Asthma pathophysiology
|
Asthma Microchapters |
|
Diagnosis |
|---|
|
Other Diagnostic Studies |
|
Treatment |
|
Case Studies |
|
Asthma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Asthma pathophysiology |
|
Risk calculators and risk factors for Asthma pathophysiology |
Editor(s)-in-Chief: C. Michael Gibson, M.S., M.D. [1] Phone:617-632-7753; Philip Marcus, M.D., M.P.H. [2]
Overview
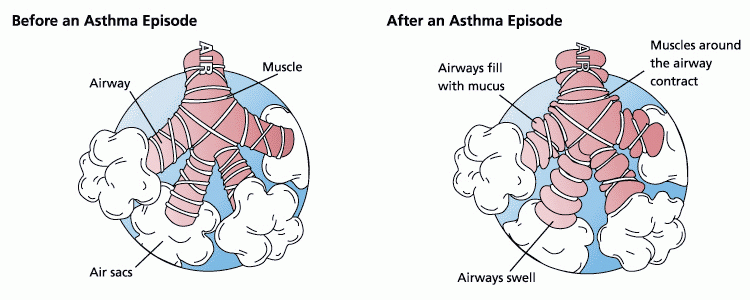
Asthma is the result of an immune response in the bronchial airways.[1]. During an asthma episode, inflamed airways react to the introduction of environmental triggers, such as smoke, dust, or pollen. The airways narrow and produce excess mucus, making it difficult to breathe.
The airways of asthmatics are "hypersensitive" to certain triggers, also known as stimuli. In response to exposure to these triggers, the bronchi (large airways) contract into spasm (an "asthma attack"). Inflammation mediated by TH2 cells induced humoral immune reaction soon follows leading to a further narrowing of the airways and excessive mucus production, this can lead to coughing and dyspnea.
Pathophysiology
Bronchoconstriction
Asthma is the result of an immune response in the bronchial airways.[1]. During an asthma episode, inflamed airways react to the introduction of environmental triggers, such as smoke, dust, or pollen. The airways narrow and produce excess mucus, making it difficult to breathe.
The airways of asthmatics are "hypersensitive" to certain triggers, also known as stimuli. In response to exposure to these triggers, the bronchi (large airways) contract into spasm (an "asthma attack"). Inflammation soon follows leading to a further narrowing of the airways and excessive mucus production, this can lead to coughing and other breathing difficulties.
Stimuli
- Allergenic air pollution, which include waste from common household pests, such as the house dust mite and cockroach, grass pollen, mould spores, and pet epithelial cells. These are typically inhaled and the body's introduction to the stimuli occurs through the respiratory system.
- Indoor allergenic air pollution from volatile organic compounds (VCOs). This including perfumes and perfumed products. Potential VCOs include: soap, dishwashing liquid, laundry detergent, fabric softener, paper tissues, paper towels, toilet paper, shampoo, hairspray, hair gel, cosmetics, facial cream, sun cream, deodorant, cologne, shaving cream, aftershave lotion, air freshener and candles, and products such as oil-based paint.
- Medications, such as aspirin,[2] β-adrenergic antagonists (beta blockers), and penicillin.
- Allergic to food such as milk, peanuts, and eggs. However, asthma is rarely the only symptom, and not all people with food or other allergies have asthma.
- Use of fossil fuel related allergenic air pollution, such as ozone, smog, summer smog, nitrogen dioxide, and sulfur dioxide. This is thought to be one of the major reasons for the high prevalence of asthma in urban areas.
- Various industrial compounds and other chemicals, notably sulfites; chlorinated swimming pools generate chloramines—monochloramine (NH2Cl), dichloramine (NHCl2) and trichloramine (NCl3)—in the air around them, which are known to induce asthma.[3]
- Early childhood infections, especially viral respiratory infections. However, persons of any age can have asthma triggered by colds and other respiratory infections even though their normal stimuli might be from another category (e.g. pollen) and absent at the time of infection. 80% of asthma attacks in adults and 60% in children are caused by respiratory viruses.
- Exercise, the effects of which differ somewhat from those of the other triggers.
- Allergenic indoor air pollution, in some countries, from newsprint & other literature such as, direct marketing/junk mail leaflets & glossy magazines.
- Hormonal changes in adolescent girls and adult women associated with the menstrual cycle can lead to a worsening of asthma. The influence of hormones can be largely varied from person to person. Some women also experience a worsening of their asthma during pregnancy, whereas others find no significant changes, and in other women their asthma improves during their pregnancy.
- Emotional stress, the influence of this trigger is not well understood.
- Cold weather can adversely affect breathing in asthmatics.
Bronchial inflammation
In both asthmatics and non-asthmatics, inhaled allergens that find their way to the inner airways are ingested by antigen presenting cells, or APCs. APCs then present pieces of the allergen to other cells of immune system. In most people, these other immune cells (TH0 cells) usually ignore the allergen molecules. In asthmatics, however, these cells differentiate into TH2, for reasons that are not well understood. The resultant TH2 cells activate an important arm of the immune system, known as the humoral immune system. The humoral immune system produces antibodies against the inhaled allergen. Later, when an asthmatic inhales the same allergen, these antibodies recognize it and activate a humoral response. This results in inflammatory response where chemicals are produced that cause the airways to constrict and release more mucus, and the cell-mediated arm of the immune system is activated. The inflammatory response is responsible for the clinical manifestations of an asthma attack. The following section describes this complex series of events in more detail.
Pathogenesis
- The fundamental problem in asthma appears to be immunological. Young children in the early stages of asthma show signs of excessive inflammation in their airways.
- Epidemiological findings give clues as to the pathogenesis. The incidence of asthma seems to be increasing worldwide, and asthma is now very much more common in affluent countries.
- In 1968 Andor Szentivanyi first described The Beta Adrenergic Theory of Asthma; in which blockage of the Beta-2 receptors of pulmonary smooth muscle cells causes asthma.[4]
- In 1995 Szentivanyi and colleagues demonstrated that IgE blocks beta-2 receptors.[5]
Since overproduction of IgE is central to all atopic diseases, this was a watershed moment in the world of allergy.[6]
- Many studies have linked asthma, bronchitis, and acute respiratory illnesses to air quality experienced by children.[7]
- This study showed that children in the high ozone communities who played three or more sports developed asthma at a rate three times higher than those in the low ozone communities. Because participation in some sports can result in a child drawing up to 17 times the normal amount of air into the lungs, young athletes are more likely to develop asthma.
- Another theory of pathogenesis is that asthma is a disease of hygiene. In nature, children are exposed to bacteria and other antigens soon after birth, switching on the TH1 lymphocyte cells of the immune system that deal with bacterial infection. If this stimulus is insufficient, as it may be in modern, clean environments, then TH2 cells predominate, and asthma and other allergic diseases may develop. This hygiene hypothesis may explain the increase in asthma in affluent populations. The TH2 lymphocytes and eosinophil cells that protect us against parasites and other infectious agents are the same cells responsible for the allergic reaction. Charcot-Leyden crystals are formed when crystalline material in eosinophils coalesce. These crystals are significant in sputum samples of people with asthma. In the developed world, the parasites that eosinophils are programmed to combat are now rarely encountered, but the immune response remains and is wrongly triggered in some individuals by certain allergens.
It has been postulated that some forms of asthma may be related to infection, particularly to Chlamydia pneumoniae.[8] This issue remains controversial, as the relationship is not borne out by meta-analysis of the research.[9] The correlation seems to be not with the onset, but rather with accelerated loss of lung function in adults with new onset of non-atopic asthma.[10] One possible explanation is that some asthmatics may have altered immune response that facilitates long-term chlamydia pneumonia infection.[11] The response to targeting with macrolide antibiotics has been investigated, but the temporary benefit reported in some studies may reflect just their anti-inflammatory activities rather than their antimicrobic action.[9]
A study conducted by the National Jewish Medical and Research Center concluded that factors such as being overweight and or obese were associated with a dose-dependent increase in the odds of incident asthma in men and women. This demonstrates that asthma incidence could be reduced by interventions targeting overweight and obese populations. [12]
References
- ↑ 1.0 1.1 Maddox L, Schwartz DA. The Pathophysiology of Asthma. Annu. Rev. Med. 2002, 53:477-98. PMID 11818486
- ↑ Jenkins C, Costello J, Hodge L. Systematic review of prevalence of aspirin induced asthma and its implications for clinical practice. BMJ 2004;328:434. PMID 14976098
- ↑ Nemery B, Hoet PH, Nowak D. Indoor swimming pools, water chlorination and respiratory health. Eur Respir J. 2002;19(5):790-3. PMID 12030714
- ↑ Szentivanyi, Andor (1968). "The Beta Adrenergic Theory of the Atopic Abnormality in Asthma". Unknown parameter
|jounal=ignored (help) - ↑ Szentivanyi A., Ali K., Calderon EG., Brooks SM., Coffey RG., Lockey RF. (1993). "The in vitro effect of Imunnoglobulin E {IgE} on cyclic AMP concentrations in A549 human pulmonary epithelial cells with or without beta adrenergic stimulation". J. Allergy Clin Immunol. 91: 379. - Part of Abstracts from:
"50th Anniversary of the American Academy of Allergy and Immunology. 49th Annual Meeting. Chicago, Illinois, March 12–17, 1993. Abstracts". J Allergy Clin Immunol. 91 (1 Pt 2): 141–379. 1993. PMID 8421135. - ↑ Kowalak JP, Hughes AS et al (eds), ed. (2001). Professional Guide To Diseases (7th ed. ed.). Springhouse.
- ↑ "Asthma and Air Quality".
- ↑ Terttu HH, Leinonen M, Nokso-Koivisto J, Korhonen T, Raty R, He Q, Hovi T, Mertsola J, Bloigu A, Rytila P, Saikku P (2006). "Non-random distribution of pathogenic bacteria and viruses in induced sputum or pharyngeal secretions of adults with stable asthma". Thorax. PMID 16517571.
- ↑ 9.0 9.1 Richeldi L, Ferrara G, Fabbri LM, Lasserson TJ, Gibson PG (2005). "Macrolides for chronic asthma". Cochrane Database Syst Rev (4): CD002997. PMID 16235309.
- ↑ Pasternack R, Huhtala H, Karjalainen J (2005). "Chlamydophila (Chlamydia) pneumoniae serology and asthma in adults: a longitudinal analysis". J Allergy Clin Immunol. 116 (5): 1123–8. PMID 16275386.
- ↑ Ronchetti R, Biscione GL, Ronchetti F, Ronchetti MP, Martella S, Falasca C, Casini C, Barreto M, Villa MP (2005). "Why Chlamydia pneumoniae is associated with asthma and other chronic conditions? Suggestions from a survey in unselected 9 years old schoolchildren". Pediatr Allergy Immunol. 16 (2): 145–50. PMID 15787872.
- ↑ journal=American Journal of Respiratory and Critical Care Medicine | volume=175 |pages=661-666 | year=2007 |