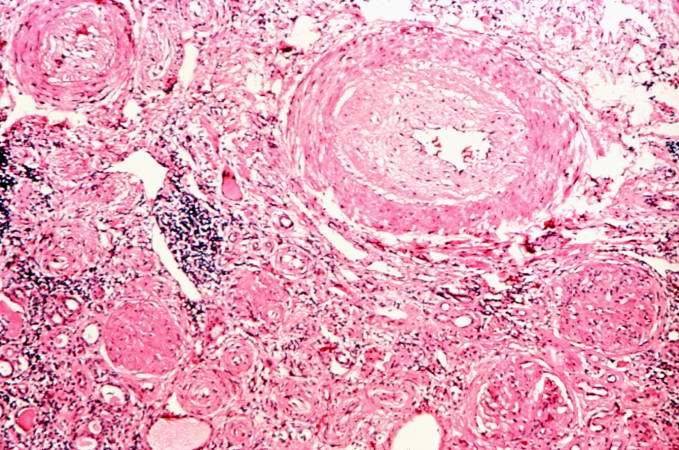
| Acute Glomerulonephritis: Micro H&E high mag; an excellent example of acute exudative glomerulonephritis. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-10 | N00, N01, N03, N18 |
| ICD-9 | 580-582 |
| DiseasesDB | 5245 |
| MeSH | D005921 |
|
Glomerulonephritis Main page |
|
|---|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Synonyms and keywords: GN; glomerular nephritis
Overview
Glomerulonephritis, also known as glomerular nephritis and abbreviated GN', is a primary or secondary immune-mediated renal disease characterized by inflammation of the glomeruli, or small blood vessels in the kidneys. It may present with isolated hematuria and/or proteinuria (blood resp. protein in the urine); or as a nephrotic syndrome, a nephritic syndrome, acute renal failure, or chronic renal failure.
They are categorized into several different pathological patterns, which are broadly grouped into non-proliferative or proliferative types. Diagnosing the pattern of GN is important because the outcome and treatment differs in different types. Primary causes are one which are intrinsic to the kidney, whilst secondary causes are associated with certain infections (bacterial, viral or parasitic pathogens), drugs, systemic disorders (SLE, vasculitis) or cancers.
Proliferative Glomerulonephritis
This type is characterised by increased number of cells in the glomerulus (hypercellular). Usually present as a nephritic syndrome and usually progress to end-stage renal failure (ESRF) over weeks to years (depending on type).
1. IgA disease (Berger's nephropathy)
This is the most common type of glomerulonephritis in adults world-wide. It usually presents as macroscopic haematuria (visibly bloody urine). It occasionally presents as a nephrotic syndrome. It often affects young males after an upper respiratory tract infection. Microscopic examination of biopsy specimens shows increased number of mesangial cells with increased matrix (the 'cement' which holds everything together). Immuno-staining is positive for immunoglobulin A deposits within the matrix. Prognosis is variable, 20% progress to ESRF. Steroids and immunosuppression are not effective treatments for this disease; ACE inhibitors are the mainstay of treatment.
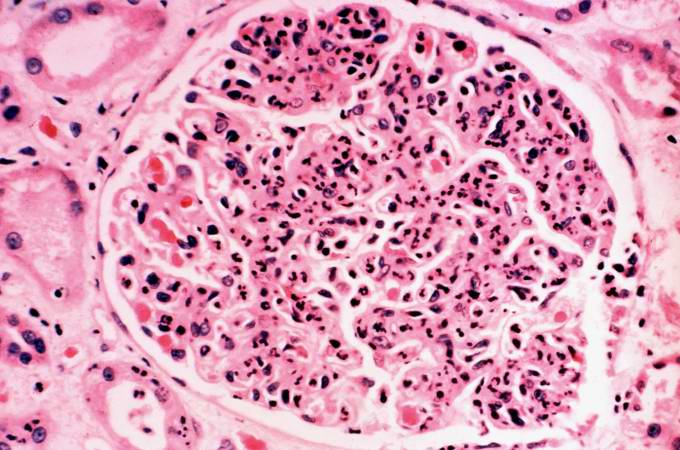
2. Post-infectious Glomerulonephritis
Post-infectious glomerulonephritis occurs after Streptococcal infection - usually of the skin, after a latency of 10 days. This condition is essentially defined as an inflammation of the kidneys. Light microscopy shows diffuse hypercellularity due to proliferation of endothelial and mesangial cells, inflammatory infiltrate with neutrophils and with monocytes. The Bowman space is reduced (compressed), in severe cases might see cresent formation [see later]. However, biopsy is seldom done because the disease usually regresses. Patients present with a nephritic syndrome. Diagnosis is suggested by positive streptococcal titers in the blood (ASOT). Treatment is supportive, and the disease resolves (as a rule) in 2 weeks.
3. Mesangiocapillary Glomerulonephritis
This is primary, or secondary to SLE, viral hepatitis, hypocomplementemia. One sees 'hypercellular and hyperlobular' glomeruli due to proliferation of both cells and the matrix within the mesangium. Presents usually with as a nephrotic syndrome but can be nephritic, with inevitable progression to ESRF.
4. Rapidly progressive Glomerulonephritis (Crescentic GN)
As the name suggests, this type has a poor prognosis, with rapid progression to kidney failure over weeks. Any of the above types of GN can be rapidly progressive. Additionally two further causes present as solely RPGN.
One is Goodpasture's syndrome. This is an autoimmune disease whereby antibodies are directed against antigens found in the kidney and lungs. As well as kidney failure, patient have hemoptysis (cough up blood). High dose immunosupression is required (intravenous methylprednisone) and cyclophosphamide, plus plasmapharesis.
Immunohistochemistry staining of tissue specimens shows linear IgG deposits.
The second cause is vasculitic disorders such as Wegener's and polyarteritis. There is a lack of immune deposits on staining, but blood tests are positive for ANCA antibody.
Histopathology
The majority of glomeruli present "crescents". Formation of crescents is initiated by passage of fibrin into the Bowman space as a result of increased permeability of glomerular basement membrane. Fibrin stimulates the proliferation of parietal cells of Bowman capsule, and an influx of monocytes. Rapid growing and fibrosis of crescents compresses the capillary loops and decreases the Bowman space which leads to renal failure within weeks or months.
-
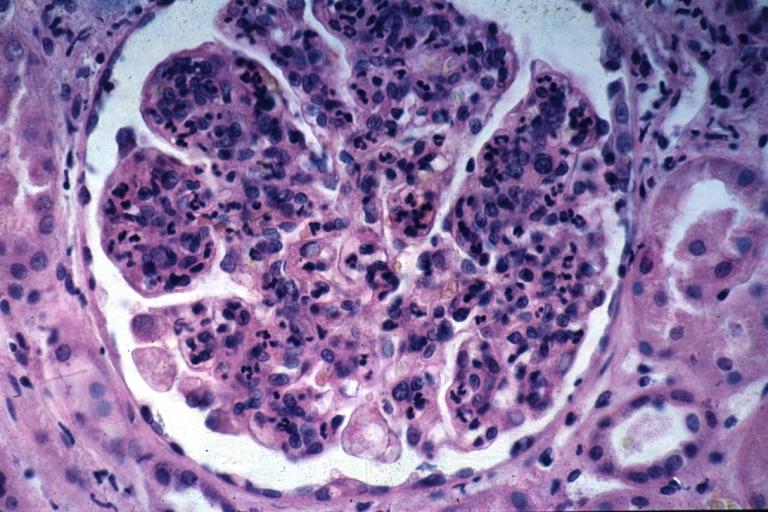
Glomerulonephritis: Micro H&E med mag; an excellent example of AGN with many neutrophils
-
Acute Glomerulonephritis: Micro H&E high mag; an excellent example of acute exudative glomerulonephritis.
Glomerulonephritis Videos
Rapidly progressive glomerulonephritis
{{#ev:youtube|CqSyj4cVZPE}}
Chronic glomerulonephritis
{{#ev:youtube|eA1vYarRAWo}}
Pathological Findings: A Case Example
Clinical Summary
A 17-year-old white male had end-stage renal disease requiring hemodialysis for 10 years. For the previous four years he had hypertension which slowly increased to about 180/120 mm Hg. Laboratory findings included a greatly elevated BUN and creatinine. He was admitted for bilateral nephrectomy and discharged in satisfactory condition on the 10th postoperative day. He was to be contacted in the future for transplantation.
Autopsy Findings
The left (97 grams) and right (88 grams) kidneys were of similar appearance. Cortices were pale, diffusely granular with a few 1-2 mm cysts. On being sectioned, the cortex of each kidney was thin (4-5 mm) and pale. Renal medullae were pale yellow-tan in color and there was abundant peripelvic fat. The ureters, pelvis, calyces and hilar vessels showed no abnormalities.
-
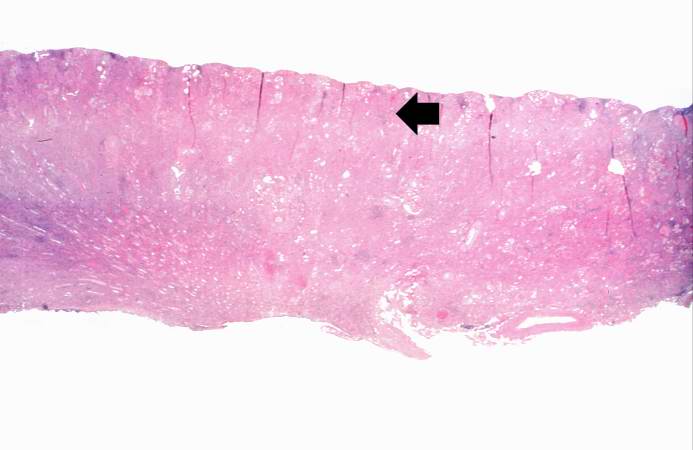
This is a low-power photomicrograph of a saggital section of end stage chronic glomerulonephritis (GN). Note the marked thinning of the cortex (arrow).
-
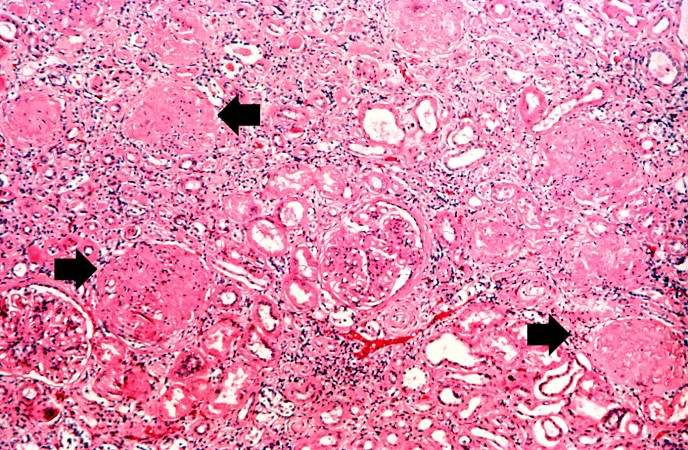
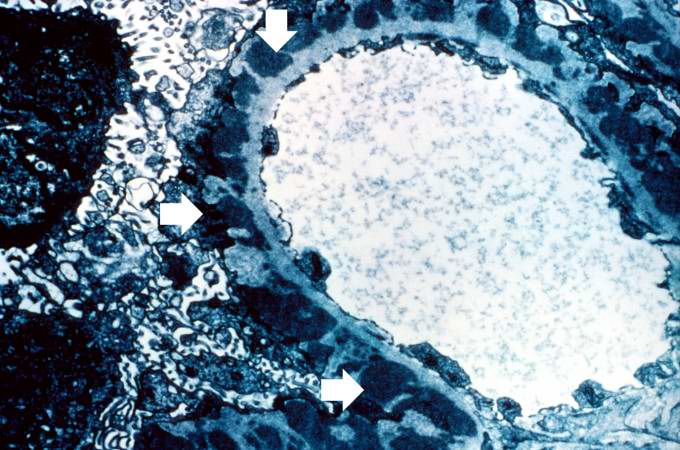
This is a higher-power photomicrograph of hyalinized glomeruli (arrows) and glomeruli with thick basement membranes.
-
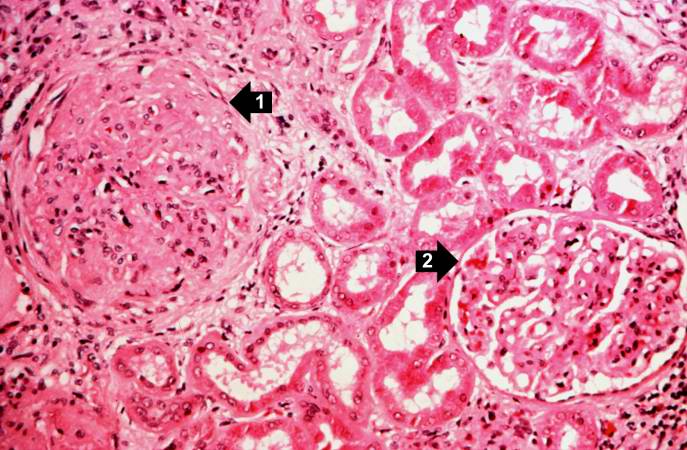
This is a higher-power photomicrograph of hyalinized glomeruli (1) and glomeruli with thickened basement membranes (2).
-
This is a photomicrograph of interstitial and vascular lesions in end stage renal disease.
-
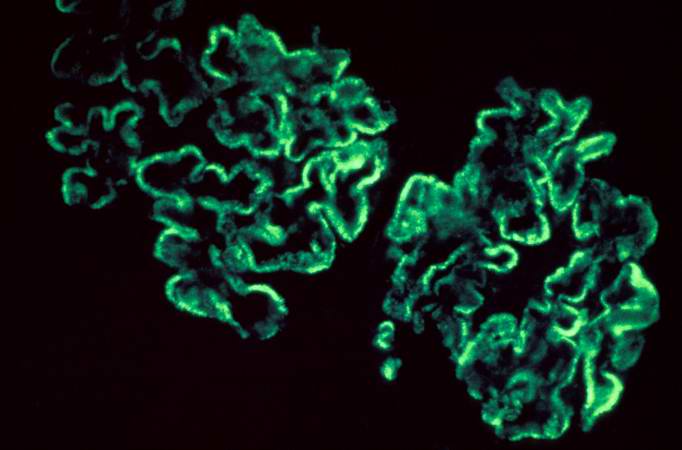
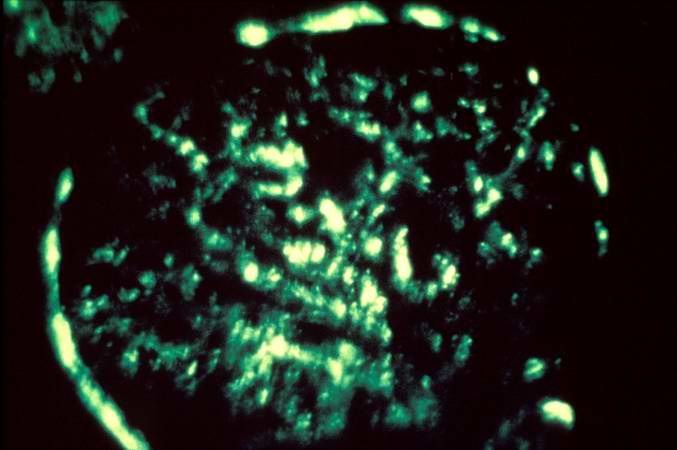
This is an immunofluorescent photomicrograph of granular membranous immunofluorescence (immune complex disease). The antibody used for these studies was specific for IgG.
-
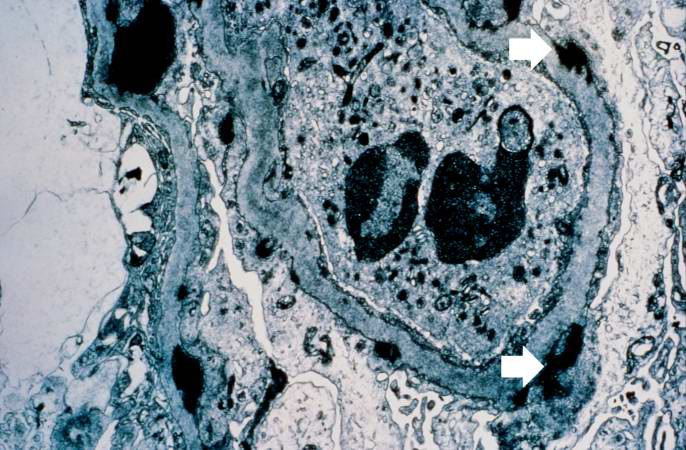
This is an electron micrograph of subepithelial granular electron dense deposits (arrows) which correspond to the granular immunofluorescence seen in the previous image.
-
This is a photomicrograph of a glomerulus from another case with acute poststreptococcal glomerulonephritis. In this case the immune complex glomerular disease is ongoing with necrosis and accumulation of neutrophils in the glomerulus.
-
This immunofluorescent photomicrograph of a glomerulus from a case of acute poststreptococcal glomerulonephritis shows a granular immunofluorescence pattern consistent with immune complex disease. The primary antibody used for this staining was specific for IgG; however antibodies for complement would show a similar pattern.
-
This electron micrograph demonstrates scattered subepithelial dense deposits (arrows) and a polymorphonuclear leukocyte in the lumen.
-
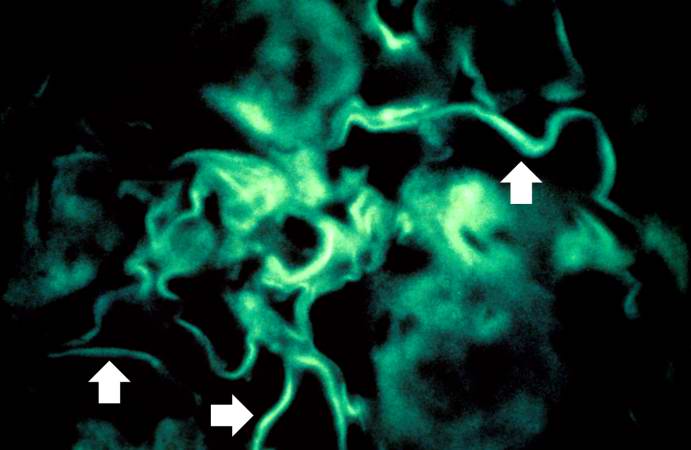
For comparison this is an immunofluorescent photomicrograph of a glomerulus from a patient with Goodpasture's syndrome. The linear (arrows) immunofluorescence is characteristic of Goodpasture's syndrome.
Related chapters
Resources
Images:
HDCN
- HDCN Nephritis Channel - Collection of lectures and links pertaining to glomerulonephritis on the HDCN (Hypertension, Dialysis, and Clinical Nephrology) on-line journal.
- Post-infectious glomerulonephritis - mayoclinic.com.
- Group A Streptococcal Infections - National Institute of Allergy and Infectious Diseases.
References
de:Glomerulonephritis nl:Glomerulonefritis sv:Glomerulonefrit