Deep vein thrombosis diagnostic approach
Editor(s)-In-Chief: The APEX Trial Investigators, C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2] ; Kashish Goel, M.D.; Assistant Editor(s)-In-Chief: Justine Cadet
|
Deep Vein Thrombosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Special Scenario |
|
Trials |
|
Case Studies |
|
Deep vein thrombosis diagnostic approach On the Web |
|
Risk calculators and risk factors for Deep vein thrombosis diagnostic approach |
Overview
Diagnosis Approach
A number of invasive (venography) and non-invasive tests (impedance plethysmography, compression ultrasonography, D-dimer testing) are available for diagnosis. Compression ultrasonography is the noninvasive diagnosis of choice for patients with a first episode of a suspected DVT.
In a patient population with a high prevalence of VTE, a negative D-dimer assay may be insufficient to rule out DVT as a single test, furthermore, not all D-dimer assays are validated for this. However, a D-dimer level <500 ng/mL by ELISA along with a low clinical probability (Wells score)[1] or other negative non-invasive tests may be useful in excluding DVT, without doing ultrasound. Independent studies validate the Wells 10 point rule.[2][3] However, the d-dimer assays vary; for rapid quantitative immunoturbidimetric assays, a cutoff of 1.0 <g/mL is used.[2]
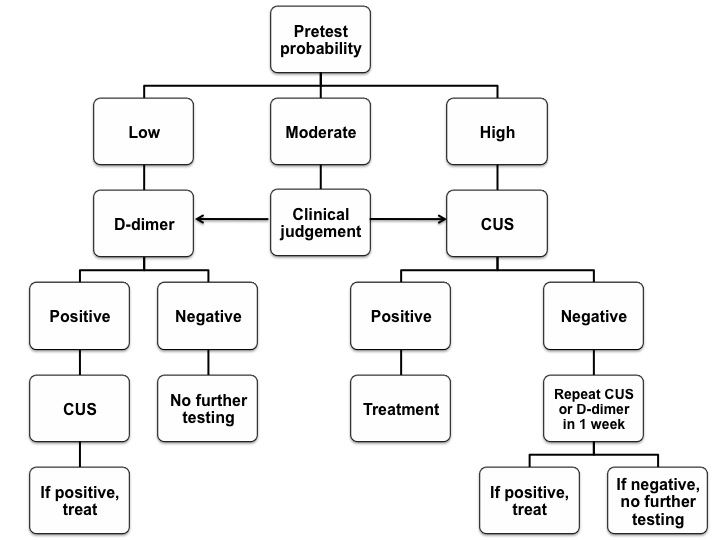
Compression ultrasonography has a positive predictive value of 94 percent (95% CI: 87-98 percent). If the clinical suspicion of DVT is high even after a negative CUS, a repeat study should be done within a week. Complete lower extremity ultrasonography may eliminate the need for repeat testing, but a positive CUS demands user expertise, and requires specialized instrumentation. The algorithm below presents a possible diagnostic approach.
CUS stands for Compression Ultrasonography; D-dimer is the highly sensitive assay. Clinical judgement and local availability should be considered in patients with a moderate probability of DVT. CUS may be preferred in patients with comorbid conditions associated with elevated D-dimer levels.
Adapted from ACCP guidelines[4].
Considerations
- Whole-leg ultrasound may be preferred in those who have severe symptoms of calf DVT or are unable to come for serial testing.
- CT scan venography, MR venography, or MR direct thrombus imaging may be used in those patients in whom ultrasound is not practical (leg cast, excessive edema) or non-diagnostic.
- The diagnostic approach may be modified based on clinical condition of the patient and specific situations.
References
- ↑ Wells PS, Anderson DR, Rodger M, Ginsberg JS, Kearon C, Gent M, Turpie AG, Bormanis J, Weitz J, Chamberlain M, Bowie D, Barnes D, Hirsh J (2000). "Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer". Thromb. Haemost. 83 (3): 416–20. PMID 10744147. Retrieved 2012-05-01. Unknown parameter
|month=ignored (help) - ↑ 2.0 2.1 Linkins LA, Bates SM, Lang E, Kahn SR, Douketis JD, Julian J; et al. (2013). "Selective d-Dimer Testing for Diagnosis of a First Suspected Episode of Deep Venous Thrombosis: A Randomized Trial". Ann Intern Med. 158 (2): 93–100. doi:10.7326/0003-4819-158-2-201301150-00003. PMID 23318311.
- ↑ van der Velde EF, Toll DB, Ten Cate-Hoek AJ, Oudega R, Stoffers HE, Bossuyt PM; et al. (2011). "Comparing the diagnostic performance of 2 clinical decision rules to rule out deep vein thrombosis in primary care patients". Ann Fam Med. 9 (1): 31–6. doi:10.1370/afm.1198. PMID 21242558.
- ↑ Bates SM, Jaeschke R, Stevens SM; et al. (2012). "Diagnosis of DVT: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 Suppl): e351S–418S. doi:10.1378/chest.11-2299. PMID 22315267. Unknown parameter
|month=ignored (help)