Androgen insensitivity syndrome pathophysiology
|
Androgen insensitivity syndrome Microchapters |
|
Differentiating Androgen insensitivity syndrome from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Androgen insensitivity syndrome pathophysiology On the Web |
|
American Roentgen Ray Society Images of Androgen insensitivity syndrome pathophysiology |
|
Directions to Hospitals Treating Androgen insensitivity syndrome |
|
Risk calculators and risk factors for Androgen insensitivity syndrome pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Pathophysiology
Normal function of androgens and the androgen receptor [2]
Understanding the effects of androgen insensitivity begins with an understanding of the normal effects of testosterone in male and female development. The principal mammalian androgens are testosterone and its more potent metabolite, dihydrotestosterone (DHT).
The androgen receptor (AR) is a large protein of at least 910 amino acids. Each molecule consists of a portion which binds the androgen, a zinc finger portion that binds to DNA in steroid sensitive areas of nuclear chromatin, and an area that controls transcription.
Testosterone diffuses from the circulation into the cytoplasm of a target cell. Some is metabolized to estradiol, some reduced to DHT, and some remains as testosterone (T). Both T and DHT can bind and activate the androgen receptor, though DHT does so with more potent and prolonged effect. As DHT (or T) binds to the receptor, a portion of the protein is cleaved. The AR-DHT combination dimerizes by combining with a second AR-DHT, both are phosphorylated, and the entire complex moves into the cell nucleus and binds to androgen response elements on the promoter region of androgen-sensitive target genes. The transcription effect is amplified or inhibited by coactivators or corepressors.
Although testosterone can be produced directly and indirectly from ovaries and adrenals later in life, the primary source of testosterone in early fetal life is the testes, and it plays a major role in human sexual differentiation. Before birth, testosterone induces the primary sex characteristics of males. At puberty, testosterone is primarily responsible for the secondary sex characteristics of males.
- See Testosterone article for fuller discussion of androgen sources and the role of testosterone in normal human development.
- See Sexual differentiation for a brief but fuller overview of human sexual differentiation and biological sex differences.
Prenatal effects of testosterone in 46,XY fetus
In a normal fetus with a 46,XY karyotype, the presence of the SRY gene induces testes to form on the genital ridges in the fetal abdomen a few weeks after conception. By 6 weeks of gestation, genital anatomies of XY and XX fetuses are still indistinguishable, consisting of a tiny underdeveloped button of tissue able to become a phallus, and a urogenital midline opening flanked by folds of skin able to become either labia or scrotum. By the 7th week, fetal testes begin to produce testosterone and release it into the blood.
Directly and as DHT, testosterone acts on the skin and tissues of the genital area and by 12 weeks of gestation, has produced a recognizable male, with a growing penis with a urethral opening at the tip, and a perineum fused and thinned into a scrotum, ready for the testes. Evidence suggests that this "remodelling" of the genitalia can only occur during this period of fetal life; if not complete by about 13 weeks, no amount of testosterone later will move the urethral opening or close a vagina-like opening.
For the remainder of gestation, the principal known effect of testosterone and DHT is continued growth of the penis and internal wolffian derivatives (part of prostate, epididymis, seminal vesicles, and vas deferens).
Early postnatal effects of testosterone in 46,XY infants
Testosterone levels are low at birth but rise within weeks, remaining at normal male pubertal levels for about 2 months before declining to the low, barely detectable childhood levels. The biological function of this rise is unknown. Animal research suggests a contribution to brain differentiation.
Pubertal effects of testosterone in 46,XY children
At puberty, many of the early physical changes in both sexes are androgenic (adult-type body odor, increased oiliness of skin and hair, acne, pubic hair, axillary hair, fine upper lip and sideburn hair).
As puberty progresses, later secondary sex characteristics in males are nearly entirely due to androgens (continued growth of the penis, maturation of spermatogenic tissue and fertility, beard, deeper voice, masculine jaw and musculature, body hair, heavier bones). In males, the major pubertal changes attributable to estradiol are growth acceleration, epiphyseal closure, termination of growth, and (if it occurs) gynecomastia.
Genetics
Because the Androgen Insensitivity Syndrome gives rise to ambiguity between the genetic and the phenotypic gender, we will use the convention 46,XY to designate a genotypic male, and 46,XX to designate a genotypic female. By this convention, a person with Androgen Insensitivity Syndrome is a 46,XY but a phenotypic female.
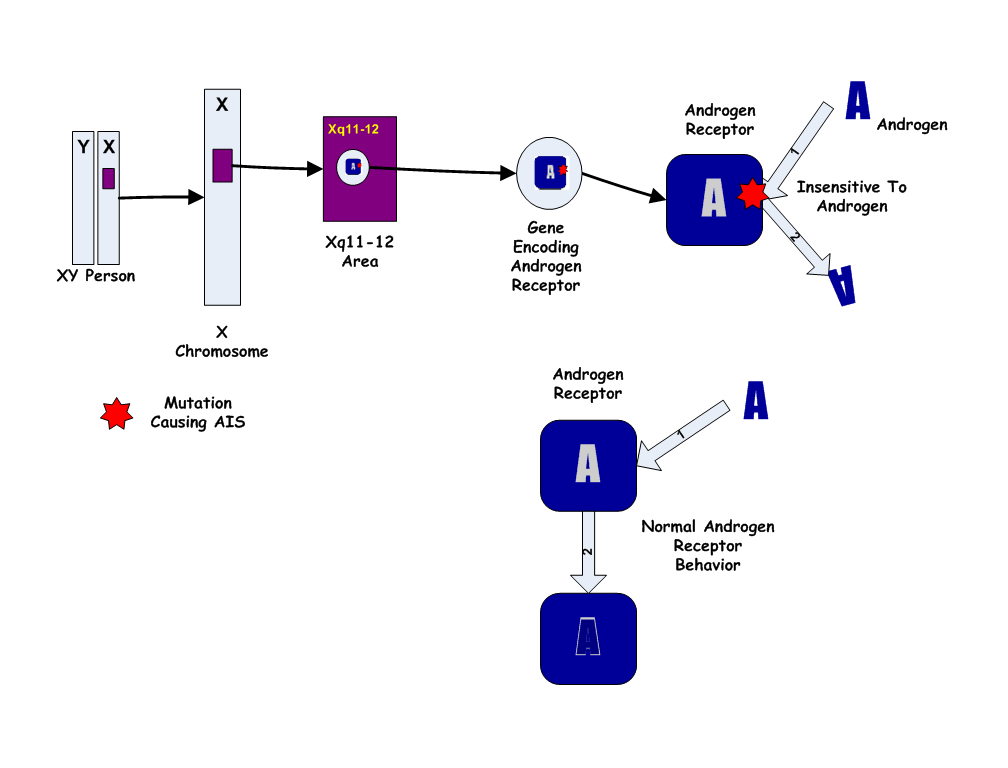
The Androgen Insensitivity Syndrome has been linked to mutations in AR, the gene for the human Androgen Receptor, located at Xq11-12 (i.e. on the X chromosome). Thus, it is an X-linked recessive trait, causing minimal or no effects in 46,XX people.

However, 46,XX women with a single mutated copy of the AR gene can be "carriers" of AIS, and their 46,XY children (male) will have a 50% chance of having the syndrome. As in some other X-linked recessive conditions, carrier mothers may display some minor traits of the condition: AIS carriers often have reduced axillary and pubic hair, and reduced normal adolescent acne.
Except in the rare instance of a new mutation, a person affected with AIS has inherited his/her single X chromosome with the defective gene from his/her mother, who may have an affected sibling. Generally the condition caused by a familial mutation will affect family members similarly, though differing degrees of severity occasionally occur in different relatives with apparently the same mutation. Carrier testing is now available for relatives at risk when a diagnosis of AIS is made in a family member.
Over 100 AR mutations causing various forms of AIS have been reported. In general, the milder types of AIS (4 and 5 in the list below) are caused by simple missense mutations with single codon/single amino acid difference, while CAIS and the nearly complete forms result from mutations that more severely affect the shape and structure of the protein. About one third of cases of AIS are new mutations rather than familial. A single case of CAIS attributed to an abnormality of the AF-1 coactivator (rather than AR itself) has been reported (OMIM 300274).