Chest pain electrocardiogram: Difference between revisions
Aisha Adigun (talk | contribs) |
No edit summary |
||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
The key findings to look for on EKG is [[ST elevation]] which is characteristic of [[myocardial infarction]]. Diffuse ST elevation may point to the diagnosis of [[pericarditis]]. Serial EKG's should be obtain to evaluate for continued or progression of myocardial injury over time. | The key findings to look for on EKG is [[ST elevation]] which is characteristic of [[myocardial infarction]]. Diffuse ST elevation may point to the [[diagnosis]] of [[pericarditis]]. Serial EKG's should be obtain to evaluate for continued or progression of [[myocardial]] injury over time. | ||
==Electrocardiogram== | ==Electrocardiogram== | ||
*[[Electrocardiogram|An electrocardiogram]] is usually required for initial evaluation of chest pain. | *[[Electrocardiogram|An electrocardiogram]] is usually required for initial evaluation of chest pain. | ||
*It | *It is very useful for the [[diagnosis]] of several etiologies of chest pain such as: | ||
====[[Acute coronary syndromes|Acute coronary syndrome]]==== | ====[[Acute coronary syndromes|Acute coronary syndrome]]==== | ||
*A standard 12 lead ECG is recommended in all patients with chest pain within 10 minutes of presentation if acute coronary syndrome is suspected<ref name="pmid3661390">{{cite journal |vauthors=Slater DK, Hlatky MA, Mark DB, Harrell FE, Pryor DB, Califf RM |title=Outcome in suspected acute myocardial infarction with normal or minimally abnormal admission electrocardiographic findings |journal=Am. J. Cardiol. |volume=60 |issue=10 |pages=766–70 |date=October 1987 |pmid=3661390 |doi=10.1016/0002-9149(87)91020-4 |url=}}</ref><ref name="pmid3920520">{{cite journal |vauthors=Brush JE, Brand DA, Acampora D, Chalmer B, Wackers FJ |title=Use of the initial electrocardiogram to predict in-hospital complications of acute myocardial infarction |journal=N. Engl. J. Med. |volume=312 |issue=18 |pages=1137–41 |date=May 1985 |pmid=3920520 |doi=10.1056/NEJM198505023121801 |url=}}</ref> | *A standard 12 lead [[ECG]] is recommended in all patients with chest pain within 10 minutes of presentation if acute coronary syndrome is suspected. <ref name="pmid3661390">{{cite journal |vauthors=Slater DK, Hlatky MA, Mark DB, Harrell FE, Pryor DB, Califf RM |title=Outcome in suspected acute myocardial infarction with normal or minimally abnormal admission electrocardiographic findings |journal=Am. J. Cardiol. |volume=60 |issue=10 |pages=766–70 |date=October 1987 |pmid=3661390 |doi=10.1016/0002-9149(87)91020-4 |url=}}</ref><ref name="pmid3920520">{{cite journal |vauthors=Brush JE, Brand DA, Acampora D, Chalmer B, Wackers FJ |title=Use of the initial electrocardiogram to predict in-hospital complications of acute myocardial infarction |journal=N. Engl. J. Med. |volume=312 |issue=18 |pages=1137–41 |date=May 1985 |pmid=3920520 |doi=10.1056/NEJM198505023121801 |url=}}</ref> | ||
*Findings on ECG suggestive of ACS include<ref name="pmid3970650">{{cite journal |vauthors=Lee TH, Cook EF, Weisberg M, Sargent RK, Wilson C, Goldman L |title=Acute chest pain in the emergency room. Identification and examination of low-risk patients |journal=Arch. Intern. Med. |volume=145 |issue=1 |pages=65–9 |date=January 1985 |pmid=3970650 |doi= |url=}}</ref><ref name="O'GaraKushner2013">{{cite journal|last1=O'Gara|first1=Patrick T.|last2=Kushner|first2=Frederick G.|last3=Ascheim|first3=Deborah D.|last4=Casey|first4=Donald E.|last5=Chung|first5=Mina K.|last6=de Lemos|first6=James A.|last7=Ettinger|first7=Steven M.|last8=Fang|first8=James C.|last9=Fesmire|first9=Francis M.|last10=Franklin|first10=Barry A.|last11=Granger|first11=Christopher B.|last12=Krumholz|first12=Harlan M.|last13=Linderbaum|first13=Jane A.|last14=Morrow|first14=David A.|last15=Newby|first15=L. Kristin|last16=Ornato|first16=Joseph P.|last17=Ou|first17=Narith|last18=Radford|first18=Martha J.|last19=Tamis-Holland|first19=Jacqueline E.|last20=Tommaso|first20=Carl L.|last21=Tracy|first21=Cynthia M.|last22=Woo|first22=Y. Joseph|last23=Zhao|first23=David X.|title=2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction|journal=Journal of the American College of Cardiology|volume=61|issue=4|year=2013|pages=e78–e140|issn=07351097|doi=10.1016/j.jacc.2012.11.019}}</ref>, [[ST elevation]], [[ST depression]] and a new [[left bundle branch block]] ([[LBBB]]) | *Findings on [[ECG]] suggestive of [[ACS]] include <ref name="pmid3970650">{{cite journal |vauthors=Lee TH, Cook EF, Weisberg M, Sargent RK, Wilson C, Goldman L |title=Acute chest pain in the emergency room. Identification and examination of low-risk patients |journal=Arch. Intern. Med. |volume=145 |issue=1 |pages=65–9 |date=January 1985 |pmid=3970650 |doi= |url=}}</ref><ref name="O'GaraKushner2013">{{cite journal|last1=O'Gara|first1=Patrick T.|last2=Kushner|first2=Frederick G.|last3=Ascheim|first3=Deborah D.|last4=Casey|first4=Donald E.|last5=Chung|first5=Mina K.|last6=de Lemos|first6=James A.|last7=Ettinger|first7=Steven M.|last8=Fang|first8=James C.|last9=Fesmire|first9=Francis M.|last10=Franklin|first10=Barry A.|last11=Granger|first11=Christopher B.|last12=Krumholz|first12=Harlan M.|last13=Linderbaum|first13=Jane A.|last14=Morrow|first14=David A.|last15=Newby|first15=L. Kristin|last16=Ornato|first16=Joseph P.|last17=Ou|first17=Narith|last18=Radford|first18=Martha J.|last19=Tamis-Holland|first19=Jacqueline E.|last20=Tommaso|first20=Carl L.|last21=Tracy|first21=Cynthia M.|last22=Woo|first22=Y. Joseph|last23=Zhao|first23=David X.|title=2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction|journal=Journal of the American College of Cardiology|volume=61|issue=4|year=2013|pages=e78–e140|issn=07351097|doi=10.1016/j.jacc.2012.11.019}}</ref>, [[ST elevation]], [[ST depression]] and a new [[left bundle branch block]] ([[LBBB]]) | ||
*It is important to note that a normal ECG does not rule out the presence of an acute myocardial infarction as ECG can show a hyper-acute [[T wave]]<ref name="pmid11992348">{{cite journal |author=Somers MP, Brady WJ, Perron AD, Mattu A |title=The prominant T wave: electrocardiographic differential diagnosis |journal=Am J Emerg Med |volume=20 |issue=3 |pages=243–51 |year=2002 |month=May |pmid=11992348 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735675702921935}}</ref><ref name="ACS_Clin_NA">Smith SW, Whitwam W. "Acute Coronary Syndromes." ''Emerg Med Clin N Am'' 2006; '''24(1)''': 53-89. PMID 16308113</ref> <ref name="ECG_Noncardiac">"The clinical value of the ECG in noncardiac conditions." ''Chest'' 2004; '''125(4)''': 1561-76. PMID 15078775</ref> as an early presentation. | *It is important to note that a normal [[ECG]] does not rule out the presence of an acute [[myocardial infarction]] as [[ECG]] can show a hyper-acute [[T wave]] <ref name="pmid11992348">{{cite journal |author=Somers MP, Brady WJ, Perron AD, Mattu A |title=The prominant T wave: electrocardiographic differential diagnosis |journal=Am J Emerg Med |volume=20 |issue=3 |pages=243–51 |year=2002 |month=May |pmid=11992348 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0735675702921935}}</ref><ref name="ACS_Clin_NA">Smith SW, Whitwam W. "Acute Coronary Syndromes." ''Emerg Med Clin N Am'' 2006; '''24(1)''': 53-89. PMID 16308113</ref> <ref name="ECG_Noncardiac">"The clinical value of the ECG in noncardiac conditions." ''Chest'' 2004; '''125(4)''': 1561-76. PMID 15078775</ref> as an early presentation. | ||
*If an initial ECG is non-diagnostic and there is still a high clinical suspicion of an MI, a repeat ECG should be conducted. | *If an initial [[ECG]] is non-diagnostic and there is still a high clinical suspicion of an [[MI]], a repeat [[ECG]] should be conducted. | ||
*It is helpful to have precious | *It is helpful to have precious [[ECG]]<nowiki/>s of a [[patient]] to determine if findings observed are new. | ||
Shown below is an EKG demonstrating clear [[ST elevation]] in the right [[precordial lead]]s depicting STEMI. A [[coronary angiography]] revealed a proximal right coronary artery occlusion<ref name="urlST elevation myocardial infarction electrocardiogram - wikidoc">{{cite web |url=https://www.wikidoc.org/index.php/ST_elevation_myocardial_infarction_electrocardiogram |title=ST elevation myocardial infarction electrocardiogram - wikidoc |format= |work= |accessdate=}}</ref> | Shown below is an [[EKG]] demonstrating clear [[ST elevation]] in the right [[precordial lead]]s depicting [[STEMI]]. A [[coronary angiography]] revealed a proximal [[right coronary artery]] occlusion. <ref name="urlST elevation myocardial infarction electrocardiogram - wikidoc">{{cite web |url=https://www.wikidoc.org/index.php/ST_elevation_myocardial_infarction_electrocardiogram |title=ST elevation myocardial infarction electrocardiogram - wikidoc |format= |work= |accessdate=}}</ref> | ||
[[Image:STEMI 20 a.jpg|center|500px]] | [[Image:STEMI 20 a.jpg|center|500px]] | ||
| Line 30: | Line 30: | ||
*ECG findings in patients with [[Pericarditis|pericarditi]]<nowiki/>s may mirror that seen in [[acute myocardial infarction]] and carrying changes may be seen as the disease progresses. | *ECG findings in patients with [[Pericarditis|pericarditi]]<nowiki/>s may mirror that seen in [[acute myocardial infarction]] and carrying changes may be seen as the disease progresses. | ||
*Findings on ECG suggestive of pericarditis at different levels include<ref name="urlPericarditis electrocardiogram - wikidoc">{{cite web |url=https://www.wikidoc.org/index.php/Pericarditis_electrocardiogram |title=Pericarditis electrocardiogram - wikidoc |format= |work= |accessdate=}}</ref> | *Findings on [[ECG]] suggestive of [[pericarditis]] at different levels include: <ref name="urlPericarditis electrocardiogram - wikidoc">{{cite web |url=https://www.wikidoc.org/index.php/Pericarditis_electrocardiogram |title=Pericarditis electrocardiogram - wikidoc |format= |work= |accessdate=}}</ref> | ||
*Stage I: ST elevation in all leads; PTa depression (depression between the end of the [[P wave]] and the beginning of the [[QRS]] complex) | *Stage I: [[ST elevation]] in all leads; PTa depression (depression between the end of the [[P wave]] and the beginning of the [[QRS]] complex) | ||
*Stage II: Pseudonormalization (transition) | *Stage II: Pseudonormalization (transition) | ||
*Stage III: Inverted [[T waves]] | *Stage III: Inverted [[T waves]] | ||
| Line 42: | Line 42: | ||
====[[Aortic dissection|Acute aortic dissection]]==== | ====[[Aortic dissection|Acute aortic dissection]]==== | ||
*ECG may lead to a delay in the diagnosis as some clinicians usually follow the diagnosis of coronary artery disease due to its more common prevalence<ref name="urlAortic dissection electrocardiogram - wikidoc">{{cite web |url=https://www.wikidoc.org/index.php/Aortic_dissection_electrocardiogram |title=Aortic dissection electrocardiogram - wikidoc |format= |work= |accessdate=}}</ref> | *[[ECG]] may lead to a delay in the [[diagnosis]] as some clinicians usually follow the [[diagnosis]] of [[Coronary heart disease|coronary artery disease]] due to its more common prevalence. <ref name="urlAortic dissection electrocardiogram - wikidoc">{{cite web |url=https://www.wikidoc.org/index.php/Aortic_dissection_electrocardiogram |title=Aortic dissection electrocardiogram - wikidoc |format= |work= |accessdate=}}</ref> | ||
*EKG findings in aortic dissection are usually non-specific. Possible findings include:<ref name="urlAortic dissection electrocardiogram - wikidoc">{{cite web |url=https://www.wikidoc.org/index.php/Aortic_dissection_electrocardiogram |title=Aortic dissection electrocardiogram - wikidoc |format= |work= |accessdate=}}</ref><ref name="EvangelistaIsselbacher2018">{{cite journal|last1=Evangelista|first1=Arturo|last2=Isselbacher|first2=Eric M.|last3=Bossone|first3=Eduardo|last4=Gleason|first4=Thomas G.|last5=Eusanio|first5=Marco Di|last6=Sechtem|first6=Udo|last7=Ehrlich|first7=Marek P.|last8=Trimarchi|first8=Santi|last9=Braverman|first9=Alan C.|last10=Myrmel|first10=Truls|last11=Harris|first11=Kevin M.|last12=Hutchinson|first12=Stuart|last13=O’Gara|first13=Patrick|last14=Suzuki|first14=Toru|last15=Nienaber|first15=Christoph A.|last16=Eagle|first16=Kim A.|title=Insights From the International Registry of Acute Aortic Dissection|journal=Circulation|volume=137|issue=17|year=2018|pages=1846–1860|issn=0009-7322|doi=10.1161/CIRCULATIONAHA.117.031264}}</ref><ref name="HirataWake2010">{{cite journal|last1=Hirata|first1=Kazuhito|last2=Wake|first2=Minoru|last3=Kyushima|first3=Masahiro|last4=Takahashi|first4=Takanori|last5=Nakazato|first5=Jun|last6=Mototake|first6=Hidemitsu|last7=Tengan|first7=Toshiho|last8=Yasumoto|first8=Hiroshi|last9=Henzan|first9=Eisei|last10=Maeshiro|first10=Masao|last11=Asato|first11=Hiroaki|title=Electrocardiographic changes in patients with type A acute aortic dissection|journal=Journal of Cardiology|volume=56|issue=2|year=2010|pages=147–153|issn=09145087|doi=10.1016/j.jjcc.2010.03.007}}</ref> | *[[EKG]] findings in [[aortic dissection]] are usually non-specific. Possible findings include: <ref name="urlAortic dissection electrocardiogram - wikidoc">{{cite web |url=https://www.wikidoc.org/index.php/Aortic_dissection_electrocardiogram |title=Aortic dissection electrocardiogram - wikidoc |format= |work= |accessdate=}}</ref><ref name="EvangelistaIsselbacher2018">{{cite journal|last1=Evangelista|first1=Arturo|last2=Isselbacher|first2=Eric M.|last3=Bossone|first3=Eduardo|last4=Gleason|first4=Thomas G.|last5=Eusanio|first5=Marco Di|last6=Sechtem|first6=Udo|last7=Ehrlich|first7=Marek P.|last8=Trimarchi|first8=Santi|last9=Braverman|first9=Alan C.|last10=Myrmel|first10=Truls|last11=Harris|first11=Kevin M.|last12=Hutchinson|first12=Stuart|last13=O’Gara|first13=Patrick|last14=Suzuki|first14=Toru|last15=Nienaber|first15=Christoph A.|last16=Eagle|first16=Kim A.|title=Insights From the International Registry of Acute Aortic Dissection|journal=Circulation|volume=137|issue=17|year=2018|pages=1846–1860|issn=0009-7322|doi=10.1161/CIRCULATIONAHA.117.031264}}</ref><ref name="HirataWake2010">{{cite journal|last1=Hirata|first1=Kazuhito|last2=Wake|first2=Minoru|last3=Kyushima|first3=Masahiro|last4=Takahashi|first4=Takanori|last5=Nakazato|first5=Jun|last6=Mototake|first6=Hidemitsu|last7=Tengan|first7=Toshiho|last8=Yasumoto|first8=Hiroshi|last9=Henzan|first9=Eisei|last10=Maeshiro|first10=Masao|last11=Asato|first11=Hiroaki|title=Electrocardiographic changes in patients with type A acute aortic dissection|journal=Journal of Cardiology|volume=56|issue=2|year=2010|pages=147–153|issn=09145087|doi=10.1016/j.jjcc.2010.03.007}}</ref> | ||
Non-specific ST-segment changes | * Non-specific ST-segment changes | ||
Atrioventricular block (second degree) | * [[Second degree AV block|Atrioventricular block]] (second degree) | ||
Left ventricular hypertrophy | * [[Left ventricular hypertrophy]] | ||
Sinus bradycardia | * [[Sinus bradycardia]] | ||
Revision as of 03:22, 11 February 2021
|
Chest pain Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Chest pain electrocardiogram On the Web |
|
Risk calculators and risk factors for Chest pain electrocardiogram |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Aisha Adigun, B.Sc., M.D.[2]
Overview
The key findings to look for on EKG is ST elevation which is characteristic of myocardial infarction. Diffuse ST elevation may point to the diagnosis of pericarditis. Serial EKG's should be obtain to evaluate for continued or progression of myocardial injury over time.
Electrocardiogram
- An electrocardiogram is usually required for initial evaluation of chest pain.
- It is very useful for the diagnosis of several etiologies of chest pain such as:
Acute coronary syndrome
- A standard 12 lead ECG is recommended in all patients with chest pain within 10 minutes of presentation if acute coronary syndrome is suspected. [1][2]
- Findings on ECG suggestive of ACS include [3][4], ST elevation, ST depression and a new left bundle branch block (LBBB)
- It is important to note that a normal ECG does not rule out the presence of an acute myocardial infarction as ECG can show a hyper-acute T wave [5][6] [7] as an early presentation.
- If an initial ECG is non-diagnostic and there is still a high clinical suspicion of an MI, a repeat ECG should be conducted.
- It is helpful to have precious ECGs of a patient to determine if findings observed are new.
Shown below is an EKG demonstrating clear ST elevation in the right precordial leads depicting STEMI. A coronary angiography revealed a proximal right coronary artery occlusion. [8]
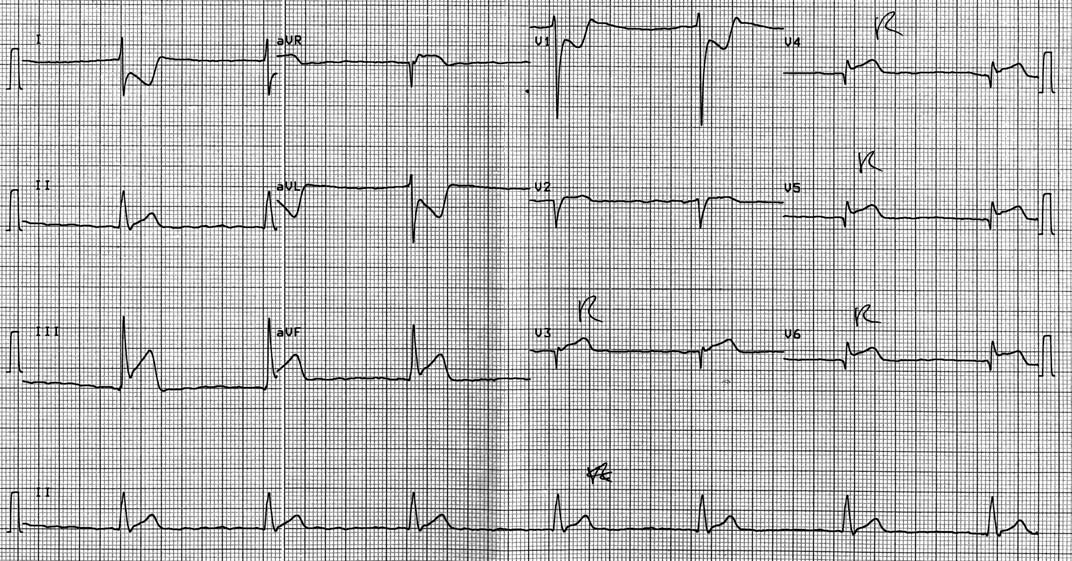
Copyleft image obtained courtesy of, http://en.ecgpedia.org/wiki/Main_Page
For more EKG examples of ST elevation myocardial infarction click here
Pericarditis
- ECG findings in patients with pericarditis may mirror that seen in acute myocardial infarction and carrying changes may be seen as the disease progresses.
- Findings on ECG suggestive of pericarditis at different levels include: [9]
- Stage I: ST elevation in all leads; PTa depression (depression between the end of the P wave and the beginning of the QRS complex)
- Stage II: Pseudonormalization (transition)
- Stage III: Inverted T waves
- Stage IV: Normalization
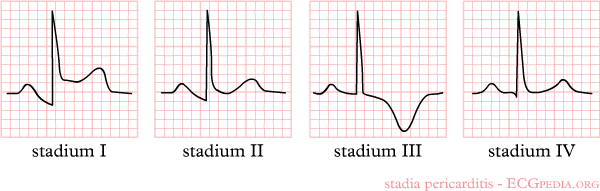
Copyleft image obtained courtesy of, http://en.ecgpedia.org/wiki/Main_Page
Acute aortic dissection
- ECG may lead to a delay in the diagnosis as some clinicians usually follow the diagnosis of coronary artery disease due to its more common prevalence. [10]
- EKG findings in aortic dissection are usually non-specific. Possible findings include: [10][11][12]
- Non-specific ST-segment changes
- Atrioventricular block (second degree)
- Left ventricular hypertrophy
- Sinus bradycardia
References
- ↑ Slater DK, Hlatky MA, Mark DB, Harrell FE, Pryor DB, Califf RM (October 1987). "Outcome in suspected acute myocardial infarction with normal or minimally abnormal admission electrocardiographic findings". Am. J. Cardiol. 60 (10): 766–70. doi:10.1016/0002-9149(87)91020-4. PMID 3661390.
- ↑ Brush JE, Brand DA, Acampora D, Chalmer B, Wackers FJ (May 1985). "Use of the initial electrocardiogram to predict in-hospital complications of acute myocardial infarction". N. Engl. J. Med. 312 (18): 1137–41. doi:10.1056/NEJM198505023121801. PMID 3920520.
- ↑ Lee TH, Cook EF, Weisberg M, Sargent RK, Wilson C, Goldman L (January 1985). "Acute chest pain in the emergency room. Identification and examination of low-risk patients". Arch. Intern. Med. 145 (1): 65–9. PMID 3970650.
- ↑ O'Gara, Patrick T.; Kushner, Frederick G.; Ascheim, Deborah D.; Casey, Donald E.; Chung, Mina K.; de Lemos, James A.; Ettinger, Steven M.; Fang, James C.; Fesmire, Francis M.; Franklin, Barry A.; Granger, Christopher B.; Krumholz, Harlan M.; Linderbaum, Jane A.; Morrow, David A.; Newby, L. Kristin; Ornato, Joseph P.; Ou, Narith; Radford, Martha J.; Tamis-Holland, Jacqueline E.; Tommaso, Carl L.; Tracy, Cynthia M.; Woo, Y. Joseph; Zhao, David X. (2013). "2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction". Journal of the American College of Cardiology. 61 (4): e78–e140. doi:10.1016/j.jacc.2012.11.019. ISSN 0735-1097.
- ↑ Somers MP, Brady WJ, Perron AD, Mattu A (2002). "The prominant T wave: electrocardiographic differential diagnosis". Am J Emerg Med. 20 (3): 243–51. PMID 11992348. Unknown parameter
|month=ignored (help) - ↑ Smith SW, Whitwam W. "Acute Coronary Syndromes." Emerg Med Clin N Am 2006; 24(1): 53-89. PMID 16308113
- ↑ "The clinical value of the ECG in noncardiac conditions." Chest 2004; 125(4): 1561-76. PMID 15078775
- ↑ "ST elevation myocardial infarction electrocardiogram - wikidoc".
- ↑ "Pericarditis electrocardiogram - wikidoc".
- ↑ 10.0 10.1 "Aortic dissection electrocardiogram - wikidoc".
- ↑ Evangelista, Arturo; Isselbacher, Eric M.; Bossone, Eduardo; Gleason, Thomas G.; Eusanio, Marco Di; Sechtem, Udo; Ehrlich, Marek P.; Trimarchi, Santi; Braverman, Alan C.; Myrmel, Truls; Harris, Kevin M.; Hutchinson, Stuart; O’Gara, Patrick; Suzuki, Toru; Nienaber, Christoph A.; Eagle, Kim A. (2018). "Insights From the International Registry of Acute Aortic Dissection". Circulation. 137 (17): 1846–1860. doi:10.1161/CIRCULATIONAHA.117.031264. ISSN 0009-7322.
- ↑ Hirata, Kazuhito; Wake, Minoru; Kyushima, Masahiro; Takahashi, Takanori; Nakazato, Jun; Mototake, Hidemitsu; Tengan, Toshiho; Yasumoto, Hiroshi; Henzan, Eisei; Maeshiro, Masao; Asato, Hiroaki (2010). "Electrocardiographic changes in patients with type A acute aortic dissection". Journal of Cardiology. 56 (2): 147–153. doi:10.1016/j.jjcc.2010.03.007. ISSN 0914-5087.