Deep vein thrombosis history and symptoms
Editor(s)-In-Chief: The APEX Trial Investigators, C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2] ; Kashish Goel, M.D.; Assistant Editor(s)-In-Chief: Justine Cadet
|
Deep Vein Thrombosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Special Scenario |
|
Trials |
|
Case Studies |
|
Deep vein thrombosis history and symptoms On the Web |
|
Risk calculators and risk factors for Deep vein thrombosis history and symptoms |
Overview
A proper history and physical exam is very important for establishing an accurate diagnosis of DVT or VTE. One of the first steps in the management of DVT is the determination of the Wells score for DVT. Out of the 10 clinical questions in the score, 9 can be ascertained solely on the basis of history and physical exam. This underscores the importance of these variables. A high index of suspicion is also necessary to diagnose DVT.
History
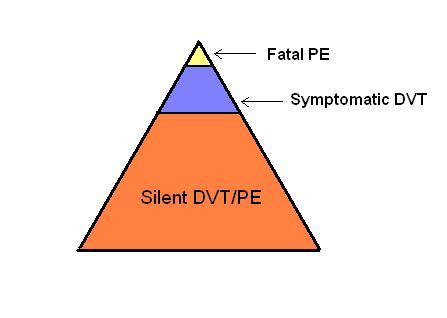
Only 10-20% of VTE is clinically recognized, as depicted by the figure below
Figure :The challenge in diagnosis of VTE
As VTE involves both DVT and PE, the patient can present with complaints of either of the disease.
- With PE, depending upon the severity of the disease, the patient experience
- Shortness of breath
- Loss of Consciousness(in case of massive PE.)
- A smaller PE near the pleura can present with
- While with DVT, patient can complain of
- swelling of lower extremity which can be warm and tender.
In patients having known risk factors, a careful history should be taken. It must include the following:
- History of any recent surgical procedure.
- Use of hormonal contraception, containing estrogen.
- Recent, long-term flying.
- History of a miscarriage (which can be a feature of thrombosis and several other disorders).
- A family history can reveal a hereditary factor in the development of DVT. A positive family history in one or more first-degree relatives under age 50 suggests the presence of a hereditary defect and/or an increased susceptibility for VTE.[1]
-
Front View:Edematous Right Leg
-
Rear View:Left limb edema localized to calf.
-
Front View:Left limb edema localized to calf.
Symptoms
Common Symptoms
The classical symptoms of DVT include:
- Pain in the affected area.
- Swelling of the affected area.
- Erythema around the affected area.
- Dilation of the surface veins and erythema of the overlying area.
However, sometimes there may be no symptoms referable to the location of the DVT.
There are several techniques done during a physical examination which can increase the detection of DVT. Some of these techniques are measuring the circumference of affected limb, measuring the circumference of the contra-lateral limb at a fixed point, and palpating the venous tract, which is often tender. Physical examination is unreliable for excluding the diagnosis of deep vein thrombosis and Homans sign is not recommended for this.
Less Common Symptoms
In phlegmasia alba dolens, the leg is pale and cold with a diminished arterial pulse.
In phlegmasia cerulea dolens, there is an acute and near-total venous occlusion of the entire extremity outflow, including the iliac and femoral veins. The leg is usually painful, cyanosed and edematous.
References
- ↑ Bezemer ID, van der Meer FJ, Eikenboom JC, Rosendaal FR, Doggen CJ (2009). "The value of family history as a risk indicator for venous thrombosis". Arch Intern Med. 169 (6): 610–5. doi:10.1001/archinternmed.2008.589. PMID 19307525.