Breast cancer screening
|
Breast Cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Breast cancer screening On the Web |
|
American Roentgen Ray Society Images of Breast cancer screening |
|
Risk calculators and risk factors for Breast cancer screening |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Jack Khouri
Overview
Breast cancer screening is an attempt to find unsuspected cancers. The most common screening methods include: self and clinical breast exams, x-ray mammography, breast magnetic resonance imaging (MRI), ultrasound, and genetic testing.
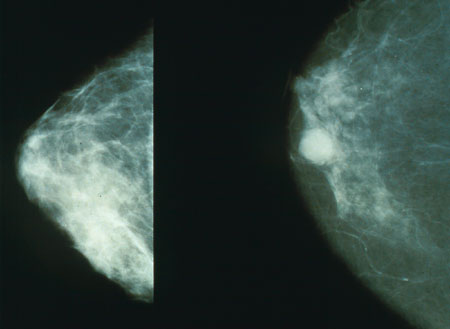
X-Ray Mammography
Mammography is still the modality of choice for screening of early breast cancer, since it is relatively fast, reasonably accurate, and widely available in developed countries. Breast cancers detected by mammography are usually much smaller (earlier stage) than those detected by patients or doctors as a breast lump.
Due to the high incidence of breast cancer among older women, screening is now recommended in many countries. Recommended screening methods include breast self-examination and mammography. Mammography has been estimated to reduce breast cancer-related mortality by 20-30%.[1] Routine (annual) mammography of women older than age 40 or 50 is recommended by numerous organizations as a screening method to diagnose early breast cancer and has demonstrated a protective effect in multiple clinical trials.[2] The evidence in favor of mammographic screening comes from eight randomized clinical trials from the 1960s through 1980s. Many of these trials have been criticised for methodological errors, and the results were summarized in a review article published in 1993.[3]
Improvements in mortality due to screening are hard to measure; similar difficulty exists in measuring the impact of Pap smear testing on cervical cancer, though worldwide, the impact of that test is likely enormous. Nationwide mortality due to cancer before and after the institution of a screening test is a surrogate indicator about the effectiveness of screening, and results of mammography are favorable.
The U.S. National Cancer Institute recommends screening mammography every one to two years beginning at age 40.[4] In the UK, women are invited for screening once every three years beginning at age 50. Women with one or more first-degree relatives (mother, sister, daughter) with premenopausal breast cancer should begin screening at an earlier age. It is usually suggested to start screening at an age that is 10 years less than the age at which the relative was diagnosed with breast cancer.
A clinical practice guideline by the US Preventive Services Task Force recommended "screening mammography, with or without clinical breast examination (CBE), every 1 to 2 years for women aged 40 and older."[5] The Task Force gave a grade B recommendation.
Criticisms of Screening Mammography
Several scientific groups however have expressed concern about the public's perceptions of the benefits of breast screening.[6] In 2001, a controversial review published in The Lancet claimed that there is no reliable evidence that screening for breast cancer reduces mortality.[7] The results of this study were widely reported in the popular press.[8]
False positives are a major problem of mammographic breast cancer screening. Data reported in the UK Million Woman Study indicates that if 134 mammograms are performed, 20 women will be called back for suspicious findings, and four biopsies will be necessary, to diagnose one cancer. Recall rates are higher in the U.S. than in the UK.[9] The contribution of mammography to the early diagnosis of cancer is controversial, and for those found with benign lesions, mammography can create a high psychological and financial cost.
Mammography in Women Less than 50 Years Old
Part of the difficulty in interpreting mammograms in younger women stems from the problem of breast density. Radiographically, a dense breast has a preponderance of glandular tissue, and younger age or estrogen hormone replacement therapy contribute to mammographic breast density. After menopause, the breast glandular tissue gradually is replaced by fatty tissue, making mammographic interpretation much more accurate. Some authors speculate that part of the contribution of estrogen hormone replacement therapy to breast cancer mortality arises from the issue of increased mammographic breast density. Breast density is an independent adverse prognostic factor on breast cancer prognosis.
A systematic review by the American College of Physicians concluded "Although few women 50 years of age or older have risks from mammography that outweigh the benefits, the evidence suggests that more women 40 to 49 years of age have such risks".[10]
Enhancements to Mammography
In general, digital mammography and computer-aided mammography have increased the sensitivity of mammograms, but at the cost of more numerous false positive results.
Computer-aided diagnosis(CAD) Systems may help radiologists to evaluate X-ray images to detect breast cancer in an early stage.[citation needed] CAD is especially established in US and the Netherlands. It is used in addition to the human evaluation of the diagnostician.
Digital Mammography
Overview
In digital mammography, the processes of image acquisition, display, and storage are separated, which allows optimization of each. Radiation transmitted through the breast is absorbed by an electronic detector, the response of which is faithful over a wide range of intensities. Once this information is recorded, it can be displayed by using computer image-processing techniques to allow arbitrary settings of image brightness and contrast, without the need for further exposure to the patient.[11] Several approaches have been taken in the development of digital mammography systems: (a) slot scanning with a scintillator and a charge-coupled device (CCD) array, (b) a flat-panel scintillator and an amorphous silicon diode array, (c) a flat-panel amorphous selenium array, (d) a tiled scintillator with fiberoptic tapers and a CCD array, and (e) photostimulable phosphor plates (computed radiography).[12]
Advantages
- Better contrast resolution for dense breasts
- reduction in recall rates
- potential for reduction in radiation dose
- increased patient throughput, postprocessing capability, and digital acquisition
As mentioned above, a film mammography's sensitivity for detecting breast cancer in women with radiographically dense breast tissue is limited. A study, which was published in the New England Journal of Medicine, aimed at assessing the role of digital mammography in screening for breast cancer in women with dense breasts. The study concluded that the overall diagnostic accuracy of digital and film mammography as a means of screening for breast cancer is similar, but digital mammography is more accurate in women under the age of 50 years, women with radiographically dense breasts, and premenopausal or perimenopausal women.[13]
Breast MRI
Magnetic resonance imaging (MRI) has been shown to detect cancers not visible on mammograms, but has long been regarded to have disadvantages. For example, although it is 27-36% more sensitive, it is less specific than mammography.[14] As a result, MRI studies will have more false positives (up to 5%), which may have undesirable financial and psychological costs. It is also a relatively expensive procedure, and one which requires the intravenous injection of a chemical agent to be effective. Proposed indications for using MRI for screening include:[15]
- Strong family history of breast cancer
- Patients with BRCA-1 or BRCA-2 oncogene mutations
- Evaluation of women with breast implants
- History of previous lumpectomy or breast biopsy surgeries
- Axillary metastasis with an unknown primary tumor
- Very dense or scarred breast tissue
However, two studies published in 2007 demonstrated the strengths of MRI-based screening:
- In March 2007, an article published in the New England Journal of Medicine demonstrated that in 3.1% of patients with breast cancer, whose contralateral breast was clinically and mammographically tumor-free, MRI could detect breast cancer. Sensitivity for detection of breast cancer in this study was 91%, specificity 88%.[16]
- In August 2007, an article published in The Lancet compared MRI breast cancer screening to conventional mammographic screening in 7,319 women. MRI screening was highly more sensitive (97% in the MRI group vs. 56% in the mammography group) in recognizing early high-grade Ductal Carcinoma in situ (DCIS), the most important precursor of invasive carcinoma. Despite the high sensitivity, MRI screening had a positive predictive value of 52%, which is totally accepted for cancer screening tests.[17] The author of a comment published in the same issue of The Lancet concludes that "MRI outperforms mammography in tumour detection and diagnosis."[18]
The American Cancer Society Guidelines for Breast Cancer Screening with MRI as an Adjunct to Mammography
According to the American Cancer Society guidelines, screening MRI is recommended for:[19]
- Women with a strong family history of breast and ovarian cancer
- Carriers of the BRCA mutation
- Women with a history of chest radiation between the ages of 10 and 30 years for Hodgkin disease
- Women with a lifetime risk greater than 20% to 25% as defined by risk predication models dependent on family history
There are several risk subgroups for which the available data are insufficient to recommend for or against screening, including women with a personal history of breast cancer, carcinoma in situ, atypical hyperplasia, and extremely dense breasts on mammography.
Breast Ultrasound
Ultrasound alone is not usually employed as a screening tool but it is a useful additional tool for the characterization of palpable tumours and directing image-guided biopsies. U-Systems is a US-based company that is selling a breast-cancer detection system using ultrasound that is fully-automated. Using an ultrasound allows a look at dense breast tissue which is not possible with digital mammmography. It is closely correlated with the digital mammography. The other significant advantage over digital mammography is that it is a pain-free procedure.
Breast Self-Exam
Breast self-examination was widely discussed in the 1990s as a useful modality for detecting breast cancer at an earlier stage of presentation. A large clinical trial in China reduced enthusiasm for breast self-exam. In the trial, reported in the Journal of the National Cancer Institute first in 1997 and updated in 2002, 132,979 female Chinese factory workers were taught by nurses at their factories to perform monthly breast self-exam, while 133,085 other workers were not taught self-exam. The women taught self-exam tended to detect more breast nodules, but their breast cancer mortality rate was no different from that of women in the control group. In other words, women taught breast self-exam were mostly likely to detect benign breast disease, but were just as likely to die of breast cancer.[20] An editorial in the Journal of the National Cancer Institute reported in 2002, "Routinely Teaching Breast Self-Examination is Dead. What Does This Mean?"[21]
BRCA Testing
Approach to Genetic Testing
Assess women with:
❑ No previous diagnosis with BRCA related cancer, and ❑ Absence of signs and symptoms of any BRCA related cancer | |||||
Risk assessment: is ANY of the following history factors present? ❑ Family members with breast, ovarian, tubal or peritoneal cancer | |||||
Yes? | |||||
Screening with ANY of the following:
❑ Ontario Family History Assessment Tool | |||||
High risk of potentially harmful BRCA mutation based on screening? | |||||
Genetic counseling
❑ Risk assessment for presence of potential BRCA mutation ❑ Educating patients about the possible genetic testing results ❑ Risk assessment of family members to identify suitable candidates for genetic testing ❑ Discussion about risk reducing interventions ❑ Post-test counseling | |||||
BRCA mutation genetic testing | |||||
Algorithm based on the 2013 US Preventive Services Task Force recommendation statement.[22]
Screening Guidelines
| Organisation | Year of the Issued Guidelines | Mammography | Clinical Breast Examination | Breast Self-Examination | Imaging |
| USPSTF | 2009 | Age 50-74 years: every 2 years Age 40-49 or >75: individualize decision (every 2 years if performed) |
Insufficient evidence for recommendation | Not recommended | Insufficient evidence for recommendation |
| American Cancer Society | 2010 | Age >40 years: annually | Age 20-39 years: every 3 years age >40 years: annually |
Optional | MRI annually in high risk women (20% lifetime risk of breast cancer, positive BRCA mutations, history of radiation therapy) |
| American College of Obstetricians and Gynecologists | 2011 | Age >40 years: annually | Age 20-39 years: every 3 years >40 years: annually |
Encouraged | Not recommended |
Risk Assessment, Genetic Counseling, and Genetic Testing for BRCA-Related Cancer in Women: U.S. Preventive Services Task Force Recommendation Statement (DO NOT EDIT)[22]
Clinical Summary of U.S. Preventive Services Task Force Recommendation
| "1. Screen women whose family history may be associated with an increased risk for potentially harmful BRCA mutations. Women with positive screening results should receive genetic counseling and, if indicated after counseling, BRCA testing. (Grade B)" |
| "1. Do not routinely recommend genetic counseling or BRCA testing to women whose family history is not associated with an increased risk for potentially harmful BRCA mutations. (Grade D)" |
References
- ↑ Elwood J, Cox B, Richardson A. "The effectiveness of breast cancer screening by mammography in younger women". Online J Curr Clin Trials. Doc No 32: [23, 227 words, 195 paragraphs]. PMID 8305999.
- ↑ Fletcher S, Black W, Harris R, Rimer B, Shapiro S (1993). "Report of the International Workshop on Screening for Breast Cancer". J Natl Cancer Inst. 85 (20): 1644–56. PMID 8105098.
- ↑ Fletcher SW, Black W, Harris R, Rimer BK, Shapiro S (1993). "Report of the International Workshop on Screening for Breast Cancer". J. Natl. Cancer Inst. 85 (20): 1644–56. PMID 8105098.
|access-date=requires|url=(help) - ↑ "NCI Statement on Mammography Screening - National Cancer Institute". Retrieved 2007-09-11.
- ↑ "Screening for breast cancer: recommendations and rationale". Ann. Intern. Med. 137 (5 Part 1): 344–6. 2002. PMID 12204019.
- ↑ "Women 'misjudge screening benefits'". BBC. Monday, 15 October, 2001. Retrieved 2007-04-04. Check date values in:
|date=(help) - ↑ Olsen O, Gøtzsche P (2001). "Cochrane review on screening for breast cancer with mammography". Lancet. 358 (9290): 1340–2. PMID 11684218.
- ↑ "New concerns over breast screening". BBC. Thursday, 18 October, 2001. Retrieved 2007-04-04. Check date values in:
|date=(help) - ↑ Smith-Bindman R, Ballard-Barbash R, Miglioretti DL, Patnick J, Kerlikowske K (2005). "Comparing the performance of mammography screening in the USA and the UK". Journal of medical screening. 12 (1): 50–4. doi:10.1258/0969141053279130. PMID 15814020.
- ↑ Armstrong K, Moye E, Williams S, Berlin JA, Reynolds EE (2007). "Screening mammography in women 40 to 49 years of age: a systematic review for the American College of Physicians". Ann. Intern. Med. 146 (7): 516–26. PMID 17404354.
- ↑ Pisano ED, Yaffe MJ (2005) Digital mammography. Radiology 234 (2):353-62. DOI:10.1148/radiol.2342030897 PMID: 15670993
- ↑ 12.0 12.1 Mahesh M (2004). "AAPM/RSNA physics tutorial for residents: digital mammography: an overview". Radiographics : a Review Publication of the Radiological Society of North America, Inc. 24 (6): 1747–60. doi:10.1148/rg.246045102. PMID 15537982. Retrieved 2011-12-02.
- ↑ Pisano ED, Gatsonis C, Hendrick E, Yaffe M, Baum JK, Acharyya S et al. (2005) Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med 353 (17):1773-83. DOI:10.1056/NEJMoa052911 PMID: 16169887
- ↑ Hrung J, Sonnad S, Schwartz J, Langlotz C (1999). "Accuracy of MR imaging in the work-up of suspicious breast lesions: a diagnostic meta-analysis". Acad Radiol. 6 (7): 387–97. PMID 10410164.
- ↑ Morrow M (2004). "Magnetic resonance imaging in breast cancer: one step forward, two steps back?". JAMA. 292 (22): 2779–80. PMID 15585740.
- ↑ Lehman CD, Gatsonis C, Kuhl CK, Hendrick RE, Pisano ED, Hanna L, Peacock S, Smazal SF, Maki DD, Julian TB, DePeri ER, Bluemke DA, Schnall MD (2007). "MRI evaluation of the contralateral breast in women with recently diagnosed breast cancer". N Engl J Med. 356 (13): 1295–1303. PMID 17392300.
- ↑ Kuhl CK, Schrading S, Bieling HB, Wardelmann E, Leutner CC, Koenig R, Kuhn W, Schild HH (2007). "MRI for diagnosis of pure ductal carcinoma in situ: a prospective observational study". The Lancet. 370 (9586): 485–492. PMID.
- ↑ Boetes C, Mann RM (2007). "Ductal carcinoma in situ and breast MRI". The Lancet. 370 (9586): 459–460. PMID.
- ↑ Saslow D, Boetes C, Burke W, Harms S, Leach MO, Lehman CD, Morris E, Pisano E, Schnall M, Sener S, Smith RA, Warner E, Yaffe M, Andrews KS, Russell CA (2007). "American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography". CA: a Cancer Journal for Clinicians. 57 (2): 75–89. PMID 17392385.
|access-date=requires|url=(help) - ↑ Thomas DB, Gao DL, Ray RM; et al. (2002). "Randomized trial of breast self-examination in Shanghai: final results". J. Natl. Cancer Inst. 94 (19): 1445–57. PMID 12359854.
- ↑ Harris R, Kinsinger LS (2002). "Routinely teaching breast self-examination is dead. What does this mean?". J. Natl. Cancer Inst. 94 (19): 1420–1. PMID 12359843.
- ↑ 22.0 22.1 Moyer VA (2013). "Risk Assessment, Genetic Counseling, and Genetic Testing for BRCA-Related Cancer in Women: U.S. Preventive Services Task Force Recommendation Statement". Ann Intern Med. doi:10.7326/M13-2747. PMID 24366376.
- CS1 maint: Multiple names: authors list
- Pages using citations with accessdate and no URL
- CS1 errors: dates
- CS1 maint: Explicit use of et al.
- All articles with unsourced statements
- Articles with unsourced statements from September 2007
- Articles with invalid date parameter in template
- Disease
- Types of cancer
- Breast
- Hereditary cancers
- Oncology
- Mature chapter