Asthma pathophysiology
|
Asthma Microchapters |
|
Diagnosis |
|---|
|
Other Diagnostic Studies |
|
Treatment |
|
Case Studies |
|
Asthma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Asthma pathophysiology |
|
Risk calculators and risk factors for Asthma pathophysiology |
Editor(s)-in-Chief: C. Michael Gibson, M.S., M.D. [1] Phone:617-632-7753; Philip Marcus, M.D., M.P.H. [2]
Pathophysiology
Bronchoconstriction
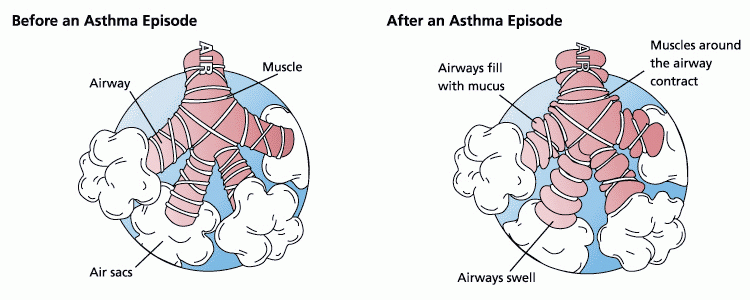
During an asthma episode, inflamed airways react to environmental triggers such as smoke, dust, or pollen. The airways narrow and produce excess mucus, making it difficult to breathe. In essence, asthma is the result of an immune response in the bronchial airways.[1]
The airways of asthmatics are "hypersensitive" to certain triggers, also known as stimuli (see below). In response to exposure to these triggers, the bronchi (large airways) contract into spasm (an "asthma attack"). Inflammation soon follows, leading to a further narrowing of the airways and excessive mucus production, which leads to coughing and other breathing difficulties.
Stimuli
- Allergenic air pollution, from nature, typically inhaled, which include waste from common household pests, such as the house dust mite and cockroach, grass pollen, mould spores, and pet epithelial cells;
- Indoor allergenic air pollution from volatile organic compounds, including perfumes and perfumed products. Examples include soap, dishwashing liquid, laundry detergent, fabric softener, paper tissues, paper towels, toilet paper, shampoo, hairspray, hair gel, cosmetics, facial cream, sun cream, deodorant, cologne, shaving cream, aftershave lotion, air freshener and candles, and products such as oil-based paint.
- Medications, including aspirin,[2] β-adrenergic antagonists (beta blockers), and penicillin.
- Food allergies such as milk, peanuts, and eggs. However, asthma is rarely the only symptom, and not all people with food or other allergies have asthma.
- Use of fossil fuel related allergenic air pollution, such as ozone, smog, summer smog, nitrogen dioxide, and sulfur dioxide, which is thought to be one of the major reasons for the high prevalence of asthma in urban areas;
- Various industrial compounds and other chemicals, notably sulfites; chlorinated swimming pools generate chloramines—monochloramine (NH2Cl), dichloramine (NHCl2) and trichloramine (NCl3)—in the air around them, which are known to induce asthma.[3]
- Early childhood infections, especially viral respiratory infections. However, persons of any age can have asthma triggered by colds and other respiratory infections even though their normal stimuli might be from another category (e.g. pollen) and absent at the time of infection. 80% of asthma attacks in adults and 60% in children are caused by respiratory viruses.
- Exercise, the effects of which differ somewhat from those of the other triggers;
- Allergenic indoor air pollution from newsprint & other literature such as, Direct marketing / junk mail leaflets & glossy magazines (in some countries).
- Hormonal changes in adolescent girls and adult women associated with their menstrual cycle can lead to a worsening of asthma. Some women also experience a worsening of their asthma during pregnancy whereas others find no significant changes, and in other women their asthma improves during their pregnancy.
- Emotional stress which is poorly understood as a trigger.
- Cold weather can adversely affect breathing in asthmatics.[4]
Bronchial inflammation
The mechanisms behind allergic asthma—i.e., asthma resulting from an immune response to inhaled allergens—are the best understood of the causal factors. In both asthmatics and non-asthmatics, inhaled allergens that find their way to the inner airways are ingested by a type of cell known as antigen presenting cells, or APCs. APCs then "present" pieces of the allergen to other immune system cells. In most people, these other immune cells (TH0 cells) "check" and usually ignore the allergen molecules. In asthmatics, however, these cells transform into a different type of cell (TH2), for reasons that are not well understood. The resultant TH2 cells activate an important arm of the immune system, known as the humoral immune system. The humoral immune system produces antibodies against the inhaled allergen. Later, when an asthmatic inhales the same allergen, these antibodies "recognize" it and activate a humoral response. Inflammation results: chemicals are produced that cause the airways to constrict and release more mucus, and the cell-mediated arm of the immune system is activated. The inflammatory response is responsible for the clinical manifestations of an asthma attack. The following section describes this complex series of events in more detail.
Pathogenesis
The fundamental problem in asthma appears to be immunological: young children in the early stages of asthma show signs of excessive inflammation in their airways. Epidemiological findings give clues as to the pathogenesis: the incidence of asthma seems to be increasing worldwide, and asthma is now very much more common in affluent countries.
In 1968 Andor Szentivanyi first described The Beta Adrenergic Theory of Asthma; in which blockage of the Beta-2 receptors of pulmonary smooth muscle cells causes asthma.[5] Szentivanyi's Beta Adrenergic Theory is a citation classic[6] and has been cited more times than any other article in the history of the Journal of Allergy.
In 1995 Szentivanyi and colleagues demonstrated that IgE blocks beta-2 receptors.[7] Since overproduction of IgE is central to all atopic diseases, this was a watershed moment in the world of allergy.[8]
The Beta-Adrenergic Theory has been cited in the scholarship of such noted investigators as Richard F. Lockey (former President of the American Academy of Allergy, Asthma, and Immunology),[9] Charles Reed (Chief of Allergy at Mayo Medical School),[10] and Craig Venter (Human Genome Project).[11]
Many studies have linked asthma, bronchitis, and acute respiratory illnesses to air quality experienced by children.[12] One of the largest of these studies is the California Children's Health Study.[13] From the press release [3]
This study showed that children in the high ozone communities who played three or more sports developed asthma at a rate three times higher than those in the low ozone communities. Because participation in some sports can result in a child drawing up to 17 times the “normal” amount of air into the lungs, young athletes are more likely to develop asthma.
Note that concentrations of ozone have risen steadily in Europe since 1870. [4]
Another theory of pathogenesis is that asthma is a disease of hygiene. In nature, babies are exposed to bacteria and other antigens soon after birth, "switching on" the TH1 lymphocyte cells of the immune system that deal with bacterial infection. If this stimulus is insufficient, as it may be in modern, clean environments, then TH2 cells predominate, and asthma and other allergic diseases may develop. This "hygiene hypothesis" may explain the increase in asthma in affluent populations. The TH2 lymphocytes and eosinophil cells that protect us against parasites and other infectious agents are the same cells responsible for the allergic reaction. Charcot-Leyden crystals are formed when crystalline material in eosinophils coalesce. These crystals are significant in sputum samples of people with asthma. In the developed world, the parasites that eosinophils are programmed to combat are now rarely encountered, but the immune response remains and is wrongly triggered in some individuals by certain allergens.
It has been postulated that some forms of asthma may be related to infection, in particular by Chlamydia pneumoniae.[14] This issue remains controversial, as the relationship is not borne out by meta-analysis of the research.[15] The correlation seems to be not with the onset, but rather with accelerated loss of lung function in adults with new onset of non-atopic asthma.[16] One possible explanation is that some asthmatics may have altered immune response that facilitates long-term chlamydia pneumonia infection.[17] The response to targeting with macrolide antibiotics has been investigated, but the temporary benefit reported in some studies may reflect just their anti-inflammatory activities rather than their antimicrobic action.[15]
One group of researchers suggested that, in part, asthma has a neurogenic paroxysmal component,[18] and that several anti-eleptic drugs have an effect. However only one paper[19] has been published as listed by PubMed and its conclusions criticized.[20]
A study conducted by the National Jewish Medical and Research Center concluded that overweight and obesity are associated with a dose-dependent increase in the odds of incident asthma in men and women, suggesting asthma incidence could be reduced by interventions targeting overweight and obesity. [21]
References
- ↑ Maddox L, Schwartz DA. The Pathophysiology of Asthma. Annu. Rev. Med. 2002, 53:477-98. PMID 11818486
- ↑ Jenkins C, Costello J, Hodge L. Systematic review of prevalence of aspirin induced asthma and its implications for clinical practice. BMJ 2004;328:434. PMID 14976098
- ↑ Nemery B, Hoet PH, Nowak D. Indoor swimming pools, water chlorination and respiratory health. Eur Respir J. 2002;19(5):790-3. PMID 12030714
- ↑ about.com article
- ↑ Szentivanyi, Andor (1968). "The Beta Adrenergic Theory of the Atopic Abnormality in Asthma". Unknown parameter
|jounal=ignored (help) - ↑ Lockey, Richard, In lasting tribute: Andor Szentivanyi, MD. J. Allergy and Clinical Immunology, January, 2006
- ↑ Szentivanyi A., Ali K., Calderon EG., Brooks SM., Coffey RG., Lockey RF. (1993). "The in vitro effect of Imunnoglobulin E {IgE} on cyclic AMP concentrations in A549 human pulmonary epithelial cells with or without beta adrenergic stimulation". J. Allergy Clin Immunol. 91: 379. - Part of Abstracts from:
"50th Anniversary of the American Academy of Allergy and Immunology. 49th Annual Meeting. Chicago, Illinois, March 12–17, 1993. Abstracts". J Allergy Clin Immunol. 91 (1 Pt 2): 141–379. 1993. PMID 8421135. - ↑ Kowalak JP, Hughes AS et al (eds), ed. (2001). Professional Guide To Diseases (7th ed. ed.). Springhouse.
- ↑ Lockey, Richard F. "Anaphylaxis: Synopsis". Allergic Diseases Resource Center. World Allergy Organization. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Unknown parameter|accessmonthday=ignored (help) - ↑ Ouellette, J. J. (1967). "The effect of partial beta adrenergic blockade on the bronchial response of hay fever subjects to ragweed aerosol". Journal of Allergy. 39 (3): 160–6. PMID 5227155. Unknown parameter
|coauthors=ignored (help); Unknown parameter|month=ignored (help) - ↑ Fraser, Claire M. (May 14, 1980). "The synthesis of beta-adrenergic receptors in cultured human lung cells: induction by glucocorticoids" (PDF). Biochemical and Biophysical Research Communications. 94 (1): 390–397. doi:10.1016/S0006-291X(80)80233-6. PMID 6248064. Unknown parameter
|coauthors=ignored (help) - ↑ "Asthma and Air Quality".
- ↑ "California Children's Health Study".
- ↑ Terttu HH, Leinonen M, Nokso-Koivisto J, Korhonen T, Raty R, He Q, Hovi T, Mertsola J, Bloigu A, Rytila P, Saikku P (2006). "Non-random distribution of pathogenic bacteria and viruses in induced sputum or pharyngeal secretions of adults with stable asthma". Thorax. PMID 16517571.
- ↑ 15.0 15.1 Richeldi L, Ferrara G, Fabbri LM, Lasserson TJ, Gibson PG (2005). "Macrolides for chronic asthma". Cochrane Database Syst Rev (4): CD002997. PMID 16235309.
- ↑ Pasternack R, Huhtala H, Karjalainen J (2005). "Chlamydophila (Chlamydia) pneumoniae serology and asthma in adults: a longitudinal analysis". J Allergy Clin Immunol. 116 (5): 1123–8. PMID 16275386.
- ↑ Ronchetti R, Biscione GL, Ronchetti F, Ronchetti MP, Martella S, Falasca C, Casini C, Barreto M, Villa MP (2005). "Why Chlamydia pneumoniae is associated with asthma and other chronic conditions? Suggestions from a survey in unselected 9 years old schoolchildren". Pediatr Allergy Immunol. 16 (2): 145–50. PMID 15787872.
- ↑ Lomia M (March 20, 2006). "Bronchial asthma as neurogenic paroxysmal and inflammatory disease -- Scientific background of effective use of anticonvulsants for pharmacotherapy of bronchial asthma".
- ↑ Lomia M, Tchelidze T, Pruidze M (2006). "Bronchial asthma as neurogenic paroxysmal inflammatory disease: a randomized trial with carbamazepine". Respiratory medicine. 100 (11): 1988–96. doi:10.1016/j.rmed.2006.02.018. PMID 16597501.
- ↑ Singh N (2007). "Carbamazepine in asthma: first do no harm!". Respiratory medicine. 101 (3): 676, author reply 677-8. doi:10.1016/j.rmed.2006.11.025. PMID 17223330.
Related warnings:- Lee T, Cochrane GM, Amlot P (1981). "Pulmonary eosinophilia and asthma associated with carbamazepine" (Scanned image). British medical journal (Clinical research ed.). 282 (6262): 440. PMID 6780065.
- Lewis IJ, Rosenbloom L (1982). "Glandular fever-like syndrome, pulmonary eosinophilia and asthma associated with carbamazepine". Postgraduate medical journal. 58 (676): 100–1. PMID 7100019.
- ↑ journal=American Journal of Respiratory and Critical Care Medicine | volume=175 |pages=661-666 | year=2007 |